Fig. 2.1
Amoebic colonitis complicated by ulcerative colonitis. (a–c) Contrast CT scanning demonstrates diffuse thickening of the sigmoid colon wall and rectal wall as well as high density of abscess wall. (d) Colonoscopy demonstrates chronic inflammation of mucosa at the sigmoid colon and rectum
(Note: the case and the figures were provided by Tang, YH. from Ruijin Hospital, Shanghai, China)
2.7.2.2 Amebic Liver Abscess
The radiological demonstrations vary at different stages of the disease. Typical liver abscess is demonstrated at the formation period of liver abscess, while atypical liver abscess is demonstrated at the suppurative inflammation period and early stage of the abscess formation. The atypical radiological demonstrations can be hardly differentiated from neoplasms. Therefore, at such stages, it tends to be misdiagnosed.
Ultrasound
Typical Liver Abscess
Singular or multiple hypoechoic or anechoic mass is demonstrated. The abscess wall is demonstrated with strong echo and varied thickness. The outer wall is smooth, while the inner wall, irregular. Circular echo of edema is demonstrated that changes gradually from bright to dark around the abscess. The anechoic abscess cavity, strong echoic abscess wall, and hypoechoic surrounding edema form the ring-in-ring sign. In the cases with gas in the abscess, narrow and long strip of strong echo is demonstrated posterior to the lesion.
Atypical Liver Abscess
The liver is demonstrated with heterogeneous liquid dark area, which is well defined from the surrounding liver tissue. By ultrasound-guided liver puncture, typical fruit jam-colored pus with no unfavorable odor can be collected, which is of great diagnostic value.
Case Study 2
An adult male patient had a history of contact to patients with amebic dysentery in an epidemic area. By serological test, amoeba was detected positive.
(For case detail and figures, please refer to Blessmann, J, et al. Trop Med Int Health, 2006, 11 (4): 504.)
Case Study 3
A male patient aged 38 years experienced right upper quadrant abdominal pain, hepatosplenomegaly, and a small quantity of ascites. The bacterial culture was negative. By microscopy, amebic trophozoite was detected.
(For case detail and figures, please refer to Mandal SK, et al. World J Gastroenterol, 2006, 12 (25): 4109.)
CT Scanning
Typical Liver Abscess
Plain CT scanning demonstrates the abscess cavity as round or round-like low-density area. The abscess wall is demonstrated as a ring-shaped strip with slightly higher density than abscess cavity but lower density than normal liver tissue. Contrast CT scanning demonstrates obvious ring-shaped enhancement of the abscess wall and no enhancement of the abscess cavity and surrounding edema. The lesion is demonstrated as a ring-shaped target sign, which may be singular ring, double rings, and triple rings. The singular ring shows the abscess wall, without obvious surrounding edema. Double ring sign shows the abscess wall by the middle space and inner ring and surrounding edema by the outer ring (Fig. 2.2). The triple ring sign shows, from inner ring outwards, a ring with inflammatory tissue, fibrous granulation tissue, and edema as well as the other two rings of the abscess wall. The external ring is a fibrous granulation tissue, with obvious enhancement by contrast scanning. The inner ring is an inflammatory necrotic tissue, with less obvious enhancement by contrast scanning.
Atypical Liver Abscess
By plain CT scanning, the demonstrations are not characteristic, with evenly low or equal and low mixed-density shadow in the liver and poorly defined lesion boundary that is partially clear but not sharp. Contrast CT scanning demonstrates internal structure and the blood supply of the lesion, which are categorized into five typical signs:
Abscess Shrinkage Sign
It is manifested as slight to moderate enhancement of the lesion at the delayed phase. The lesion is demonstrated with equal density change like surrounding liver parenchyma. Edema strip surrounding the abscess is absent at the portal vein phase. The lesions are demonstrated to be smaller than that by plain CT scanning, or even cannot demonstrated, suggesting purulent inflammatory stage of the abscess or inflammatory response after incomplete liquefaction of abscess in liver tissue.
Peripheral Congestion Sign
By contrast scanning, the liver tissue surrounding the abscess is demonstrated with high perfusion and transient obvious enhancement at the arterial phase. The enhancement of the liver tissue is wedge shaped or in large flake, with the range confined within the liver tissue surrounding abscess or hepatic segment of the abscess. The enchantment rapidly fades away. Until the portal vein phase and early parenchyma phase, the enhancement of the surrounding liver tissue is not obvious. The detection rate of such a sign is up to 75 %. The sign is caused by decreased blood flow in the portal vein and compensatorily increased blood flow in the hepatic artery due to stenosis of the intrahepatic portal vein arising from inflammation of the portal area.
Cluster-Like Sign
Multiple tiny abscesses (<2 cm) gather into mass or fuse together, with honeycomb-like enhancement.
Petallike Sign
Petallike sign is found in the cases with multilocular abscess. Inflammatory responses can be demonstrated at the residual locular septum in the abscesses, with relatively obvious enchantment. Several adjacent septa in combination are demonstrated in a petallike sign, with mixed low-density area of less obvious enhancement.
Delayed Enhancement Sign
Long-term persistence of abscess enchantment, the lesion density being relatively higher or equal to liver parenchyma with poorly defined boundary, and shrinkage of the lesion suggest the purulent inflammation stage or proliferative reactions after destructions by purulent inflammation.
Inflammatory edema around the abscess wall and alive liver tissue with equal density enhancement are caused by capillary inflammatory congestion at the inflammatory granulation tissue of the abscess wall and its consequent increase of permeability. Therefore, slow exosmose and slow discharge of contrast agent occur.
Case Study 4
A male patient aged 31 years experienced fever and diarrhea with jam-colored stool with no known causes, tenesmus, and dull pain at the right upper quadrant. Amebic serum antibody IgM was positive.
Fig. 2.2
Amoebic liver abscess. (a–c) CT scanning demonstrates the lesion at the right posterior inferior liver lobe with quite well-defined boundary, central low density of the abscess, and no enhancement at the artery phase, portal vein phase, and delayed phase. The abscess wall is demonstrated to be smooth with ring-shaped enhancement, which is surrounded by low-density edema strip
(Note: the case and the figures were proved by Tang, YH. from Ruijin Hospital, Shanghai, China.)
Case Study 5
An adult male experienced fever, jaundice, and abdominal pain. Amebic trophozoite was detected by microscopy.
A. Ultrasound demonstrates abscess at the right liver lobe.
B. Contrast CT scanning demonstrates abscess at the right liver lobe with inner gas density shadow during the venous phase and involved right hepatic vein.
(For case detail and figures, please refer to Singh V, et al. Am J Trop Med Hyg, 2008, 78 (4): 556.)
Case Study 6
A male patient aged 29 years complained of right upper quadrant pain and high fever 5 years ago. Amebic trophozoite was detected by microscopy.
Case Study 7
A female patient aged 43 years experienced fever, chills, epigastric pain, nausea, and vomiting. She was diagnosed with amebic liver abscess.
(For case detail and figures, please refer to Kim TY, et al. Korean J Parasitol, 2010, 48 (2): 157.)
Case Study 8
A male patient aged 37 years experienced fever and right upper quadrant pain. Enzyme-linked immunosorbent assay demonstrated positive amoeba antibody.
(For case detail and figures, please refer to Miller Q, et al. Curr Surg, 2000, 57 (5): 476.)
Case Study 9
A male patient aged 57 years complained of fever, poor appetite, and right abdominal pain for 15 days, which was persistent dull pain. Enzyme-linked immunosorbent assay was positive, with IgG 1:1,600.
(For case detail and figures, please refer to Sodhi KS, et al. J EmerG Med, 2008, 34 (2): 155.)
Case Study 10
Two patients with amebic dysentery came from an epidemic area. Their diagnosis was amebic liver abscess.
(For case detail and figures, please refer to Mortele KJ, et al. Radiographics, 2004, 24 (4): 937.)
MR Imaging
Typical Liver Abscess
Plain MR imaging demonstrates the abscess cavity with long T1 and long T2 signal. The signal of the abscess wall is slightly higher than the abscess cavity but is lower than a normal liver tissue. The edema surrounding the abscess is demonstrated with slightly low T1WI signal and slightly high T2WI signal, namely, the halo sign. Contrast MR imaging demonstrates ring-shaped enhancement of the abscess with even thickness, but no enhancement of the abscess cavity.
Atypical Liver Abscess
Plain MR imaging demonstrates the lesion with equal or low T1WI signal but poorly defined contour and varied T2WI signal that is possibly high, equal, or low, representing granulation tissue with rich blood supply, fibrous granulation tissue, and fibrous tissue, respectively. The abnormal signal at the hepatic segment is relatively low T1WI signal, which is hardly distinguished from the lesion, but high T2WI signal, which is even and lower than the lesion. Contrast MR imaging demonstrates obvious and delayed enhancement of the granulation tissue with rich blood supply at the artery phase, while gradually obvious enhancement of the fibrous granulation tissue along with delayed time. DWI demonstrates high signal of the abscess cavity with low ADC value.
Case Study 11
A male patient aged 24 years complained of right upper abdominal pain and fever for 5 days and tachycardia. Enzyme-linked immunosorbent assay detected positive amoeba antibody.
Case Study 12
A male patient aged 61 years complained of fever for 8 days, vomiting for 5 days, right upper abdominal pain, and both feet edema for 3 days. Enzyme-linked immunosorbent assay detected positive amoeba antibody.
The cases of 11 and 12 are published in Sarda AK, et al. Korean J Hepatol, 2011, 17 (1): 71.
For case detail and figures, please refer to Sarda AK, et al. Korean J Hepatol, 2011, 17 (1): 71.
2.7.2.3 Pulmonary and Pleural Amebiasis
Chest X-Ray and CT Scanning
The demonstrations include pleural effusion and elevated diaphragm. There are pneumonia type, round mass type, cavity type, pneumothorax type, and cardiac valve involved type. The cardiac valve involved type is demonstrated with exudative change in the medial and middle parts of both lungs and diffuse intra-alveolar exudation with hilum as the center (Fig. 2.3).
Cardiac Color Ultrasound
The chordae tendineae of the mitral valve is demonstrated with rupture and prolapsed. Moderate or severe incomplete closure of the mitral valve can be demonstrated. Pressure gradient can be detected from the right to the left venous system.
Case Study 13
A female patient aged 22 years experienced fever with a body temperature of 39.4 °C, right chest pain, fatigue, and diarrhea. She was diagnosed with pleural amebiasis.
(For case detail and figures, please refer to Uslu A, et al. Respiration, 2004, 71 (4): 424.)
Case Study 14
A male patient aged 52 years, an American soldier, reported a history of living in Libya for 3 months. He complained of fever, right upper abdominal pain, and bloody stool for 10 days. By enzyme-linked immunosorbent assay, amoeba antibody was detected positive in the pleural effusion. Serum IgG antibody was detected positive.
Fig. 2.3
Pulmonary and pleural amebiasis. (a, b) X-ray demonstrates elevated right diaphragm and arch line-like shadow which is laterally high and medially low, suggesting right pleural effusion. (c) CT scanning demonstrates multiple abscesses in the liver, the largest one in size of 7 × 7 cm, which involves the diaphragm, with diaphragm perforation in length of about 2.75 cm. (d) CT scanning demonstrates inflammation at the right lower lung lobe, right pleural effusion which skips from anterior vertebra to its contralateral counterpart, leftward shift of the mediastinum, and pericardial effusion. (e, f) Reexamination after treatment for 6 weeks demonstrates absorbed and improved inflammation at the right lung and pleural effusion and shrinkage of liver abscess (Reprint with permission from Shrestha M, et al. Sout H Med J, 2010, 103 (2): 165.)
Case Study 15
A male patient aged 27 years, a homosexual, experienced dyspnea and right upper abdominal pain. By indirect hemagglutination test, amoeba antibody was detected positive.
(For case detail and figures, please refer to Chang HR, et al. Intern Med, 2010, 51 (5): 471.)
Case Study 16
A male patient aged 41 years experienced diarrhea, fever, and progressive dyspnea. He reported a medical history of amebic colonitis.
(For case detail and figures, please refer to Yokoyama T, et al. Infect Drug Resist, 2010, 3: 1.)
2.7.2.4 Brain Amebiasis
Brain Abscess
The cerebral parenchyma is demonstrated with multiple hemorrhage, malacia, and small suppurative foci. CT scanning and MR imaging demonstrate irregular lesion with no envelope and no surrounding ring-shaped enhancement.
Granulomatous Amebic Encephalitis
The disease is a necrotizing granulomatous encephalitis at the temporal lobe, brainstem, and cerebellum. Ventriculitis and choroiditis may also occur. It is pathologically characterized by scattering local necrotizing cystic space-occupying lesion. CT scanning and MR imaging demonstrate singular or multiple low-density or mixed-density space-occupying lesions at the basal ganglia, cerebral cortex, subcortical white matter, cerebellum, and pons, with ring-shaped enhancement by contrast scanning or imaging. The lesion may be surrounded by edema. In the cases with small lesions, solid nodular enhancement can be demonstrated, with inapparent surrounding edema (Figs. 2.4, 2.5, 2.6, and 2.7).
Case Study 17
A male patient aged 43 years complained of aphasia, generalized weakness, dizziness, and ataxia for 4 days. He reported a medication history of metronidazole to treat amebic liver abscess for 2 months, and he was diagnosed with metronidazole poisoning.
For case detail and figures, please refer to Kalia V. et al. Indian J Radiol Imaging, 2010, 20 (3): 195.
Case Study 18
A male patient aged 75 years experienced headache, slurred speech, and absentmindedness. He was diagnosed with granulomatous amebic encephalitis complicated by brain abscess.
For case detail and figures, please refer to Sarica FB, et al. Turk Neurosur, 2009, 19 (3): 256.
Case Study 19
A male patient aged 40 years experienced fever and dizziness. He was diagnosed with chronic granulomatous amebic encephalitis.
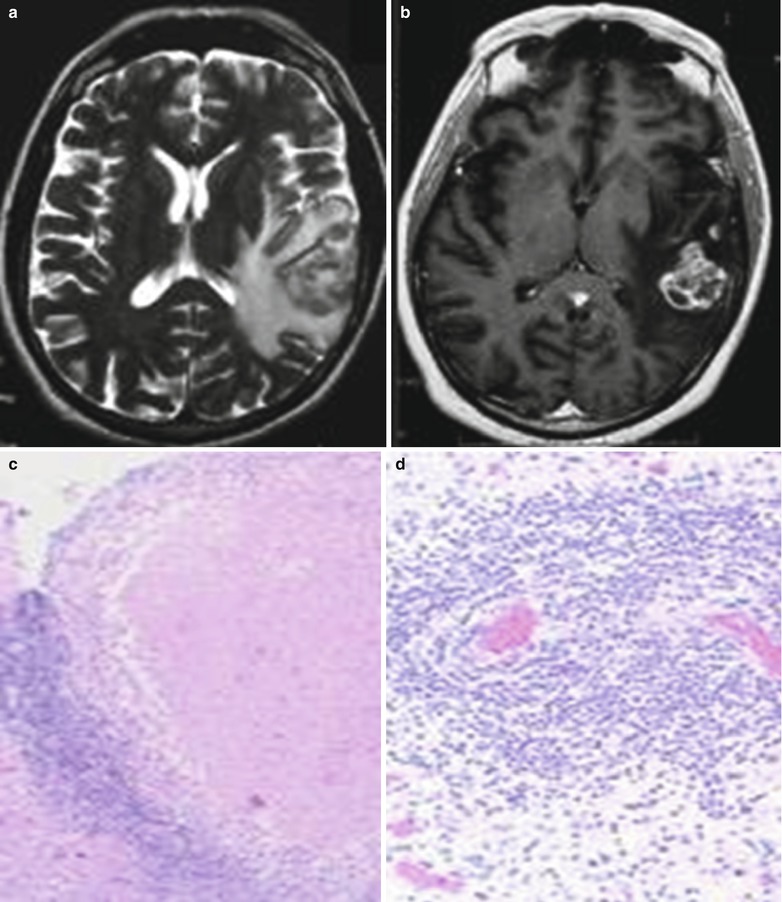
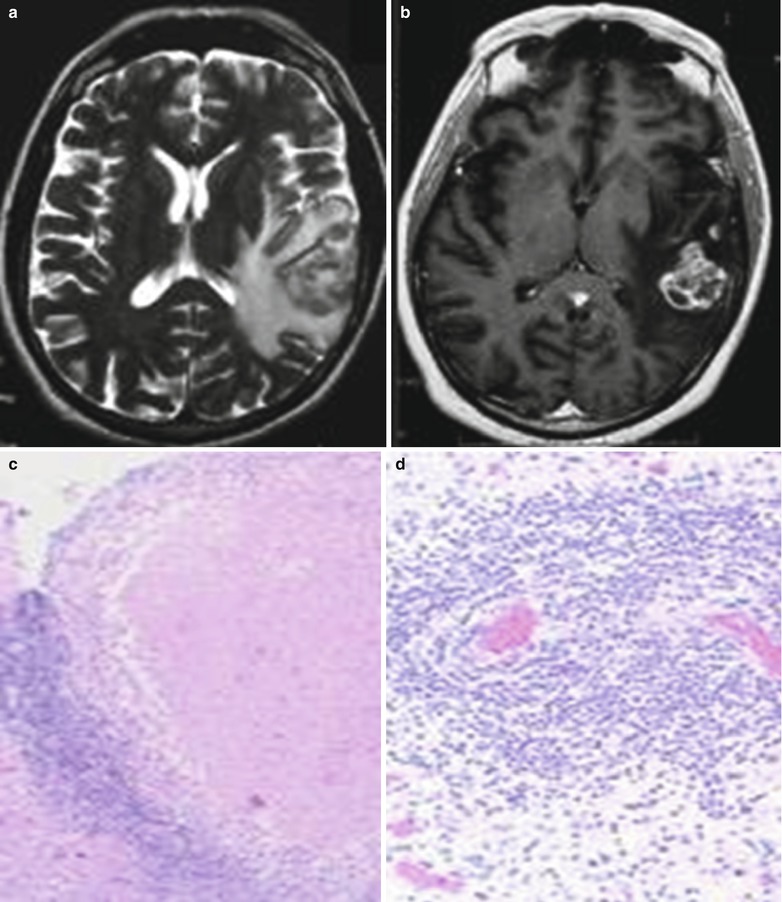
Fig. 2.4




Chronic granulomatous amebic encephalitis. (a) T2WI of MR imaging demonstrates mixed signal shadow at the left temporal and parietal lobes, with surrounding large flakes of edema signal. (b) Contrast T1WI demonstrates floral hoop-like enchantment of the lesion at the left parietal lobe. (c) Microscopy demonstrates lymphocytes around cuff blood vessel (H&E staining, with original medium magnification). (d) Microscopy demonstrates necrotizing granulomatous inflammation (H&E staining, with original magnification) (Reprint with permission from Perez MT, et al. Ann Diagn Pathol 2007, 11 (6): 440.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree