The radiological responses of bone to pathological process are limited; thus, similar x-ray signs occur in widely different conditions. It should be noted that it takes time for the various signs to develop. For example, in adults, it takes several weeks for a periosteal reaction to be visible after trauma and, in a child with osteomyelitis, the clinical features are present from 7 to 10 days before the first sign is visible on the radiograph. In general, the signs take longer to develop in adults than they do in children.
The signs of bone disease are summarized in Box 11.1.
- Decrease in bone density
- Increase in bone density
- Periosteal reaction
- Cortical thickening
- Alteration in trabecular pattern
- Alteration in the shape of a bone
- Alteration in bone age
- A decrease in bone density may be focal or generalized. Focal reduction in density is usually referred to as a ‘lytic area’ or an area of ‘bone destruction’. Generalized decrease in bone density is best referred to as ‘osteopenia’ until a specific diagnosis such as osteomalacia or osteoporosis can be made.
- An increase in bone density (sclerosis) may also be focal or generalized.
- The periosteum is not normally visible on a radiograph. The term ‘periosteal reaction’ refers to excess bone produced by the periosteum, which occurs in response to such conditions as neoplasm, inflammation or trauma. Several patterns of periosteal reaction are seen (Fig. 11.2), but they do not correlate with specific diagnoses. At the edge of a very active periosteal reaction there may be a cuff of new bone known as a Codman’s triangle (Fig. 11.2d). Although often seen in highly malignant primary bone tumours, e.g. osteosarcoma, a Codman’s triangle is also found in other aggressive conditions.
- Cortical thickening also involves the laying down of new bone by the periosteum (Fig. 11.3), but here the process is very slow. The result is that the new bone, although it may be thick and irregular, shows the same homogeneous density as does the normal cortex. There are no separate lines or spicules of calcification as seen in a periosteal reaction. The causes include chronic osteomyelitis, healed trauma, response to chronic stress or benign neoplasm. The feature common to all these conditions is that the process is either very slowly progressive or has healed.
- Alteration in trabecular pattern is a complex response usually involving a reduction in the number of trabeculae with an alteration in the remaining trabeculae, e.g. in osteoporosis and Paget’s disease. In osteoporosis, the cortex is thin and the trabeculae that remain are more prominent than usual, whereas in Paget’s disease the trabeculae are thickened and trabeculation is seen in the normal compact bone of the cortex (Fig. 11.4).
- Alteration in the shape of a bone is another complex response with many causes. Many cases are congenital in origin; some are acquired, e.g. acromegaly and expanding bone tumours.
- Alteration in bone age. The time of appearance of the various epiphyseal centres and their time of fusion depends on the age of the child. For the measurement of ‘bone age’, a film of one hand and wrist is taken and compared with a set of standard films, which provides an indication of skeletal maturity.
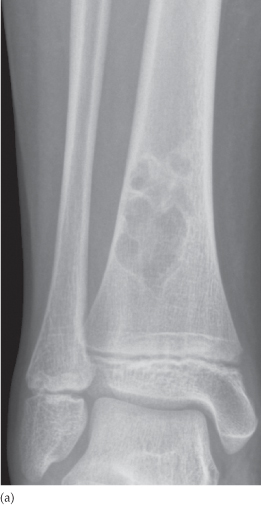
Fig. 11.2 Different types of periosteal reactions. (a) Smooth, lamellar, periosteal reaction on the radius and ulna in a case of non-accidental injury. (b) Spiculated (sunray) periosteal reaction in a case of osteogenic sarcoma (arrows). (c) ‘Onion skin’ periosteal reaction in a case of Ewing’s sarcoma (arrows). Here the periosteal new bone consists of several distinct layers. (d) Codman’s triangle in a case of osteogenic sarcoma. At the edge of the lesion the periosteal new bone is lifted up to form a cuff (arrow).
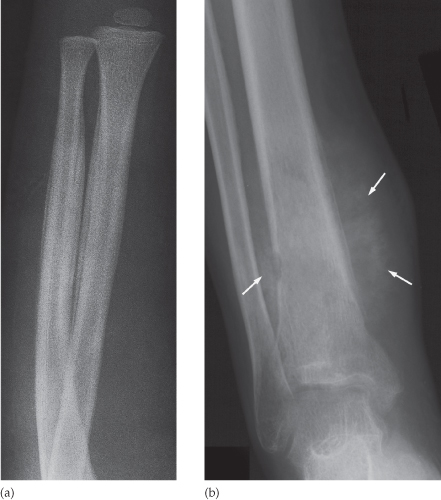
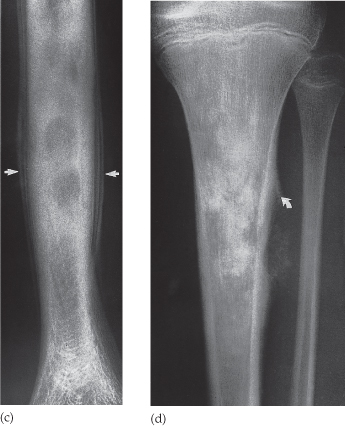
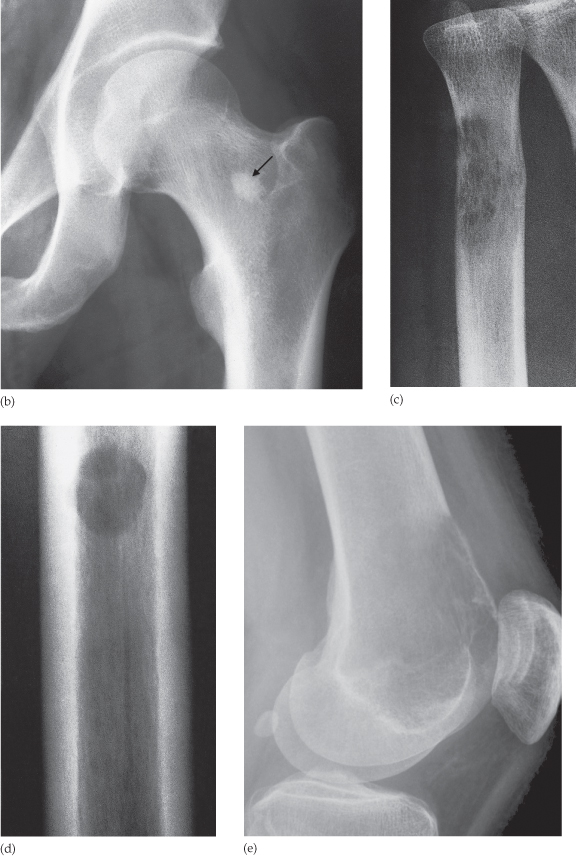
Fig. 11.3 Cortical thickening. Note the thickened cortex in the midshaft of the tibia from old, healed osteomyelitis. Same patient as in Fig. 11.19a,b taken 1 year later.

Fig. 11.4 Alteration of trabecular pattern in Paget’s disease involving the upper part of the tibia, leaving the lowest part of the tibia and the fibula unaffected. Note the coarse trabeculae. The other features of Paget’s disease – thickened cortex and bone expansion – are also present.

Ultrasound in Musculoskeletal Disease
Ultrasound cannot evaluate bone pathology but does have a complementary imaging role in the following:
- in detecting tenosynovitis, tendon tears and rupture (Fig. 11.5)
- in the diagnosis of osteomyelitis.
Fig. 11.5 Achilles tendon rupture. (a) The normal tendon shows a fibrillary pattern. (b) There is disruption of the fibrillary pattern due to a rupture of the tendon. The hypoechoic area (*) is due to a haematoma.

Radionuclide Bone Imaging
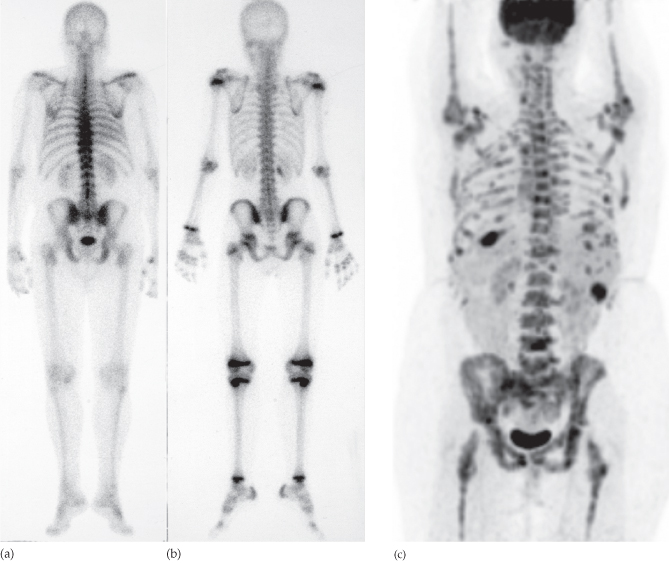
Technetium-99m (99mTc) labelled phosphate complexes given as an intravenous injection are the agents used for bone scintigraphy. They are taken up selectively by the bones (Fig. 11.6) and are also excreted in the urine. These agents may be concentrated by certain soft tissue tumours, by soft tissue calcifications and by sites of tissue damage.
Fig. 11.6 (a,b) Normal radionuclide bone scan. (a) Adult. Note the radionuclide in the bladder. (b) Child. Note the bands of increased uptake in the epiphyseal plates where bone growth is occurring. (c) FDG-PET/CT demonstrates multiple, metabolically active bone metastases in a patient with breast cancer.
Increased uptake on the radionuclide bone scan is seen in conditions where there is an increased blood supply and high bone turnover with new bone formation. Many bone abnormalities – including fractures, benign or malignant tumours, infection, infarction and Paget’s disease – give positive scans, so correlation with plain radiographs is usually essential. The indications for technetium bone scanning are given in Box 11.2.
- Detection of metastases
- Detection of osteomyelitis
- Determination of whether a lesion is solitary or multifocal
- Investigation of a clinically suspected bone lesion despite a normal radiograph:
- metastases
- trauma (particularly stress injury)
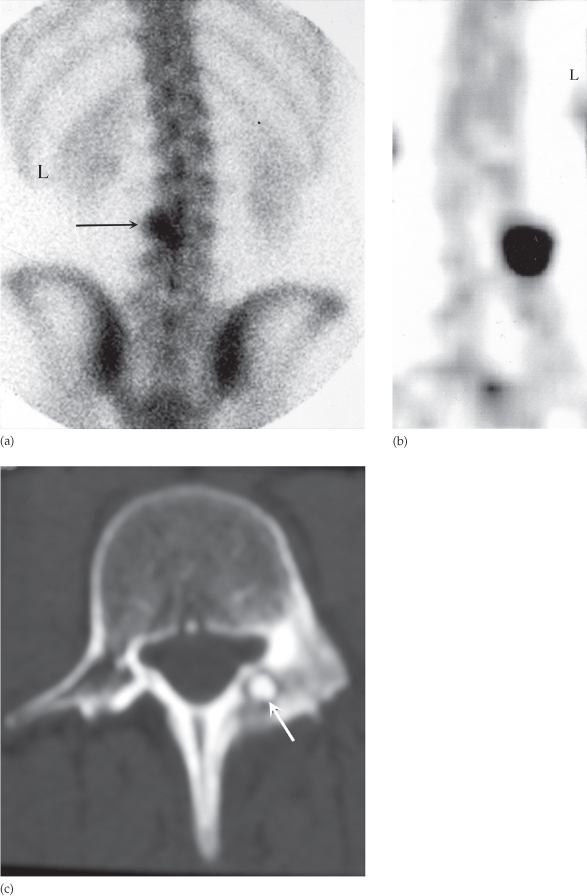
- osteoid osteoma (Fig. 11.7)
- early osteomyelitis
- metastases
- Determination, in equivocal cases, of whether an abnormality seen on the radiograph is significant or not (a positive bone scan makes it likely that a true lesion exists and a negative one reduces the probability of disease considerably)
- Investigation of painful joint prostheses
Fig. 11.7 Osteoid osteoma that was not visible on plain films. (a) Bone scan (posterior view) showing a focal area of intense increased uptake in L3 (arrow). L, left. (b) Single photon emission computed tomography (SPECT) scan showing the increased uptake more clearly. (c) CT demonstrating the tumour arising in the pedicle (arrow).
Fluorodeoxyglucose positron emission tomography (FDG-PET) with computed tomography (CT) may be used to demonstrate bone metastases (Fig. 11.6c). However, this would normally only be done in preference to technetium bone scan if other sites of disease were being evaluated. It is recognized that some benign bone lesions take up FDG to the same extent as some primary malignant bone tumours.
Computed Tomography in Bone Disease
Plain radiographs are usually very informative, however CT is needed in selected cases, particularly in the detection of subtle fractures or in complex fractures (Box 11.3). Bone window settings (see Chapter 1) should always be viewed when reporting CT of the brain, chest and abdomen.
- Demonstration of abnormalities in the spine, pelvis and hips (Fig. 11.8) where plain films are frequently difficult to interpret
- Three-dimensional reconstructions can be made of fractures, which are particularly useful in showing the fractures and position of the fragments and for planning corrective surgery
- Demonstration of the extent and characterization of bone tumours in selected cases to complement MRI
- As a guide for bone biopsy
Fig. 11.8 CT scan of a pelvis showing a large mass (arrows) due to a metastasis destroying the medial half of the right iliac bone with extension into the adjacent soft tissues.

Magnetic Resonance Imaging in Bone Disease
Magnetic resonance imaging (MRI) has come to play a vitally important role in musculoskeletal disorders (Box 11.4). Calcified tissues such as bone produce no signal with MRI, but MRI can demonstrate the bone marrow, making it possible to see the extent of disease such as metastases, other tumours and infections, even in areas where bone destruction is not yet evident on plain films or CT (Fig. 11.9). MRI is also particularly good for showing soft tissue abnormalities.
- Demonstration of disc herniation and spinal cord or nerve root compression
- Diagnosis of bone metastases
- To show the extent of primary bone tumours
- Demonstration of myeloma and lymphoma (Fig. 11.9)
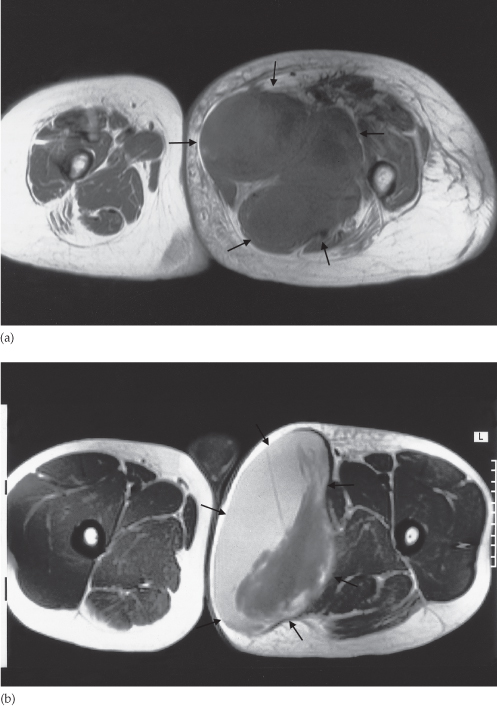
- To image soft tissue masses (Fig. 11.10)
- Diagnosis of osteomyelitis and to show any soft tissue abscess
- Diagnosis of avascular necrosis and other joint pathologies
- To image both acute and chronic injury to joint cartilages, ligaments and other intra-articular soft tissues
Fig. 11.9 MRI of bone tumours. (a) T1-weighted post contrast scan of osteosarcoma in the lower shaft and metaphysis of the left femur. The extent of tumour (arrows) within the bone and the soft tissue extension are both very well shown. The low signal in the medulla (*) is due to the calcified osteogenic component of the tumour. (b) The true extent of the tumour cannot be assessed from a plain film, although the plain film provides a more specific diagnosis, because the bone formation within the soft tissue extension (arrows) is obvious. (c) T2-weighted scan of lymphoma in the T10 vertebral body (arrow). The very high signal of the neoplastic tissue is evident even though there is no deformity of shape of the vertebral body.
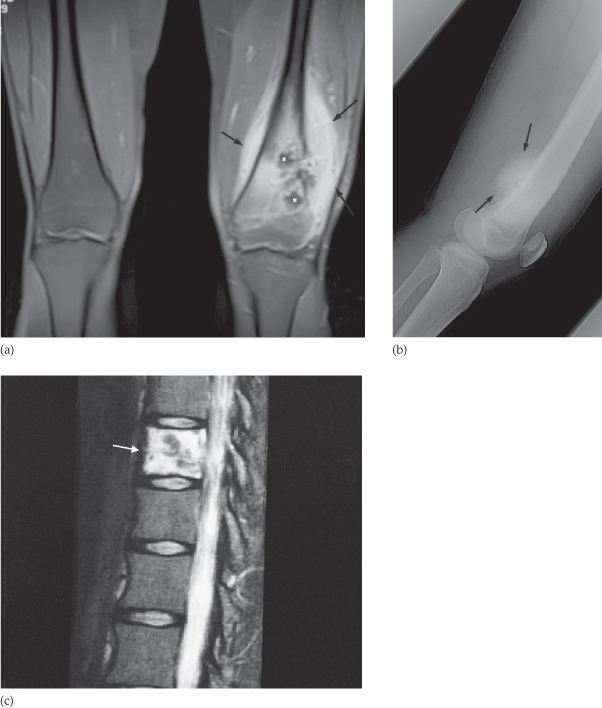
Fig. 11.10 T1-weighted MRI of soft tissue masses. (a) Soft tissue sarcoma producing an obvious soft tissue mass (arrows) in the medial compartment of the left thigh. (b) Large haematoma (arrows) in the medial compartment of the left thigh showing a mixed signal, including the characteristic high signal of recent haemorrhage on a T1-weighted sequence.
Bone Disease Diagnosis
When considering the diagnosis and differential diagnosis of bone diseases, it is convenient to divide disorders into four main groups:
Fractures are dealt with separately in Chapter 14.
Solitary Lesions
Solitary areas of lysis, sclerosis or a combination of the two, are usually one of the following:
- bone tumour:
- malignant (primary or secondary)
- benign
- malignant (primary or secondary)
- osteomyelitis
- bone cyst, fibrous dysplasia or other non-neoplastic defect of bone
- conditions of uncertain nature such as Langerhans’ histiocytosis and osteoid osteoma.
Primary malignant bone tumours and osteomyelitis are usually accompanied by periosteal reaction. Pathological fractures may be seen through benign and malignant bone tumours and through bone cysts.
The radiological diagnosis of a localized bone lesion can difficult. Some conditions are readily diagnosed but, in others, even establishing which broad category of disease is present can be difficult. The initial radiological decision is usually to try and decide whether the lesion is benign (i.e. stable or very slow growing) or whether it is aggressive (i.e. a malignant tumour or an infection). It is also important to know the age of the patient, as certain lesions tend to occur in a specific age range.
The following features should be looked for on plain radiographs and CT when trying to decide the nature of a localized bone lesion.
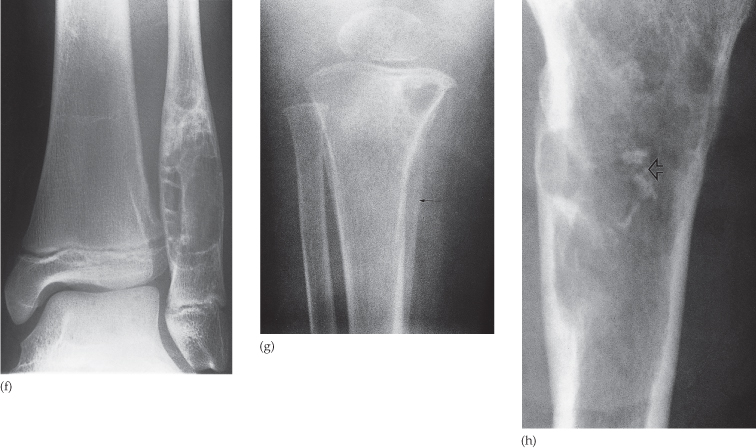
Fig. 11.11 Localized lesions. (a) A well-defined sclerotic edge can be seen indicating a benign lesion – a fibrous cortical defect. (b) (Opposite) Bone island. There is a small, well-defined area of compact bone in the neck of the femur (arrow). This common finding is without significance. (c) An ill-defined edge – in this case a metastasis. This type of bone destruction is known as permeative. (d) A well-defined edge – in this case a metastasis in the shaft of the femur. (e) Destruction of the cortex indicating an aggressive lesion – another metastasis. (f) Expansion of the cortex due to fibrous dysplasia. (g) Periosteal reaction (arrow) – in this case osteomyelitis. (h) A lesion containing calcium (arrow) due to a cartilage tumour – in this case a chondrosarcoma.
- Osteomyelitis
- Malignant bone tumour, particularly Ewing’s sarcoma and osteosarcoma
- Occasionally metastasis, particularly neuroblastoma
- Langerhans’ histiocytosis
Bone Tumours
The precise diagnosis of a bone tumour can be notoriously difficult both for the radiologist and the pathologist. Accurate histological diagnosis is essential for all malignant lesions and it is important to realize that separate portions of a tumour may show different histological appearances. In general, plain film radiography is the best imaging technique for making a diagnosis, whereas MRI or CT delineate the full extent of a tumour to advantage and show the effects on surrounding structures and the relationship to the neurovascular bundle. The main role for radionuclide bone scanning is to diagnose metastatic bone disease. Metastatic malignant tumours are by far the commonest bone neoplasm, outnumbering by many times primary malignant tumours. They are discussed later in the chapter.
Primary Malignant Tumours
On plain films, primary malignant tumours usually have poorly defined margins, often with a wide zone of transition between the normal and abnormal bone. The lesion may destroy the cortex of the bone. A periosteal reaction is often present and a soft tissue mass may be seen.
Radionuclide bone scans show substantially increased activity in the lesion.
MRI is the most accurate technique for showing the local extent of the tumour using multiplanar views. Extension into both the medullary cavity and the soft tissues can be accurately defined, as can the relationship to important nerves and blood vessels.
Osteosarcoma (osteogenic sarcoma) (see Fig. 11.9) occurs mainly in the 5–20-year-old age group, but is also seen in the elderly following malignant change in Paget’s disease. The tumour often arises in a metaphysis, most commonly around the knee. There is usually bone destruction with new bone formation, and typically a florid, spiculated periosteal reaction is present, the so-called ‘sunray appearance’ (see Fig. 11.2b). The tumour may elevate the periosteum to form a Codman’s triangle (see Fig. 11.2d).
Chondrosarcoma
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree