Key Points
- •
The primary indications for performing bladder ultrasound at the bedside are estimation of bladder volume, confirmation of proper urinary catheter placement, detection of stones, and assessment of ureteral jets in suspected obstructive uropathy.
- •
Bladder volume can be calculated using the following formula: Volume = (0.75 × width × length × height).
- •
Detection of a bladder mass during a point-of-care ultrasound exam warrants further workup, including additional imaging and expert consultation.
Background
Bedside ultrasound evaluation of the bladder has several clinical applications. Estimation of bladder volume, confirmation of proper urinary catheter placement, detection of stones, and assessment of ureteral jets in suspected obstructive uropathy are the core indications for point-of-care bladder ultrasound.
Many patients who present with a complaint of “urinary retention” do not truly have urinary retention. Evaluation of bladder volume based on physical exam is inaccurate due to body habitus in a significant percentage of patients. Bladder ultrasound can precisely determine bladder volume and avoid unnecessary urinary catheterizations. When urinary catheterization is necessary, bedside ultrasound can confirm proper placement and functioning of the catheter. In pediatric patients, bladder volume estimation can eliminate unnecessary catheterizations, and real-time ultrasound guidance can substantially reduce complications associated with suprapubic bladder aspirations.
Normal Anatomy
The bladder is a triangular organ positioned in the pelvic cavity that is located inferior and anterior to the peritoneal cavity and directly posterior to the pubic symphysis ( Figure 21.1 ). Ureters enter the trigone of the bladder posteriorly and inferiorly ( Figure 21.2 ). In males, the prostate encircles the bladder neck caudally and normally measures <5 cm in transverse diameter.
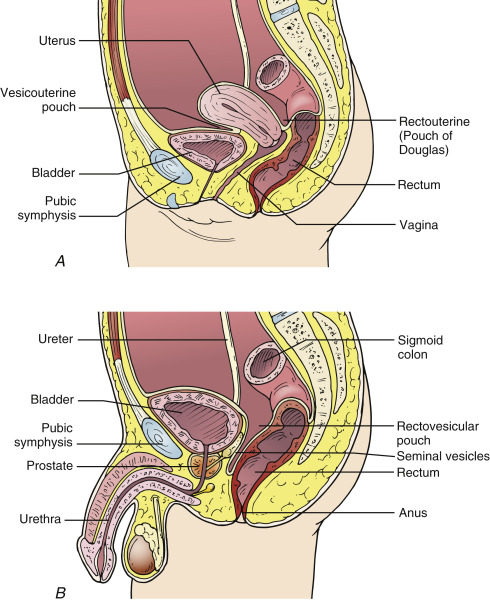
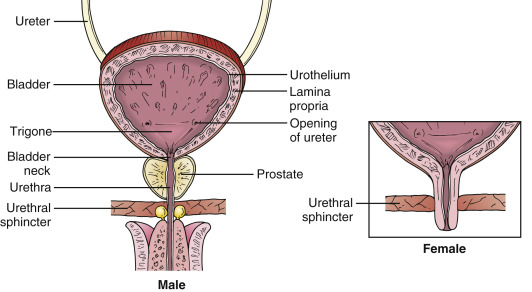
Image Acquisition
The curvilinear transducer (3.0–5.0 MHz) is ideal for imaging the bladder. Its mid-range frequency allows for optimal resolution, and its wider footprint permits visualization of the entire bladder. A fluid-filled bladder readily propagates sound waves resulting in posterior acoustic enhancement, or hyperechogenicity, posterior to the bladder. This artifact can obscure the far field of the image, and certain findings, such as pelvic free fluid, may be missed. The far-field gain should be decreased to better visualize hypoechoic or anechoic entities posterior to the bladder.
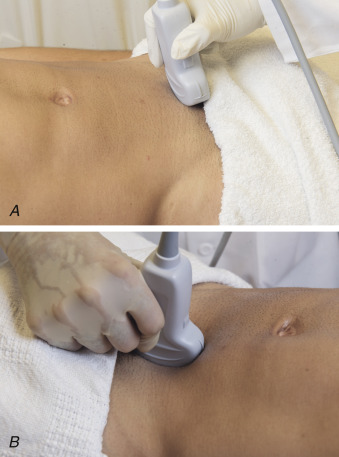
The bladder is located posterior and inferior to the pubic symphysis and is best visualized from a suprapubic approach. With the patient in a supine position, place the transducer in a transverse plane at the superior edge of the pubic symphysis and aim the ultrasound beam posteroinferiorly ( Figure 21.3 A ). Tilt the transducer superiorly and inferiorly to visualize the entire bladder in a transverse plane. Assess the bladder for its degree of distention and for the presence of stones or masses. If the bladder is not filled, the transducer often has to be pointed caudally into the pelvic cavity to identify the bladder. The prostate gland is hyperechoic and can be visualized in a transverse plane adjacent to the inferior bladder wall. Rotate the transducer 90 degrees clockwise to obtain longitudinal views of the bladder in a sagittal plane ( Figure 21.3 B). Scan the bladder thoroughly in a sagittal plane by tilting the transducer to visualize the leftmost and rightmost walls.
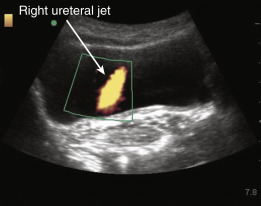
In patients with renal colic, visualization of ureteral jets, or intermittent expression of urine into the bladder, rules out complete obstruction of the ureter. To visualize ureteral jets, scan slowly through the bladder in a transverse plane and focus over the trigone. Ureteral jets can be detected using two-dimensional gray-scale sonography, but they are best visualized with power Doppler on a low-flow setting (i.e., low PRF setting). Power Doppler demonstrates flow regardless of direction and is particularly suited for detecting low-flow states, such as ureteral jets. The jets appear as colorful emissions streaming from the base of the bladder toward its center ( Figure 21.4 ). In well-hydrated patients, they appear at regular intervals every 15–20 sec and last <1 sec. The presence of bilateral ureteral jets in a well-hydrated patient rules out significant obstructive uropathy with high specificity. Ureteral obstruction is suspected when a jet is not visualized on the affected side but is visualized unilaterally on the unaffected side.
Pathologic Findings
Distended Bladder and Urinary Retention
Bladder volume can be calculated using the following formula :
Bladder volume = ( 0.75 × width × length × height )
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree