Fig. 10.1
Schematic of a parasternal approach to a mediastinal biopsy on a transverse CT section through the thorax at the level of the aortic arch. The needles are inserted lateral to the sternum and advanced into the mediastinal masses (M)
Occasionally, the space between the lateral edge of the sternum and the internal mammary vessels may be too small to allow safe parasternal needle placement. Placing the patient in a lateral decubitus position may cause the mediastinum to shift laterally toward the dependent side, bringing the lesion or the mediastinal fat into direct contact with the parasternal chest wall and allowing the needle access to the lesion (Fig. 10.2) [2, 5]. Alternatively, saline solution or dilute contrast medium can be injected to create an artificial extrapleural path for needle placement (Fig. 10.3) [9]. Under CT guidance, a 22-gauge needle is advanced into the extrapleural space to inject the saline solution and create a “salinoma” window. After creation of this safe extrapleural window, the 22-gauge needle is removed and a large-bore (18-gauge or larger) guide needle is advanced through the salinoma to the lesion. Subsequently, using a coaxial technique, FNAB and core biopsies can be obtained through the guide needle. Alternatively, a 22-gauge needle with a removable hub can be used for initial localization, allowing advancement of the guide needle over the 22-gauge needle. It is important to remember that the degree of contact between the mediastinum and the parasternal chest wall may alter with the patient’s breathing during the biopsy procedure, precluding the use of the parasternal approach or resulting in inadvertent traversal of the lung or pleural space (Fig. 10.4). Breathing can also cause a small mediastinal lesion to move out of the biopsy plane.
Fig. 10.2
Schematic showing the use of decubitus positioning for a parasternal approach. (a) In the supine position, aerated lung is interposed between the mass (M) and the chest wall. (b) In the left lateral decubitus position, the mediastinum shifts to the left, creating a mediastinal window for needle placement
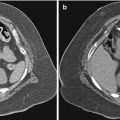
Fig. 10.3
Artificial widening of mediastinum for parasternal approach. (a) A CT scan shows an anterior mediastinal mass (M) and a narrow parasternal mediastinal window (arrowheads). (b) A CT scan shows the mediastinum widened by the injection of saline solution (arrowheads), allowing for extrapleural placement of the biopsy needle (arrow)
Fig. 10.4
Inadvertent pulmonary traversal during parasternal biopsy. (a) A CT scan shows an anterior mediastinal mass (M) in contact with the anterior chest wall. Note the extent of mediastinal fat (arrowhead) and the planned needle trajectory. (b) A CT scan shows lung (L) in the path of the needle causing separation of the mediastinal fat from the anterior chest wall. (c) A drawing illustrates how interposition of the parietal pleura into the needle’s path can result in inadvertent traversal of the pleural space during a parasternal biopsy
For a US-guided parasternal biopsy (Fig. 10.5), the parasternal access window should be large enough to allow space for the transducer face and for simultaneous needle placement; hence, the use of US guidance is generally limited to biopsies of large anterior mediastinal lesions. Because of the small size of the access window, a small-footprint transducer is used, and a freehand technique is preferred over needle-attachment guides. It is essential to identify and avoid the major mediastinal blood vessels, including the internal mammary vessels; if needed, color Doppler imaging can be used for this purpose [11]. In some patients, curvature of the anterior ribs or costal cartilage may not allow enough space for the US transducer and the biopsy needle.
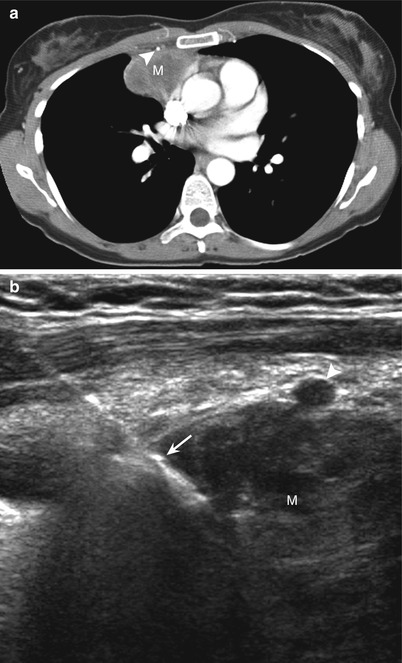
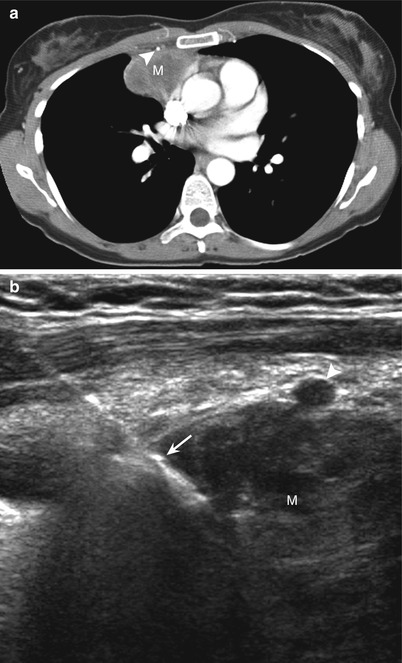
Fig. 10.5
US-guided parasternal biopsy. (a) A CT scan shows an anterior mediastinal mass (M). Note the position of the internal mammary vessels (arrowhead). (b) An ultrasonogram shows the biopsy needle (arrow) inserted via a parasternal approach and advanced lateral to the internal mammary artery (arrowhead) into the mass (M)
The parasternal approach also is appropriate for biopsies of anterior or middle mediastinal lesions. Although the parasternal approach is used mostly for needle biopsy of prevascular lesions or masses in the aortopulmonary window (Fig. 10.6), pretracheal or paratracheal lesions can also be accessed with this approach by advancing the needle between the major vessels (Fig. 10.7). Traversal of the brachiocephalic veins or superior vena cava with thin (e.g., 22-gauge) needles for biopsy of middle mediastinal lesions has been safely performed without complications [3, 7, 12]. Occasionally, a left parasternal approach may be used to access a lesion in the right mediastinum (Fig. 10.8).
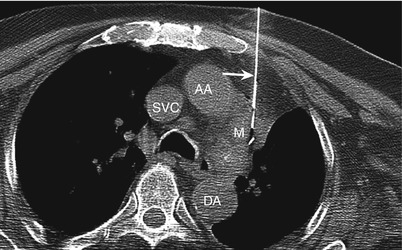
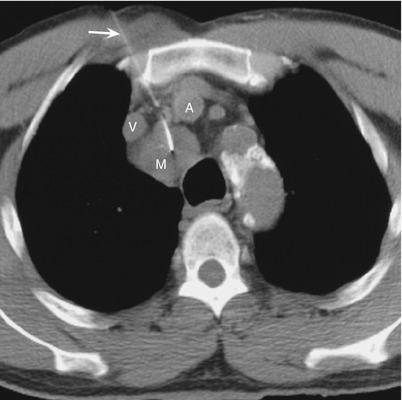
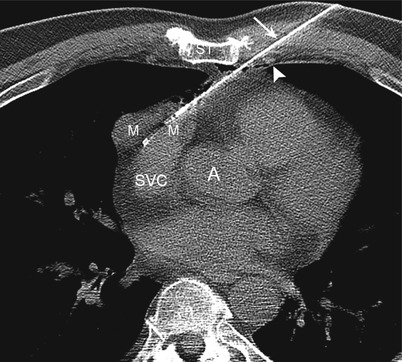
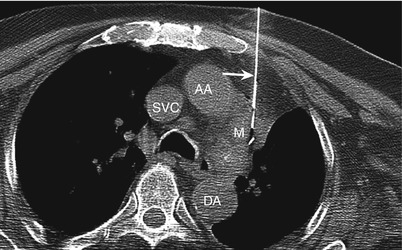
Fig. 10.6
Parasternal approach. A CT scan shows a biopsy needle (arrow) advanced through the mediastinal fat into an aortopulmonary window mass (m). Note the relationship of the mass to the aortic arch (AA), descending thoracic aorta (DA), and superior vena cava (SVC)
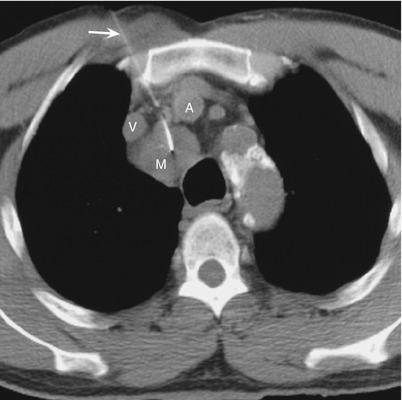
Fig. 10.7
Parasternal approach. A CT scan shows a biopsy needle (arrow) advanced between the right brachiocephalic vein (V) and artery (A) for biopsy of a pretracheal mass (M)
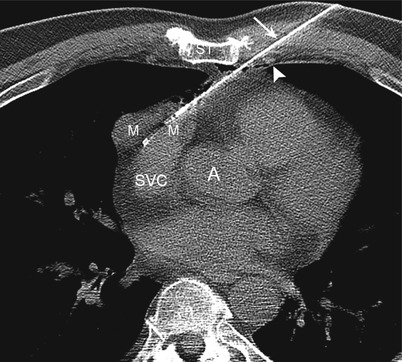
Fig. 10.8
Parasternal approach. A CT scan shows a biopsy needle (arrow) advanced between the sternum (ST) and internal mammary vessels (arrowhead) on the left side for biopsy of an anterior mediastinal mass (m) on the right side. Note the position of the superior vena cava (SVC) and aortic root (A)
Paravertebral Approach
For the paravertebral approach, the patient is generally placed in the prone position; patients who are unable to lie prone may be placed in a prone oblique or lateral decubitus position. The needle is advanced immediately lateral to the vertebral body between the endothoracic fascia and the parietal pleura. The endothoracic fascia, located outside the parietal pleura, lines the walls of the thorax and merges with the prevertebral fascia posteromedially. In some patients, the paravertebral extrapleural space may be wide enough to allow needle biopsy without traversing the pleura. However, in most patients, an injection of saline solution or a dilute iodinated contrast medium is required to displace the mediastinal parietal pleura and gain extrapleural access (Fig. 10.9) [5, 9].
Fig. 10.9
Schematic of the extrapleural paravertebral approach for needle biopsy of a posterior mediastinal mass (M) after widening of the mediastinal space by injection of saline solution
An 18-gauge blunt-tip needle or cannula is used for creation of the extrapleural window; the same needle can be used as the guide needle for performing the biopsy with a coaxial technique (Fig. 10.10). Alternatively, a 22-gauge needle may be introduced initially to inject fluid and subsequently be exchanged for an 18-gauge needle to perform the biopsy [9]. In most patients, injection of 10–20 mL of saline solution is sufficient to achieve adequate mediastinal widening; however, larger volumes may be required [18]. Insufficient widening can occur when the needle tip lies outside the endothoracic fascia, in a blood vessel, or in the pleural space. The injection of saline solution also displaces mediastinal structures, such as the azygos vein, esophagus, nerves, and vertebral blood vessels, from the needle’s path, thereby reducing the risk of inadvertent injury to these structures. Needle advancement and biopsy must be performed expeditiously because the mediastinal widening regresses along with the redistribution of fluid. The needle should be inserted medial to the pleural surface at the head of the ribs. Administration of saline through a needle placed lateral to the transverse process may not achieve mediastinal widening because of the fixation of the endothoracic fascia and parietal pleura at this location [5, 9]. The biopsy needle should be placed along the superior edge of the rib and above the transverse process to avoid injury to the intercostal nerve and artery. Some investigators recommend oral administration of a contrast medium if the esophagus is not identified on non-contrast-enhanced CT scans [5, 9]. In some patients, the presence of large osteophytes or the orientation of the transverse process may preclude paravertebral extrapleural access [19].
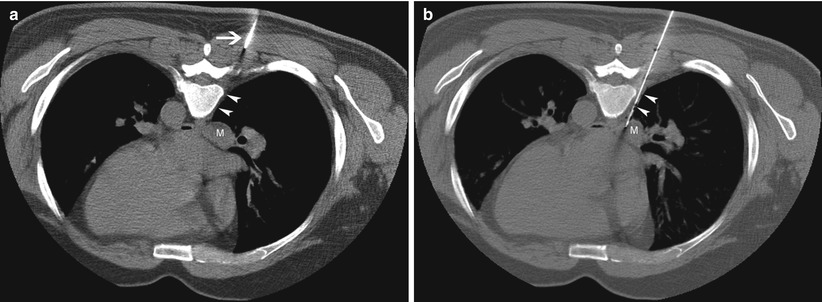
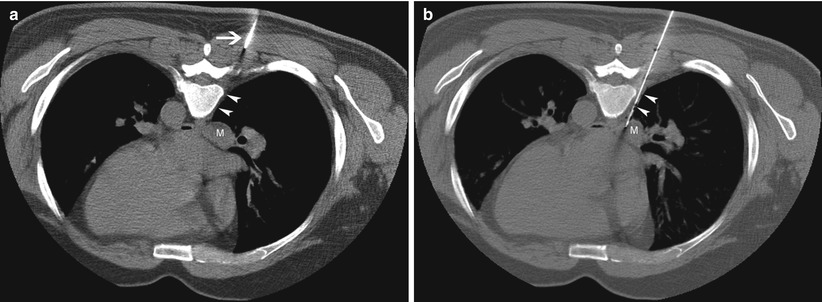
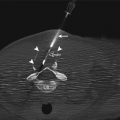
Fig. 10.10
Paravertebral approach for subcarinal mass. (a) A CT scan obtained with the patient prone shows a subcarinal mass (M); an 18-gauge needle (arrow) has been advanced to the edge of the paravertebral space (arrowheads). (b) A CT scan obtained with the patient prone shows how the injection of saline solution has widened the mediastinum (arrowheads), creating a safe extrapleural path to the mass (M)
The paravertebral approach allows access to posterior mediastinal lesions and is used mostly for biopsy of subcarinal lesions from the right side (Fig. 10.10). Occasionally, a saline injection may cause sufficient displacement of the descending aorta to allow retroaortic access from the left side (Fig. 10.11) for biopsy of subcarinal, periesophageal, or left paratracheal masses. To avoid inadvertent injury to the aorta, only a blunt-tip guide needle should be used with this approach. The right paravertebral approach can also sometimes be used for accessing middle mediastinal lesions located in the pre- or paratracheal spaces, especially cranial to the level of the arch of the azygos vein [19].
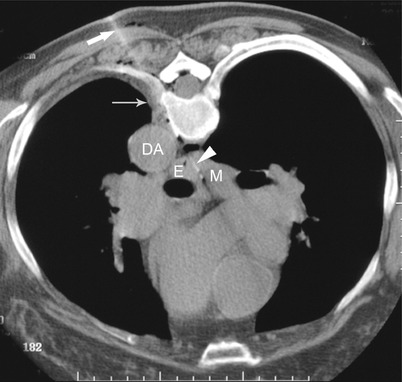
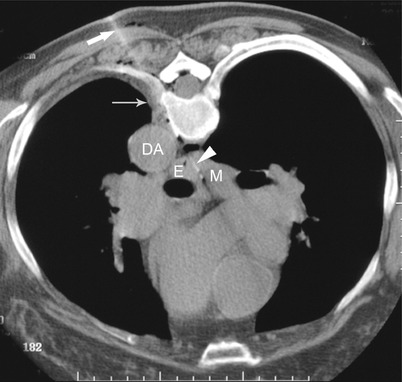
Fig. 10.11
Paravertebral retroaortic approach. A CT scan shows an 18-gauge guide needle (thick arrow) inserted into the paravertebral space (thin arrow) and advanced between the descending aorta (DA) and vertebral body after widening of these spaces by saline injection. A 22-gauge needle (arrowhead) was advanced through the guide needle to obtain aspirates from the subcarinal mass (M). E esophagus
Transsternal Approach
The transsternal approach involves needle placement through the sternum (Fig. 10.12). Any of the commonly available 18-gauge guide needles (Chiba [Cook Inc., Bloomington, IN] or Hawkins-Akins [Meditech, Westwood, MS]) are adequate to penetrate the sternum. Although an 18-gauge hypodermic needle can also be used to penetrate the sternum, it precludes the insertion of a coaxial 20-gauge core-biopsy needle to obtain larger specimens when needed [8]. If necessary, larger-caliber bone biopsy systems and drill bits can be used to gain transsternal access.
Fig. 10.12
Schematic of the transsternal approach showing needles traversing the sternum for biopsy of anterior mediastinal, preaortic, or pretracheal masses (M)
Transsternal needle insertion performed with local anesthesia and intravenous sedation is well tolerated by most patients. Injection of a local anesthetic into the periosteum of the anterior and posterior sternal cortices minimizes the discomfort associated with the procedure. A non-contrast-enhanced CT study obtained immediately before the procedure should be sufficient for safe biopsy planning in most patients who have had previous diagnostic contrast-enhanced CT scans; rarely, intravenous administration of a contrast agent may be needed during the procedure to help differentiate among mediastinal structures.
The transsternal approach is used for biopsy of lesions that are not safely accessible by the parasternal approach. The transsternal approach is usually used for biopsy of anterior mediastinal masses (Fig. 10.13) [6, 13] but also allows access to middle or posterior mediastinal masses (Fig. 10.14) [8]. Traversal of a brachiocephalic vein with 22-gauge needles for biopsy of middle or posterior mediastinal masses has been shown to be safe (Fig. 10.15) [8]. A curved 22-gauge Chiba needle can also be used to compensate for minor discrepancies in the trajectory of the guide needle (Fig. 10.16) [8]. Saline administration can be used to increase the contact between the mediastinum and the sternum to avoid pleural traversal as in the parasternal technique (Fig. 10.16).
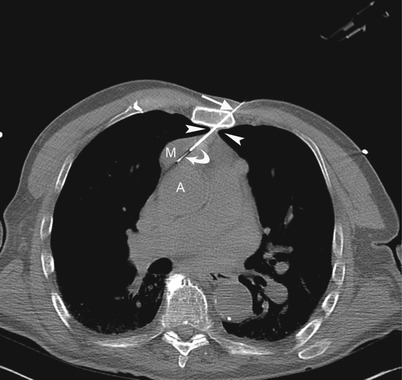
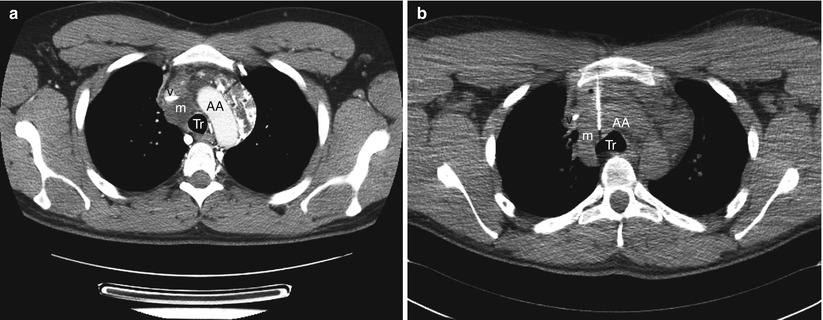
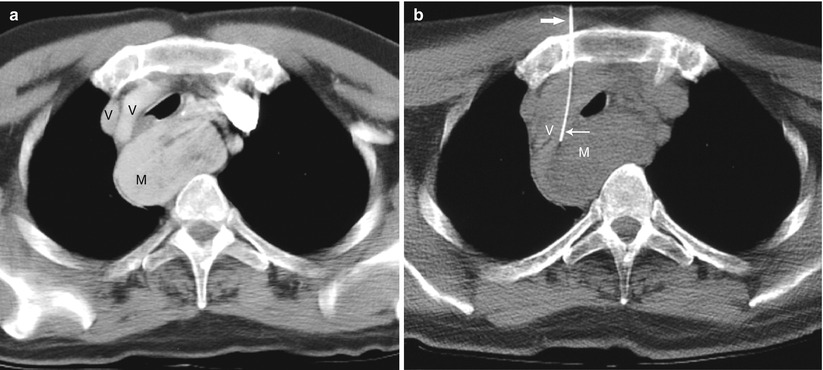
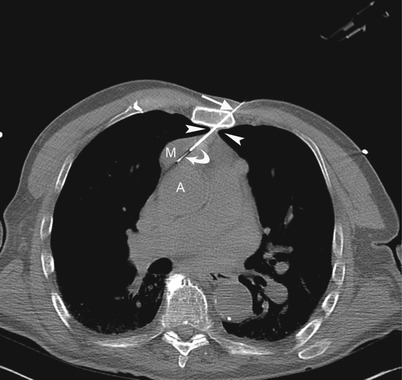
Fig. 10.13
Transsternal approach. A CT scan shows an 18-gauge needle (arrow) traversing the sternum and anterior mediastinal soft tissues and a 20-gauge core-biopsy needle (curved arrow) advanced through the 18-gauge needle into an anterior mediastinal mass (M) located anterior to the ascending aorta (A). Note that the anterior mediastinal soft tissues (arrowheads) do not extend laterally to allow parasternal extrapleural access
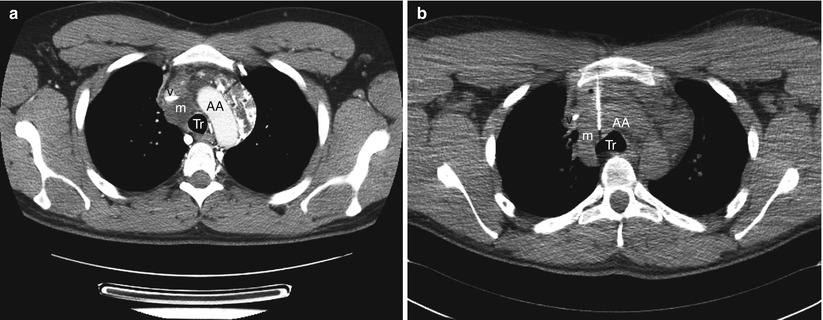
Fig. 10.14
Transsternal approach. (a) A contrast-enhanced CT scan shows a paratracheal mass (m) located anterolateral to the trachea (Tr) between the SVC (v) and aortic arch (AA). (b) A CT scan shows transsternal biopsy of the mass (m) with the biopsy needle passing between the superior vena cava (v) and the aortic arch (AA)
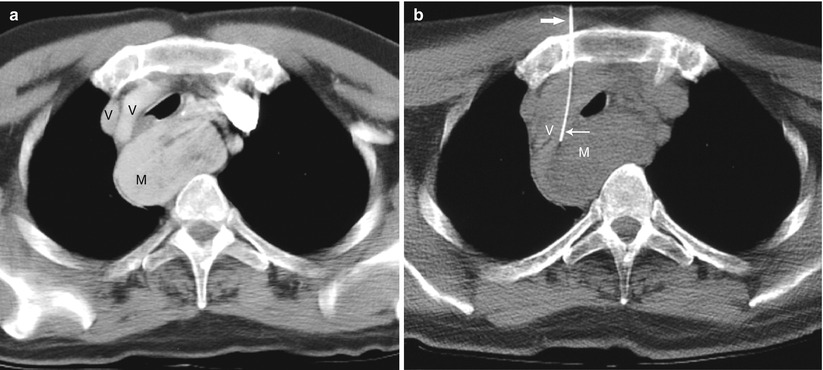
Fig. 10.15




Transsternal approach. (a) A contrast-enhanced CT scan shows a retrotracheal mass (M) posterior to the right and left brachiocephalic veins (V). (b) A CT scan shows a 22-gauge biopsy needle (thin arrow) coaxially introduced through an 18-gauge transsternal needle (thick arrow) and transgressing the left brachiocephalic vein (V) to obtain a sample of the mass (M)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree