Jean Noel Buy1 and Michel Ghossain2
(1)
Service Radiologie, Hopital Hotel-Dieu, Paris, France
(2)
Department of Radiology, Hotel Dieu de France, Beirut, Lebanon
35.1 Cysts []
35.1.1 Bartholin Gland Cyst
35.1.2 Epithelial Inclusion Cysts
35.1.3 Mucinous Cysts
35.1.4 Mesonephric-Like Cysts
35.1.5 Cyst of the Canal of Nuck
35.1.7 Suburethral Diverticulum
35.2.1 Bartholinitis
35.2.2 Labial Cellulitis (Fig. )
35.2.3 HPV Infection
35.3 Benign Tumors []
35.3.1 Epithelial
35.3.2 Mesenchymal Tumors
Abstract
The major vestibular (Bartholin) glands are bilaterally adjacent to the posterior vestibular bulb with acini composed of simple columnar mucus-secreting epithelium.
35.1 Cysts [1]
35.1.1 Bartholin Gland Cyst
35.1.1.1 Anatomy and Histology of the Glands
The major vestibular (Bartholin) glands are bilaterally adjacent to the posterior vestibular bulb with acini composed of simple columnar mucus-secreting epithelium.
Each gland is drained just external to the hymen ring of the vestibule posterolaterally. The Bartholin duct 2.5 cm length is lined:
Proximally by mucus-secreting epithelium
Then transitional epithelium
At its exit squamous epithelium
35.1.1.2 Pathology of the Cyst
Duct obstruction occurs at their vestibular orifice, situated at the 5 and 7 o’clock positions between the hymen and labia minora, with subsequent accumulation of secretion and cystic dilatation. The cyst can appear posterolaterally or laterally in the vestibule. The cyst lining varies from mucin secreting to squamous or transitional. The content of an uninfected Bartholin cyst is either clear or mucoid highly viscous and thick.
35.1.1.3 MR Imaging
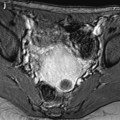
When the content is clear fluid, the signal intensity on T1 and T2 is like urine (Fig. 35.1). When mucoid, their signal intensity is intermediate on T1 and intermediate or high on T2 (Fig. 35.2).
Fig. 35.1
MRI of an uninfected Bartholin gland cyst with translucent liquid. Axial (a) and sagittal (b) T2W images, axial T1W image (c), axial T1W-FS image after gadolinium injection (d). Biloculated cystic lesion (arrows) developed lateral to the introitus. This topography is typical for a Bartholin cyst. Signal intensity identical to urine is related to its aqueous uninfected content as confirmed at excision
Fig. 35.2
Mucoid uninfected Bartholin cyst. Sagittal (a) and axial (b) T2W images with vaginal opacification, Sagittal T1W image (c), and axial T1W images (d). Two centimeters cyst (arrows) located posterolaterally to the introitus at 5 o’clock, compressing the wall of the vagina. This topography is typical for a Bartholin cyst. The cyst has an intermediate signal on T1 and on T2 related to its mucoid content confirmed at excision
Complications
Infection (see below)
Association of Bartholin adenocarcinoma
35.1.2 Epithelial Inclusion Cysts
Definition: Lined by a stratified squamous epithelium
Location: The labia majora and clitoris
Size: 2–5 mm
Content: Keratinous
35.1.3 Mucinous Cysts
Definition: Lined by mucus-secreting columnar epithelium
Location: Minor vestibular gland
Content: Mucinous
35.1.4 Mesonephric-Like Cysts
Definition: The epithelium is cuboidal to columnar
Location: Lateral aspects of the vulva
Content: Clear fluid
35.1.5 Cyst of the Canal of Nuck
Location:
The superior aspect of the labia majora
Inguinal canal
They must be distinguished from an inguinal hernia with which they are associated in one-third of cases [2].
There are comma-shaped cysts with their tails directed cranially toward the inguinal canal.
35.1.6 Urothelial Cysts (Skene Duct Cysts)
Skene ducts run parallel to the urethra and are located lateral and posterior to the external urethral meatus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree