Fig. 17.1
Scheme of the three types of stress that act on bowel and mesentery in abdominal blunt trauma
Crushing may determine local lacerations of the bowel wall and mesentery, mural and mesenteric hematomas, localized devascularization, and full-thickness contusions. Susceptibility to crush injuries increases with age, in relation to the relaxation of abdominal musculature. Because of their anatomical features (close contact to the spine), the duodenum and transverse colon are particularly susceptible to this type of injury [17], which are often caused by seat belt, steering wheel or, mostly in pediatric age, bicycle handlebar.
Shearing forces can lead to bowel lacerations, mesenteric tears, and interruption of the mesenteric vessels. Points of anatomical fixity, or intestinal segments close to acquired fixity points, such as bridles and adhesions, are more susceptible to these injuries.
The presence of a “seat belt mark” sign, characterized by patterned ecchymosis or abrasion across the patient’s abdominal wall, correspondent to the position of the diagonal or horizontal strap of the seat belt, is considered a reliable predictor of bowel injury [11, 18]. A radiologic seat belt sign, consisting of increased attenuation in the subcutaneous fat over the abdomen, has been described [16]. At impact, the seat belt compression may close off the bowel, causing a sudden increase of the intraluminal pressure in the “closed loop” that may result in bursting injuries. When the intraluminal pressure reaches 120–140 mmHg, either a single perforation or multiple small perforations of the bowel wall can occur, usually on the antimesenteric border of the loop [15, 16]. Requiring less energy to occur than injuries from the crush and shearing mechanisms, burst lesions are therefore more likely to be isolated (not associated with other injuries) [16]. Pre-existing pathological conditions, such as ileus, Crohn disease, and bowel obstruction, predispose the bowel to this type of injury.
17.3 Anatomo-Pathological Considerations
The small bowel is the most often injured intestinal tract (70%) in blunt abdominal trauma. As already mentioned, intestinal tracts close to fixed point of attachment, such as proximal jejunum near the ligament of Treitz and distal ileum near the ileocecal valve, where mobile and fixed portions of the gut are contiguous, are particularly exposed to damage [19, 20].
The colon accounts for 20% of intestinal traumatic injuries. The ascending and descending colon, fixed and partially retroperitoneal, are generally susceptible to more severe injuries compared to the more mobile transverse and sigmoid colon. Injuries to the right colon are always associated with multiple injuries elsewhere, reflecting the high-energy dissipation required to inflict them [21, 22] (Fig. 17.2). The sigmoid colon is at risk of closed loop perforation. Due to its exposed location, the transverse colon is reported to be the most vulnerable portion of the large bowel, but its relative mobility accounts for the minor entity of most injuries at this site.


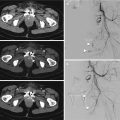
Fig. 17.2
High-energy blunt abdominal trauma. Axial CT images show rib fractures (curved arrow in a), hemoperitoneum (arrow in a) and hepatic contusion (arrowhead in a), devascularization of the right kidney (arrow in b), mesenteric hematoma (arrowhead in c) with contrast material extravasation (active bleeding) (arrow in c), and unenhanced ascendant colon wall (arrow in d)
Duodenum represents the intestinal tract less frequently involved in blunt trauma (10%). Its anatomical features (mainly retroperitoneal organ, in direct contact with the thoracic spine) explain the peculiarity of diagnostic findings in cases of perforation and the frequent association with pancreatic injury.
Injuries to the appendix, stomach, and rectum are extremely uncommon. Rectum injuries are often associated with major pelvic fractures.
The site of damage correlates well with prognosis, accounting the amount and quality of bowel content, which is less enzymatically active and has low pH and bacterial counts in case of small bowel lesions and more contaminating in case of colonic lesions. Intraperitoneal blood is a minor peritoneal irritant.
Bowel and mesenteric injuries are frequently associated with abdominal solid organ lesions [23] or spine and pelvic bones fractures [24].
The management of bowel and mesenteric traumatic injuries depends on the location and the type of damage. Surgical treatment is not always necessary and depends on the relevance of the lesion: major and minor injuries can be distinguished (Table 17.1). Surgically significant injuries, or “major” lesions, include a complete tear of the bowel, devascularized bowel, active mesenteric bleeding, and mesenteric injury associated with bowel ischemia.
Table 17.1
Bowel and mesentery major and minor injuries
Bowel | Mesentery |
|---|---|
Significant (major) injuries | |
Complete tear of the bowel wall | Active bleeding |
Bowel ischemia | Mesentery disruption |
Mesenteric injury with bowel ischemia | |
Not significant (minor) injuries | |
Serosal tear of the bowel wall | Mesenteric hematoma (no bleeding) |
Bowel hematoma | Mesenteric stranding |
Minor injuries include serosal tear of the bowel wall, bowel hematoma, mesenteric hematoma without active bleeding and mesenteric stranding; these conditions can be managed conservatively.
17.4 The Role of MDCT
Since diagnosis based on clinical findings has low sensitivity and is often unreliable, a set of diagnostic tools has been used to evaluate patients in whom abdominal injury is suspected, including DPL, FAST scan, and CT [4, 25].
DPL, traditionally used in several countries, is fairly sensitive (90%) for the detection of hemoperitoneum, but has several limitations: it is poorly specific in assessing the site and the extent of the damage, it is not reliable in detecting retroperitoneal injuries and, like any invasive procedure, it carries some risk of iatrogenic injuries [4, 10]. The use of results of DPL as the sole indication for surgery has led to a high nontherapeutic laparotomy rate.
FAST scan has a great sensitivity (86%) for the detection of free intra-abdominal fluid, but is nonspecific with regard to organ injury [4].
With a wide range of reported values for sensitivity and specificity (between 80–95% and 48–99%, respectively) [26], the accuracy of CT for detection of intestinal and mesenteric injuries due to blunt trauma has long been controversial. Until the 2000s, surgical literature described CT as unreliable in distinguishing surgical from not-surgical bowel and mesenteric injuries. The recent introduction of MDCT significantly decreased the time taken to perform the examination, decreased the motion artifacts, and improved the blood vessel opacification and solid organ enhancement. Providing a wide spectrum of findings suggestive of bowel and mesenteric injuries, MDCT is more sensitive and specific than DPL, FAST scan, and clinical examination [19]. Owing to the great advances in CT technology and improvement in interpretation, MDCT has currently become the diagnostic tool of choice in the evaluation of blunt abdominal trauma in hemodynamically stable patients [6, 27].
17.5 MDCT Technique
All MDCT examinations must be performed with a high-resolution protocol, with reconstruction interval values equals to 1 mm, and completed with coronal and sagittal multiplanar reconstruction in the post-processing elaboration.
The acquisition of pre-contrast CT abdomino-pelvis scans is useful to identify free air collections, to detect abnormal attenuation of mesenteric fat, and to assess the attenuation values of any fluid collection and/or of the bowel wall.
A biphasic study in arterial and venous phase after the intravenous infusion of 120–150 ml of iodinated contrast material at an adequate rate (≥3 ml/s) is indicated to detect active bleeding and identify perfusion abnormalities in the bowel loops. In suspicious of low-flow vascular active bleeding, a delayed phase (3–5 min) may be added to the examination [11, 28].
Many investigators have proven that administration of oral contrast material is not routinely required in the MDCT evaluation of patients with blunt abdominal trauma [4, 29–31]. Being time-consuming, oral contrast material administration increases the risk of vomiting and aspiration without improvement of diagnostic capability [32].
17.6 MDCT Findings of Intestinal and Mesenteric Injury
According to surgical and prognostic criteria, traumatic injuries of the bowel and mesentery can be classified into “major” and “minor.” Major lesions, including bowel perforation, active mesenteric bleeding, and mesenteric injury associated with bowel ischemia, require a surgical treatment. If unrecognized, these injuries may result in high morbidity and mortality, related to sepsis or hemorrhage. Minor lesions, including bowel wall tear limited to the serosa, bowel wall hematoma, and mesenteric hematoma without active bleeding, can be treated conservatively.
Currently, there are several recognized CT features of blunt bowel and mesenteric injury (Tables 17.2 and 17.3). Based on radiological criteria, we distinguish specific (direct) and nonspecific (indirect) bowel and mesenteric injury signs. Getting familiar with the appearance of specific and nonspecific signs is crucial to making a prompt and accurate diagnosis [4].
Table 17.2
MDCT signs of bowel injury
Specific (direct signs) | Nonspecific (indirect signs) |
|---|---|
Bowel wall discontinuity | Bowel wall thickening |
Extraluminal air | Abnormal bowel wall enhancement |
Intramural air | Intraperitoneal/retroperitoneal fluid |
Table 17.3
MDCT signs of mesenteric injury
Specific (direct signs) | Nonspecific (indirect signs) |
|---|---|
Active bleeding | Mesenteric infiltration |
Beading/termination of mesenteric vessels | Intraperitoneal fluid (mesenteric fluid collections) |
Mesenteric hematoma |
17.7 MDCT Findings of Bowel Injury
17.7.1 Bowel Wall Discontinuity
Detection of a discontinuous bowel wall is the most specific sign of bowel injury, with 100% specificity [4]. However, this finding is extremely uncommon on MDCT images and it has a very low sensitivity (5–10%) [23]. The relative infrequency of direct visualization of bowel perforation is mainly due to the small size of discontinuities [4]. The type of lesion may also influence the possibility of detection: blowout perforations are harder to identify on CT than lacerations because of the collapsing, cockade shaped, margins of the small hole. Site of perforation is important as well: a lesion occurring on the antimesenteric equatorial border of the loop may be easier to identify on axial scans (Fig. 17.3); lesions involving the superior or inferior wall will be better detected on multiplanar reconstruction. Lesions of the bowel wall are better depicted in the portal venous phase scan [11]. The distribution of free air may be useful in localizing the point of bowel rupture [28].
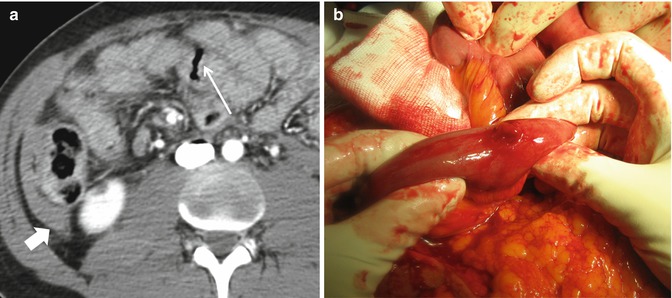
Fig. 17.3
Discontinuous bowel wall. (a) Axial CT contrast-enhanced image shows a wall discontinuity (arrow) on the anterior, antimesenteric wall of a small bowel loop, with extraluminal air and hemoperitoneum (thick arrow). (b) Intraoperative photograph of an antimesenteric small bowel wall perforation. Intraoperative image courtesy of Dr. Ennio Adami, MD
17.7.2 Extraluminal Air
The presence of extraluminal air has a reported specificity of 95% and a sensitivity of 30–60% for bowel perforation [23]. Pneumoperitoneum or so-called “free air” is not necessarily detectable on CT scans at admission and may be apparent only at later examinations, obtained after 6–12 h. In cases of small bowel perforation, only minimal amount of free air is present.
Pneumoretroperitoneum seems to be a more sensitive finding of perforation of one of the retroperitoneal intestinal tracts: second to fourth portion of duodenum, ascending and descending colon [31].
Although bowel perforation is a major cause of this sign, extraluminal air may also be observed in the absence of bowel perforation [32]. Other possible sources of free air in the abdomen are diffusion of a pneumothorax in patients with diaphragmatic injury, barotrauma, mechanical ventilation, and chest tube placement. Small amounts of air can penetrate through the female genital tract. Intraperitoneal rupture of bladder with Foley catheter in place can cause pneumoperitoneum as well. Mimicking true pneumoperitoneum, the presence of air confined between the inner layer of the abdominal wall and the peritoneum parietal layer, so-called “pseudopneumoperitoneum,” represents a potential diagnostic pitfall [4, 11].
However, the presence of free air in association with coexistent ancillary signs, such as bowel wall thickening, abnormalities of parietal enhancement, free fluid, and mesenteric infiltration, is highly predictive of bowel injury.
Using wide window settings (lung or bone windows) to review CT images aids in detecting small amounts of free abdominal air. Free air from bowel rupture commonly tends to extend behind the anterior abdominal wall, under the anterior parietal peritoneal layer, and along the anterior surfaces of liver and spleen (Fig. 17.4). However, foci of air may also be seen at the porta hepatis or in the mesenteric and portal venous system (Fig. 17.5). Extraluminal air can also be seen trapped in the mesentery (Fig. 17.6a), if the bowel wall discontinuity occurs on the mesenteric border, or located in the retroperitoneum, in case of duodenal, ascending and descending colon traumatic perforation (Fig. 17.6b).




Fig. 17.4
Axial CT contrast-enhanced scan shows free air from bowel rupture laying behind the anterior abdominal wall, along the anterior surfaces of liver and spleen (arrows in a). Viewing the CT image in a bone window (b) better demonstrates the presence of small amounts of extraluminal air collections

Fig. 17.5
Axial CT scans show air foci at the porta hepatis (arrows) (a). Axial CT scans show focal air bubble collecting in the portal venous system (arrow) (b)

Fig. 17.6
Axial CT contrast-enhanced scans show air foci trapped in the mesentery (arrow in a). Free air in the retroperitoneum (arrows in b)
17.7.3 Intramural Air
Major and minor bowel injuries have findings of bowel wall thickening and free fluid in common. Along with extraluminal air, the presence of air bubbles confined in the thickness of the bowel wall (Fig. 17.7) increases the probability of a full-thickness injury, a major injury that requires laparotomy, rather a partial thickness injury, which can be treated conservatively [31].


Fig. 17.7
Axial CT contrast-enhanced scan shows foci of intramural air (arrowhead) in a thick-walled small bowel loop. Interloop fluid is also seen (thin arrows)
17.7.4 Bowel Wall Thickening
Seen in 75% of transmural injuries, focal bowel wall thickening seems to be more sensitive for bowel injury than pneumoperitoneum [30–35]. This sign has a reported specificity of 90%, but is relatively insensitive, with reported values ranging 55–75% [36]. To minimize subjectivity in the evaluation of this sign, many authors suggest considering abnormal a disproportionate circumferential thickening of the bowel wall compared with normal appearing segments (Fig. 17.8) or a bowel wall thickness greater than 3 mm for the small bowel and 5 mm for the colon with adequate bowel distension. Focal bowel thickening can also be the expression of a partial thickness bowel injury. Intramural hematoma is a known evidence of blunt traumatic injury. Frequently localized to the duodenum (Fig. 17.9), uncommon in the large bowel, it is generally treated conservatively and tends to spontaneous resolution. Delayed complications such as stricture and obstruction are reported in some cases.