Anatomy, embryology, pathophysiology
- ◼
Lesions in the liver are often characterized based upon underlying histology. The most common benign lesions include simple cysts, hemangiomas, hepatocellular adenoma (HCA), focal nodular hyperplasia (FNH), regenerative nodules, and hepatic abscess.
- ◼
Most benign hepatic lesions are asymptomatic and found incidentally ( Fig. 17.1 ). Symptoms, if present, are often related to mass effect including pain/discomfort, nausea, vomiting, or early satiety.
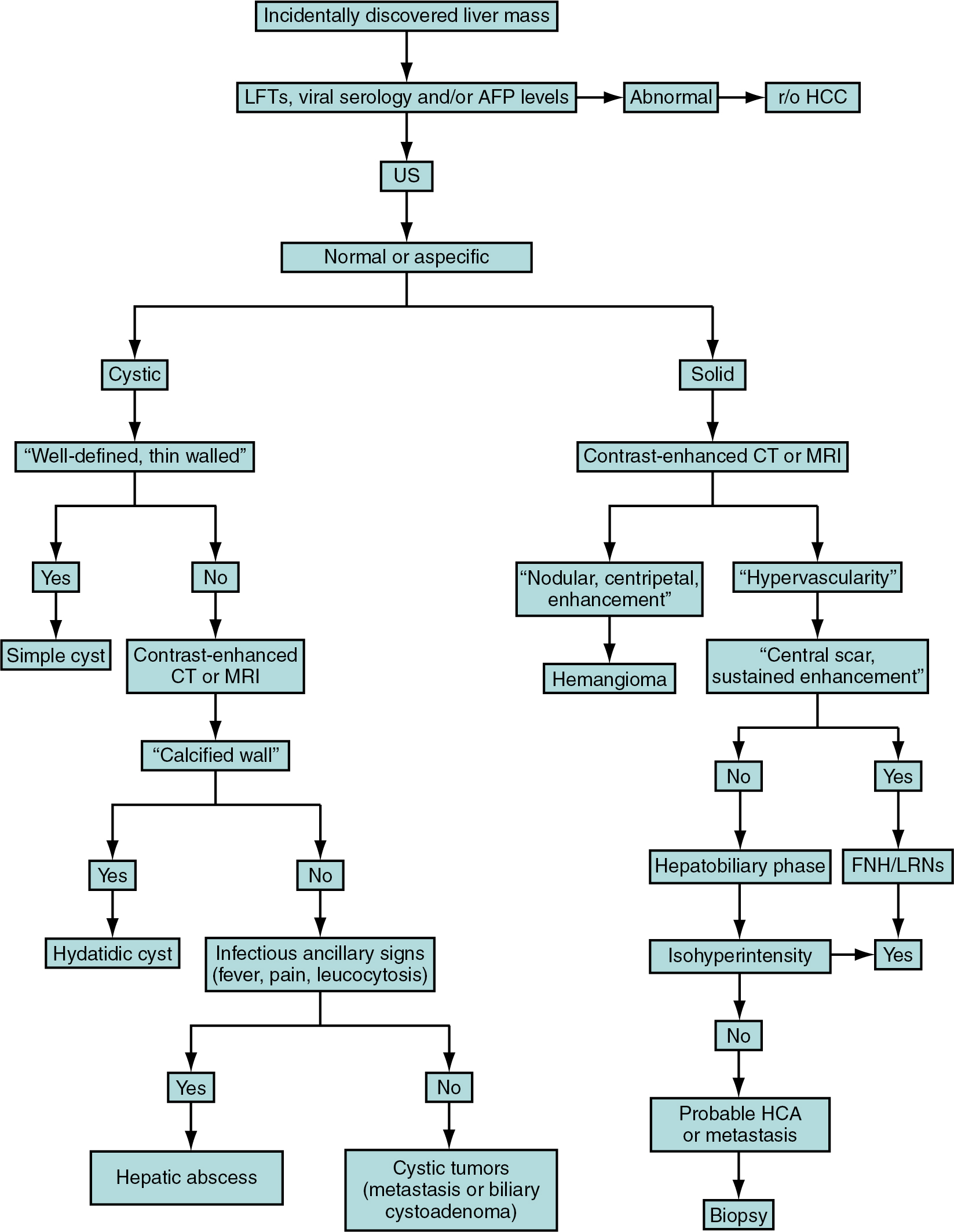
Fig. 17.1
Flow chart of a practical diagnostic approach to management of benign hepatic lesions. AFP , Alpha-fetoprotein; CAs , contrast agents; CT , computed tomography; FNH , focal nodular hyperplasia; HCA , hepatocellular adenoma; HCC , hepatocellular carcinoma; LFTs , liver function tests; LRNs , large regenerative nodules; MRI , magnetic resonance imaging; r/o , rule out; US , ultrasound.
(From Sahani DV, Samir AE. Abdominal Imaging , ed 2. Philadelphia: Elsevier; 2017.)
- ◼
Hepatic abscess may present with signs of infection including fever and leukocytosis.
- ◼
HCA can present with hemorrhage and possible rupture.
Techniques
Computed tomography
- ◼
Multiphase computed tomography (CT) including hepatic arterial phase, portal venous phase, and delayed phase (equilibrium, 3 min) is the protocol of choice for evaluation of hepatic lesions.
- ◼
Precontrast acquisition may be helpful in evaluation of cysts and areas of spontaneous hyperdensity.
Magnetic resonance imaging
- ◼
In- and out-of-phase imaging and fat suppression techniques can demonstrate areas of microscopic and macroscopic fat, respectively.
- ◼
Hepatocyte specific contrast agents are taken up by well differentiated/functional hepatocytes, which allows for evaluation for dedifferentiated masses or masses of nonhepatic origin using uptake characteristics. Commonly used agents include Eovist/Primovist (Gd-EOB-DTPA; 50% hepatocyte uptake) and MultiHance (Gd-BOPTA; 2%–4% hepatocyte uptake) ( Fig. 17.2 ).
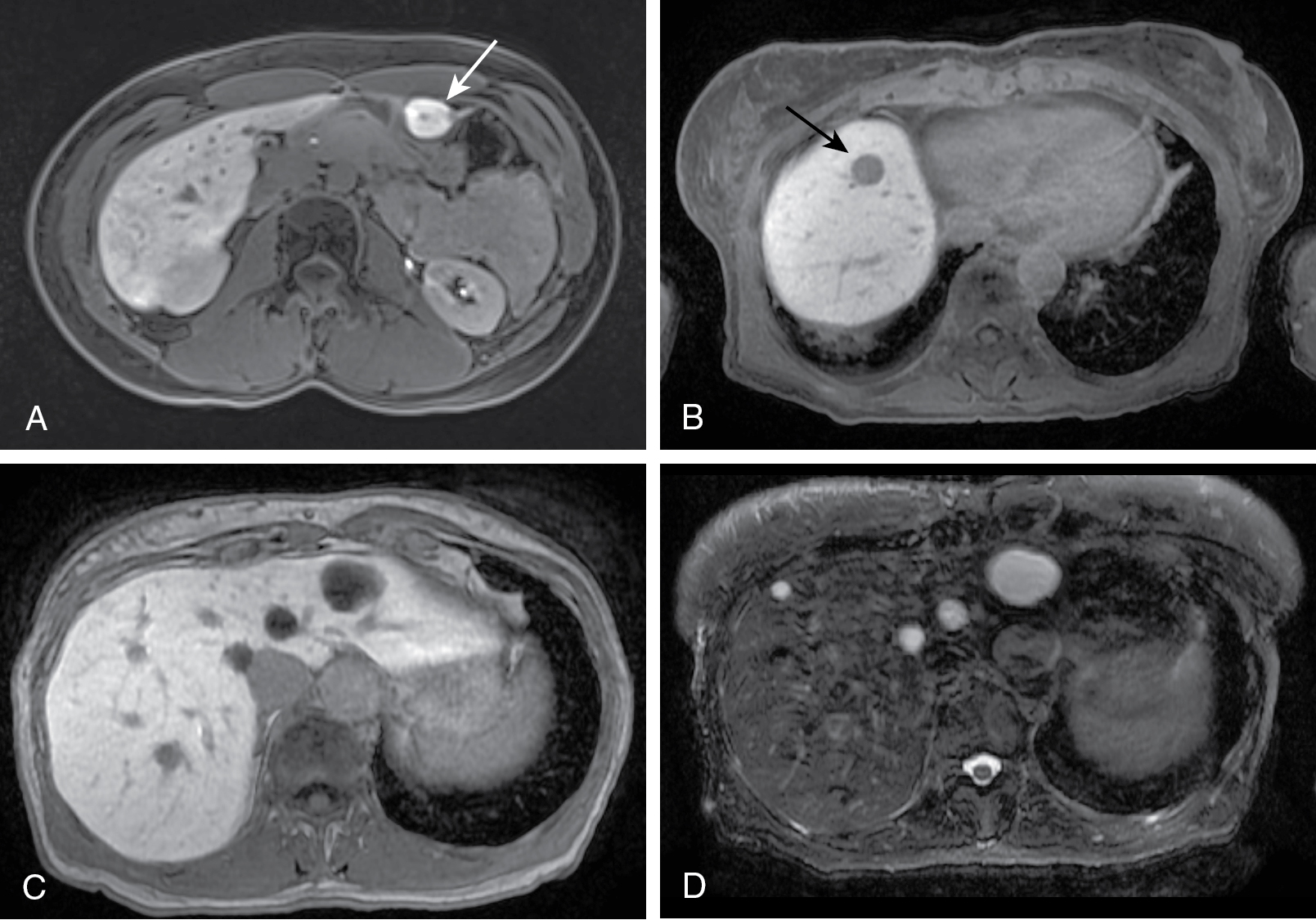
Fig. 17.2
Liver lesions on hepatobiliary imaging after Eovist administration. A, Hepatobiliary imaging at 20 minutes in a 28-year-old woman demonstrating uptake in a segment 3 focal nodular hyperplasia (arrow), which contains functional hepatocytes. B to D, A 67-year-old woman with breast cancer demonstrating both malignant and benign liver lesions. Twenty-minute hepatobiliary imaging shows lack of uptake in lesions without normal hepatocytes, such as a metastasis ( arrow in B). Benign lesions such as cysts (left hepatic lesions in C) also show lack of Eovist uptake. Correlation with T2 signal is necessary for differentiating cysts (D) or hemangiomas from metastases.
(From Sahani DV, Samir AE. Abdominal Imaging , ed 2. Philadelphia: Elsevier; 2017.)
- ◼
Diffusion-weighted imaging (DWI) can evaluate impedance to the microscopic movement of water molecules often indicating areas of increased or disorganized cellularity.
Ultrasound
- ◼
Low cost, lack of ionizing radiation, and availability make ultrasound (US) a good modality for primary evaluation.
- ◼
Decreased sensitivity because of body habitus and bowel gas, operator skill dependence, and limited field of view are all limitations to this modality.
- ◼
Although some lesions, such as cysts (anechoic) and hemangiomas (hyperechoic) are often easily identified, others may be indistinguishable from background liver.
- ◼
Elastography and microbubble contrast may provide additional diagnostic information.
Specific disease processes
Simple cyst
- ◼
Often incidental and asymptomatic, they are most common in middle aged women (5:1), although cysts can be seen at any age and may demonstrate mass effect if large enough.
- ◼
They be complicated by hemorrhage, rupture, or secondary infection.
- ◼
Lined by cuboid epithelium identical to bile ducts, indicating biliary origin.
- ◼
May cause increased alkaline phosphatase or bilirubin if there is mass effect upon the bile ducts.
Computed tomography
- ◼
Cysts are thin walled well-defined fluid attenuating lesions that are often unilocular although septae or multiloculation may be present. Neither the cyst nor wall should show enhancement ( Fig. 17.3 ).

Fig. 17.3
Typical presentation of hepatic (bile duct) simple cyst. A, Axial precontrast computed tomography (CT) image shows a large, sharply defined lesion ( arrow ) in the left lobe of the liver that is hypoattenuating compared with the surrounding hepatic parenchyma and aorta. Hypoattenuation to the aorta on precontrast images is the single most important finding to diagnose cystic lesions on CT. B, Corresponding contrast-enhanced CT scan during portal venous phase demonstrates absence of lesion enhancement. C, Ultrasound image in a different patient shows a round, well-circumscribed mass ( arrow ) with imperceptible wall and increased through-transmission of sound waves.
(From Sahani DV, Samir AE. Abdominal Imaging , ed 2. Philadelphia: Elsevier; 2017.)
Magnetic resonance imaging
- ◼
Prolongation of both T1 and T2 because of fluid content is present, which manifests as low T1 signal and high T2 signal. Internal hemorrhage may show variable signal intensities based upon age and amount of blood content. No enhancement or connection to the biliary tree should be present.
Ultrasound
- ◼
Well-defined anechoic lesion with posterior acoustic enhancement and no internal flow on Doppler.
Differential diagnosis
- ◼
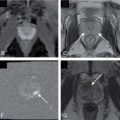
Complex features or deviation from the aforementioned imaging characteristics should make one consider alternative diagnoses ( Fig. 17.4 ). These include abscess, hydatid cysts, peribiliary cysts ( Fig. 17.5 ), biliary hamartoma/cystadenoma/cystadenocarcinoma ( Figs. 17.6 and 17.7 ), choledochal cyst ( Fig. 17.8 ), or necrotic metastases.

Fig. 17.4
Imaging findings and differential diagnosis among different cystic lesions of the liver, including hydatid cyst, simple cyst, pyogenic abscess, biliary cystadenoma, polycystic liver disease, biliary hamartomas, and Caroli disease. A to F, Portal venous phase computed tomography. G, Gadolinium-enhanced T1-weighted gradient recalled echo magnetic resonance image. A, Calcified wall ( black arrow ), thick enhancing wall ( arrow ), and daughter cysts ( asterisks ) are typical of hydatid cyst. B, A simple hepatic cyst has no visible wall ( arrow ). Note the mild intrahepatic biliary dilatation ( arrowhead ) secondary to mass effect in both cases. Other findings that may help in narrowing differential diagnosis when facing cystic liver lesions are (C and D) thick enhancing walls ( arrow, C) and internal septa ( arrow, D) in pyogenic liver abscess and biliary cystadenoma, (E) multiplicity and partially calcified walls in polycystic liver disease, (F) small size (<15 mm) and multiplicity ( arrows ) in biliary hamartomas, and (G) demonstration of a “dot sign” ( arrow ) resulting from a centrolesional portal venous branch in Caroli disease.
(From Sahani DV, Samir AE. Abdominal Imaging , ed 2. Philadelphia: Elsevier; 2017.)

Fig. 17.5
Biliary hamartoma. The coronal heavily T2-weighted (A) and fat-suppressed, moderately T2-weighted (B) images reveal multiple small fluid-intense lesions scattered throughout the liver. The maximal intensity projection image from a three-dimensional magnetic resonance cholangiopancreatography sequence (C) confirms high fluid content isointense to bile. Note the mild hyperintensity of the breast implants, typical of silicone and less intense than saline.
(From Roth C, Deshmukh S. Fundamentals of Body MRI , ed 2. Philadelphia: Elsevier; 2016.)

Fig. 17.6
Magnetic resonance cholangiopancreatography in a 70-year-old man with multiple small peribiliary T2 bright cysts ( arrow ) caused by peribiliary cystic disease. There are several small associated side-branch intraductal papillary neoplasms ( small arrows ).
(From Boland GW. Gastrointestinal Imaging: the Requisites , ed 4. Philadelphia: Saunders; 2014.)

Fig. 17.7
Axial T2-weighted (A) and postcontrast (B) magnetic resonance imaging in a 36-year-old woman with a complex cystic 9-cm biliary cystadenoma. Note internal septa ( arrows ).
(From Boland GW. Gastrointestinal Imaging: the Requisites , ed 4. Philadelphia: Saunders; 2014.)


Fig. 17.8
Axial T2-weighted fat-saturated magnetic resonance imaging (A) and axial contrast-enhanced computed tomography (CT) (B) in a 39-year-old woman with type V choledochal cyst (Caroli disease), multiple T2 bright ectatic bile ducts, and a CT central dot sign ( small arrow ).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree