Jean Noel Buy1 and Michel Ghossain2
(1)
Service Radiologie, Hopital Hotel-Dieu, Paris, France
(2)
Department of Radiology, Hotel Dieu de France, Beirut, Lebanon
27.1.1 Cervicitis
27.2.1 Metaplasia []
27.2.2 Hyperplasia
27.3 Cysts
27.3.1 Nabothian Cyst
27.3.2 Tunnel Clusters
27.4 Benign Tumors
27.4.1 Endocervical Polyps
27.4.3 Leiomyomas
Abstract
Cervicitis can be infectious related to different microorganisms (bacteria, viruses, fungi, protozoa, and parasites) or noninfectious (chemical or mechanical) [1].
27.1 Inflammatory Diseases
27.1.1 Cervicitis
Cervicitis can be infectious related to different microorganisms (bacteria, viruses, fungi, protozoa, and parasites) or noninfectious (chemical or mechanical) [1].
Infectious cervicitis can affect either the endocervical-type columnar epithelium producing mucopurulent endocervicitis or the epithelium of the exocervix producing exocervicitis.
In this clinical setting, MR can display retention cysts [2].
27.1.2 Exophytic Condyloma Acuminata [1]
It is one of the common manifestations of human papilloma virus (HPV) infection of the lower anogenital tract. It is caused by HPV types 6 and 11. They are commonly multifocal and may involve the mature squamous epithelium of the exocervix as well as the immature squamous epithelium of the transformation zone.
At colposcopy, they appear white exophytic lesions with papillary projections.
Other aspects include maculopapular, only slightly raised lesions.
27.2 Metaplasia-Hyperplasia
27.2.1 Metaplasia [1]
Metaplasia can be from tubal, tubo-endometrioid, or transitional cell type.
In tubal metaplasia, endocervical glands are lined by Müllerian-type epithelium that resembles that of the fallopian tube. It can be quite extensive and can occasionally be mistaken for endocervical glandular neoplasia.
Glands are typically confined to the superficial third of the cervical wall (they extend less than 7 mm into the cervical stroma). It can be typical or atypical.
27.2.2 Hyperplasia
According to its origin (endocervical glands or mesonephric duct remnants), there are two types, microglandular hyperplasia and mesonephric hyperplasia.
27.2.2.1 Microglandular Hyperplasia [1]
Histology
It is a benign proliferation of endocervical glands forming tightly packed glandular or tubular units of varying sizes lined by flattened to cuboidal cells with eosinophilic cytoplasm containing small quantities of mucin. Stroma separating the glands is usually infiltrated with acute and chronic inflammatory cells.
It can be present as a simple focus or as multiple foci. It may involve the surface or deeper portions of endocervical clefts.
Clinical Findings
It is common in women of reproductive age as a result of contraceptive or in pregnant women.
It can result in postcoital bleeding or spotting.
It can form a cervical polyp of 1–2 cm.
MR Findings
They are similar to those of hyperplasia of the endometrium (Fig. 27.1).
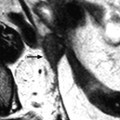
Fig. 27.1
Endometrial hyperplasia with foci of mucinous metaplasia of the endometrium extending into the endocervix (same patient as Fig. 22.20). Seventy-five-year-old woman with metrorrhagia and hydrorrhea. (a, b) Sagittal T2W images display thickening of the endometrium and to a lesser extent of the cervical mucosa (arrow) with multiple cystic glands. Deeper cystic glands in the myometrium are also present related to adenomyosis
Differential Diagnosis
Microglandular hyperplasia with solid areas can be difficult to distinguish from adenocarcinoma on pathology [1].
27.2.2.2 Mesonephric Hyperplasia
Definition
The vestigial elements of the distal ends of the mesonephric ducts are found in 1–22 % of adult cervices. Mesonephric remnants are most commonly present in the lateral aspects of the cervix. They consist of tubules or cysts that are usually located deep in the lateral cervical wall.
Mesonephric remnants may become hyperplastic, resulting in a tubuloglandular proliferation with transmural involvement of the cervix. The most common form is the lobular type that is characterized by clustered mesonephric tubules with or without a centrally mesonephric duct.
Mesonephric hyperplasia is almost always asymptomatic and is detected on cervical biopsy or hysterectomy specimens.
Differential Diagnosis
Minimal-deviation adenocarcinoma of the endocervix can be differentiated by:
1.
Lack of complex glandular pattern and periglandular stromal edema
2.
Absence of cytologic features: mitosis, intracellular mucin
3.
Absent carcinoembryonic antigen (CEA)
27.2.2.3 Imaging Findings
On MR, endocervical hyperplasia appeared as a multicystic mass with thin and regular walls, which can be in some cases partially thickened separating by stroma with contrast uptake. Differential diagnosis can be with Nabothian cysts, tunnel clusters, and adenocarcinoma (Table 27.3).
27.3 Cysts
27.3.1 Nabothian Cyst
27.3.1.1 Definition
They are lined by a single layer of mucin-producing endocervical epithelium, which is flattened. They develop most frequently within the transformation zone secondary to squamous metaplasia.
27.3.1.2 Macroscopic and Radiologic Findings
They are very common incidental findings on US and MR. They are frequently multiple and exceptionally large (Fig. 27.2). Their characteristics are reported in Table 27.1.




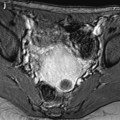
Fig. 27.2
Large Nabothian cyst. Thirty-eight-year-old woman with a large known Nabothian cyst that has increased in size on clinical examination. (a) EVS shows a large loculated Nabothian cyst that has increased in size since the last examination (7 cm vs. 3 cm, one and a half year before). (b, c) MR T2W sagittal (b) and axial (c) show a large anterior loculated cyst c or more precisely several Nabothian cysts (a main large cyst and smaller cysts giving a multiloculated appearance). (d, e) MR T1W axial images without (d) and with fat suppression (e) did not show any hyperintensity suggestive of hemorrhage. (f–i) DMR before injection (f), at the arterial (g), venous (h), and delayed (i) phases, did not show any nodular or suspicious contrast uptake in the cysts
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree