Key Points
- •
Pericardial effusion is common and can be accurately detected by providers of different specialties using point-of-care ultrasound.
- •
The clinical importance of a pericardial effusion can be synthesized from a combination of both clinical and ultrasound findings.
- •
Emergency pericardiocentesis guided by ultrasound can be a lifesaving procedure.
Background
Pericardial effusions are defined as the presence of fluid in the pericardial space that exceeds the upper physiologic amount of 50 mL and may be caused by malignancy, uremia, trauma, infection, and rheumatologic diseases. Although the incidence of pericardial effusions in the general population is not known, data suggest that up to 13.6% of patients with otherwise unexplained dyspnea presenting to emergency departments have pericardial effusions of varied clinical significance. Bedside ultrasound allows rapid, noninvasive diagnosis of pericardial effusion and acute pericardial tamponade. Physical exam findings, such as Beck’s triad (hypotension, jugular venous distention, and muffled heart sounds), although commonly emphasized, are not specific, and may be more reliable in trauma patients with a rapid accumulation of fluid. Few applications of emergency point-of-care ultrasound are more time critical and potentially lifesaving as cardiac ultrasound to detect pericardial tamponade. It is well documented that focused cardiac ultrasound can be learned by noncardiologists with different scopes of practice who can reliably diagnose pericardial effusions with >95% accuracy compared with comprehensive transthoracic echocardiography.
Image Interpretation
The pericardium is a dense, fibrous double-layered membrane that completely encircles the heart and a few centimeters of the aorta and pulmonary arteries. The dense parietal pericardial tissue is highly echogenic (bright white appearance on ultrasound) and is easily recognized both anteriorly and posteriorly as the sonographic border of the heart. The pericardial space is a blind sac contained within the visceral and parietal pericardium and usually contains a scant amount of pericardial fluid.
A normal heart contains approximately 10 mL of serous fluid in the pericardial sac. This small amount of fluid is occult on ultrasound, and the parietal and visceral layers of pericardium are seen as one hyperechoic layer adjacent to the myocardium in most views Pericardial effusions are seen on ultrasound as an anechoic (black) band that encircles the heart and separates the bright white, highly reflective parietal pericardium from the heterogeneous gray myocardium. Although a very small amount of fluid can be normal, distinguishing the origin (physiologic vs. pericardial disease) is not readily possible. In high-risk clinical circumstances where trivial effusions may be harbingers of important, evolving pericardial disease (e.g., penetrating trauma, postcardiac procedure), even a very small effusion should be considered pathologic until proven otherwise.
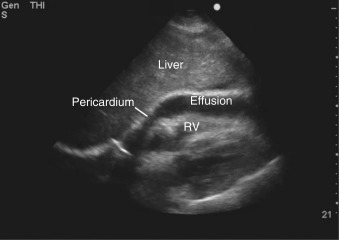
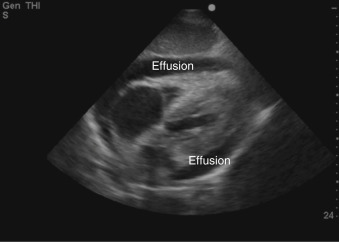
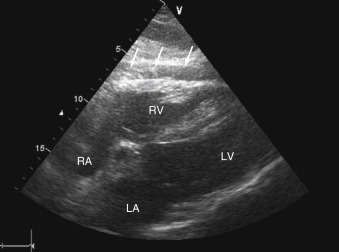
Free-flowing pericardial fluid initially accumulates posteriorly and is identified in the most dependent area of the pericardial sac. In the subcostal view, an effusion is seen as an anechoic stripe between the right ventricular free wall and pericardium adjacent to the liver ( Figure 17.1 and ![]() ). In the parasternal long-axis and short-axis views, pericardial effusions are seen posterior to the left ventricle ( Figure 17.2 and
). In the parasternal long-axis and short-axis views, pericardial effusions are seen posterior to the left ventricle ( Figure 17.2 and ![]() ). As the volume of pericardial fluid increases, an effusion becomes circumferential ( Figure 17.3 ). After cardiac surgery or percutaneous procedures, or in patients with recurrent pericardial disease, pericardial fluid may be loculated and does not flow freely with changes in patient position. Recognition of a loculated pericardial effusion is important because hemodynamic compromise can occur with even a small amount of located fluid.
). As the volume of pericardial fluid increases, an effusion becomes circumferential ( Figure 17.3 ). After cardiac surgery or percutaneous procedures, or in patients with recurrent pericardial disease, pericardial fluid may be loculated and does not flow freely with changes in patient position. Recognition of a loculated pericardial effusion is important because hemodynamic compromise can occur with even a small amount of located fluid.
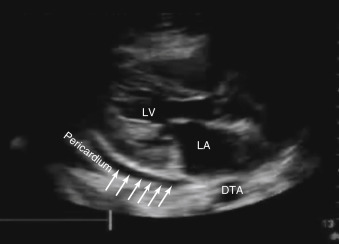
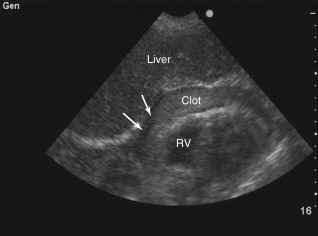
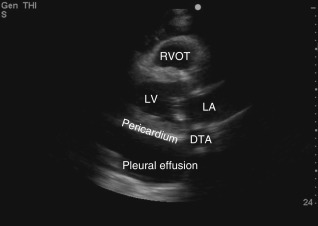
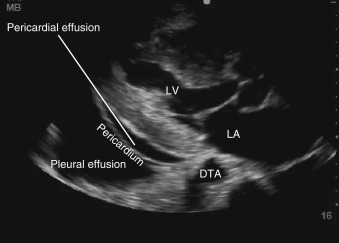
A number of conditions can mimic pericardial effusion and must be distinguished from true effusions. First, an epicardial fat pad, fatty tissue interposed between the two layers of pericardium, may be misdiagnosed as a pericardial effusion because they both appear anechoic and occupy the potential pericardial space. Fat can be distinguished from a true effusion based on its more gray or isoechoic appearance, rather than the anechoic appearance of an effusion. Also, nonloculated effusions typically collect dependently (posteriorly, in a supine patient), and if an anechoic space is seen only anteriorly, then it is most likely an epicardial fat pad ( Figure 17.4 and ![]() ). Effusions containing pus, fibrin, thrombus, or cellular debris from malignancy may appear more echogenic and can be overlooked as myocardium or adjacent lung tissue ( Figure 17.5 ). Second, a pleural effusion can be mistaken for a pericardial effusion. In a parasternal long-axis view, both effusions are seen as anechoic areas posterior to the left atrium and left ventricle but can be distinguished based on their relationship to the descending thoracic aorta (DTA). A pericardial effusion traverses anterior to the DTA, whereas a left pleural effusion is seen posterior to the DTA ( Figures 17.6 and 17.7 and
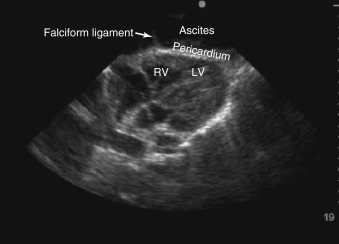
). Effusions containing pus, fibrin, thrombus, or cellular debris from malignancy may appear more echogenic and can be overlooked as myocardium or adjacent lung tissue ( Figure 17.5 ). Second, a pleural effusion can be mistaken for a pericardial effusion. In a parasternal long-axis view, both effusions are seen as anechoic areas posterior to the left atrium and left ventricle but can be distinguished based on their relationship to the descending thoracic aorta (DTA). A pericardial effusion traverses anterior to the DTA, whereas a left pleural effusion is seen posterior to the DTA ( Figures 17.6 and 17.7 and ![]() ). If the descending thoracic aorta is not well seen, an effusion should be confirmed from parasternal short-axis and subcostal views, or a dedicated left pleural view can also be obtained. Lastly, in certain views, providers must be vigilant not to mistake peritoneal fluid for pericardial fluid. Because the subcostal cardiac imaging plane crosses the upper abdomen, ascites may be misinterpreted as pericardial fluid in this view ( Figure 17.8 and
). If the descending thoracic aorta is not well seen, an effusion should be confirmed from parasternal short-axis and subcostal views, or a dedicated left pleural view can also be obtained. Lastly, in certain views, providers must be vigilant not to mistake peritoneal fluid for pericardial fluid. Because the subcostal cardiac imaging plane crosses the upper abdomen, ascites may be misinterpreted as pericardial fluid in this view ( Figure 17.8 and ![]() ). The absence of circumferential fluid around the heart, and acquiring corroborating cardiac and abdominal ultrasound views, can eliminate this pitfall.
). The absence of circumferential fluid around the heart, and acquiring corroborating cardiac and abdominal ultrasound views, can eliminate this pitfall.
Pathologic Findings
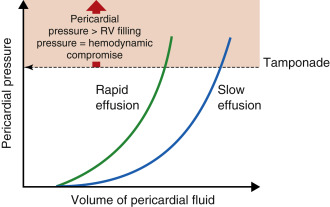
Hemodynamic effects of fluid in the pericardial space depend both on the volume and rate of fluid accumulation, as well as the patient’s intravascular volume status. A slowly expanding pericardial effusion (e.g., malignant effusion) can become quite large (>2000 mL) with little increase in pericardial pressure, whereas rapid accumulation of even a small volume of fluid (50–100 mL) can lead to a marked increase in pericardial pressure (e.g., myocardial perforation during placement of a pacemaker lead) ( Figure 17.9 ). Other important factors that determine the hemodynamic consequences of pericardial effusion include pericardial fluid characteristics (serous vs. blood), anatomic distribution (eccentric vs. concentric), integrity of the pericardial layers (inflamed, neoplastic invasion, fibrous), volume status of the patient, and size and thickness of the underlying cardiac chambers.
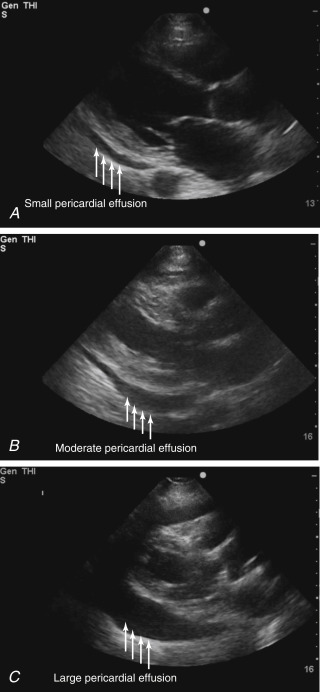
Pericardial Effusion (Small, Moderate, Large)
Several scales for quantifying the volume of a pericardial effusion have been described, but the assessment of these dimensions is subjective. Most commonly, the maximum fluid dimension measured in diastole allows for the following categorization ( Figure 17.10 ):
- 1.
Small: <1 cm (
 )
)
- 2.
Moderate: 1–2 cm (
 )
)
- 3.
Large: >2 cm (
 )
)