Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) is widely used for joint imaging, allowing clear definition of the joint anatomy and the detection of abnormal fluid, change in signal intensity or enhancement. It is widely used for
- meniscal and ligamentous tears (e.g. in the knee)
- rotator cuff tears of the shoulder
- avascular necrosis of the hip
- septic arthritis.
Normal tendons are clearly defined, smooth and return no signal and therefore appear black on MRI sequences. In tendon degeneration or ligament sprain, the tendon may have increased signal intensity, altered size (usually increased), irregular margins or abnormal shape. There may be fluid around the ligaments or the fibres may be disrupted. In the knee, the normal menisci appear as black triangles on MRI. A meniscal tear can be seen when either the normal shape of the meniscus is disrupted by an abnormal signal, or if a portion of the meniscus is missing.
The normal synovium is only a thin membrane, and it is therefore invisible to MRI. Synovial proliferation is the hallmark of rheumatoid arthritis. Enhancement of thickened, inflamed synovium following intravenous contrast is the key to an early diagnosis of non-invasive rheumatoid arthritis.
Arthrography
Arthrography involves injecting contrast medium into the joint space directly and then performing a magnetic resonance scan. Magnetic resonance arthrography has a role in the shoulder and wrist.
Ultrasound
Ultrasound is used to image the soft tissues of joints and is also used to inject local anaesthetic and steroid solutions to treat inflammatory conditions. Several joints are amenable to imaging on ultrasound, including the shoulder and joints of the arm, wrist and hand, knee, ankle and foot.
On ultrasound, a normal tendon or ligament is a bright/echogenic linear band of varying thickness depending on its location. Normally, the collagen fibres are continuous and intact. The possible findings one should look for are: changes in echogenicity, increase in size of tendon, fluid in the joint and irregularity of bone surface.
When interruptions in ligament or tendon fibres exist, they are visualized as anechoic/black areas within the tendon. Partial thickness tears reveal fibrous disruption, while full thickness tears demonstrate tendon gaps. High grade, partial thickness tearing is imaged as tendon thinning. Enlarged, hypoechoic tendons with normal echotexture may be due to low grade injuries, intratendinous oedema or tendinopathy. In a normal joint, the bursa is a thin, black/anechoic line which is less than 2 mm thick. The bursa fills with fluid when irritated or infected.
Arthritis
Signs Indicating the Presence of Arthritis
Joint space narrowing is due to destruction of articular cartilage. It occurs in practically all forms of joint disease except avascular necrosis.
Soft tissue swelling around a joint may be seen in any arthritis accompanied by a joint effusion and whenever periarticular inflammation is present. It is, therefore, a feature of inflammatory, and particularly infective, arthritis. Discrete soft tissue swelling around the joints can be seen in gout due to gouty tophi.
Osteoporosis of the bones adjacent to joints occurs in many painful conditions. Underuse of the bones seems to be an important mechanism, but is not the only factor. Osteoporosis is particularly severe in rheumatoid and tuberculous arthritis.
Signs That Point to the Cause of Arthritis
An articular erosion is an area of destruction of the articular cortex and the adjacent trabecular bone (Fig. 12.2), usually accompanied by destruction of the articular cartilage. Erosions are easily recognized when seen in profile, but when viewed en face the appearances can be confused with a cyst. Oblique views designed to show erosions in profile are often taken.
Fig. 12.2 Erosions. Areas of bone destruction are seen affecting the articular cortex of the metacarpophalangeal joint. A typical erosion is arrowed. The joint space is also narrowed.

There are several causes of erosions (Box 12.1).
- Inflammatory overgrowth of the synovium (pannus), which occurs in:
- rheumatoid arthritis, by far the commonest cause of an erosive arthropathy
- juvenile rheumatoid arthritis (Still’s disease)
- psoriasis
- Reiter’s disease
- ankylosing spondylitis
- tuberculosis
- rheumatoid arthritis, by far the commonest cause of an erosive arthropathy
- Response to the deposition of urate crystals in gout
- Destruction caused by infection:
- pyogenic arthritis
- tuberculosis
- pyogenic arthritis
- Synovial overgrowth caused by repeated haemorrhage in haemophilia and related bleeding disorders
- Neoplastic overgrowth of synovium, e.g. synovial sarcoma
Osteophytes, subchondral sclerosis and cysts are all features of osteoarthritis. A characteristic increase in the density of subchondral bone is seen in avascular necrosis (see Figs 12.15 and 12.16).
Several conditions lead to characteristic alterations in the shape of the joint or relationship of the bone ends, e.g. slipped epiphysis, developmental dysplasia of the hip, osteochondritis dissecans and avascular necrosis in its later stages.
Diagnosis of Arthritis
When considering an arthritis it is important to have the following information:
- Rheumatoid arthritis virtually always involves the hands and feet, principally the metacarpo- and metatarsophalangeal joints, the proximal interphalangeal joints and the wrist joints. Psoriatic arthritis usually affects the terminal interphalangeal joints.
- Gout characteristically involves the metatarsophalangeal joint of the big toe.
- When osteoarthritis is seen in the hands it almost always involves the terminal interphalangeal joints and often affects the carpometacarpal joint of the thumb. In the feet, it is almost always the first metatarsophalangeal joint that is affected. In the large joints, osteoarthritis is common in the hips and knees but relatively rare in the ankle, shoulders and elbows unless there is some underlying deformity or disease.
- The distribution of neuropathic arthritis depends on the neurological deficit; for example, diabetes affects the ankles and feet, whereas syringomyelia affects the shoulders, elbows and hands.
Rheumatoid Arthritis
Rheumatoid arthritis is a polyarthritis caused by inflammatory overgrowth of synovium known as pannus.
The earliest change is periarticular soft tissue swelling and osteoporosis. This osteoporosis is believed to be due to a combination of disuse and synovial hyperaemia. Destruction of the articular cartilage by pannus leads to joint space narrowing and to small bony erosions which occur, initially, at the joint margins (Fig. 12.3). These erosions are often seen first around the metatarso- or metacarpophalangeal joints, proximal interphalangeal joints and on the styloid process of the ulna. Later, extensive erosions may disrupt the joint surfaces. Ulnar deviation is usually present at this stage. With very severe destruction, the condition is referred to as arthritis mutilans (Fig. 12.4).
Fig. 12.3 Early rheumatoid arthritis. Small erosions are present in the articular cortex (arrows) and there is soft tissue swelling around the proximal interphalangeal joints.

Fig. 12.4 Advanced rheumatoid arthritis (arthritis mutilans). There is extensive destruction of the articular cortex of the metacarpophalangeal joints with ulnar deviation of the fingers. Fusion of the carpal bones and wrist joint has occurred.

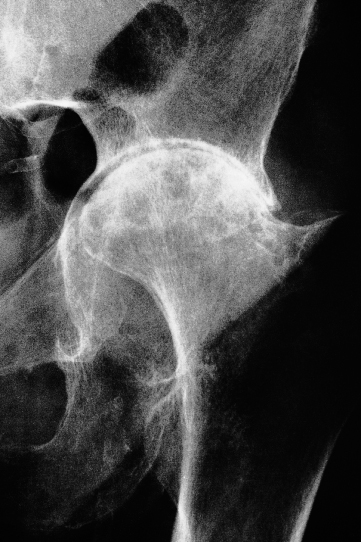
Similar changes are seen in the large joints (Fig. 12.5). In such cases, osteoarthritis may be superimposed on the rheumatoid arthritis and may dominate the picture.
Fig. 12.5 Rheumatoid arthritis. Uniform loss of joint space is seen in this hip joint. Sclerosis is also present due to associated osteoarthritis.
With severe disease, there may be subluxation at the atlantoaxial joint (Fig. 12.6) due to laxity of the transverse ligament, which holds the odontoid peg against the anterior arch of the atlas. Atlantoaxial subluxation may only be demonstrable in a film taken with the neck flexed. Even though it is frequently asymptomatic, there is always the possibility of neurological symptoms from compression of the spinal cord by the odontoid process and it is important to be aware of its existence if the patient is to have a general anaesthetic. Atlantoaxial instability can be well demonstrated with MRI.
Fig. 12.6 Rheumatoid arthritis – atlantoaxial subluxation. C1 is displaced anteriorly upon C2. The distance between the arch of the atlas and the odontoid peg (arrow) is increased from the normal value (2 mm) to 8 mm. This is the same patient whose hand is illustrated in Fig. 12.4.

Role of Radiology in Rheumatoid Arthritis
Radiographs assist in the diagnosis of doubtful cases. To this end, the detection of erosions is extremely helpful. A widespread erosive arthropathy is almost diagnostic of rheumatoid arthritis. Radiographs are also useful in assessing the extent of the disease and in observing the response to treatment.
Other Erosive Arthropathies
A number of other arthropathies, such as juvenile rheumatoid arthritis and the HLA-B27 spondyloarthropathies, which include psoriasis and Reiter’s disease, produce articular erosions.
Juvenile rheumatoid arthritis (Still’s disease, juvenile chronic polyarthritis) shows many features similar to rheumatoid arthritis but erosions are less prominent. The knee, ankle and wrist are the joints most commonly affected. Hyperaemia from joint inflammation causes epiphyseal enlargement and premature fusion.
In psoriasis, there is an erosive arthropathy with predominant involvement of the terminal interphalangeal joints (Fig. 12.7).
Fig. 12.7 Psoriatic arthropathy. There are extensive erosive changes affecting the interphalangeal joints but sparing the metacarpophalangeal joints.

Gout
In gout, the deposition of urate crystals in the joint and in the adjacent bone gives rise to an arthritis that most commonly affects the metatarsophalangeal joint of the big toe.
The earliest change is soft tissue swelling. At a later stage, erosions occur that, unlike rheumatoid arthritis, may be at a distance from the articular cortex. These erosions have a well-defined, often sclerotic, edge and frequently have overhanging edges (Fig. 12.8a). They are due to urate deposits in the bone. These deposits may be very large, causing extensive bony destruction. There is usually no osteoporosis.