Fig. 27.1
The preferred local anesthetic injection procedure used at Walter Reed Army Medical Center (With permission from Buckenmaier and Bleckner [71])
Table 27.1
Recommended techniques and conditions to minimize the risk of local anesthetic intravascular injection
Standard monitoring with audible oxygen saturation tone |
Oxygen supplementation |
Slow, incremental injection (5 mL, every 10–15 s) |
Gentle aspiration for blood before injection and every 5 mL thereafter |
Initial injection of local anesthetic test dose containing at least 5–15 μg epinephrine with observation for heart rate change >10 beats/min, blood pressure changes >15 mmHg, or lead II – wave amplitude decrease by 25 % |
Pretreatment with benzodiazepines to increase the seizure threshold to local anesthetic toxicity |
Patient either aware or sedated but still able to maintain meaningful communication with the physician |
Resuscitation equipment and medications readily available at all times |
If seizures occur, patient care includes airway maintenance, supplemental oxygen, and termination of the seizure with propofol (25–50 mg) or thiopental (50 mg) |
Local anesthetic toxicity that leads to cardiovascular collapse should immediately be managed with prompt institution of advanced cardiac life support (ACLS) protocols |
Anatomy of the Brachial Plexus
The brachial plexus is commonly formed from the five roots (anterior rami) of vertebrae C5 through T1 (Fig. 27.2). Considerable morphological variations in brachial plexus formation have been described, even on contralateral sides of the same individual, though sex, race, or side of the body does not appear to influence this variation [6]. The brachial plexus can be described as “prefixed” when C4 brachial plexus contributions occur or “postfixed” when T2 contributions are noted. Uysal et al. [7] surveyed 200 fetuses noting the common C5 through T1 contribution that occurred 71.5 %, prefixed plexuses were observed 25.5 %, and the postfixed plexus was noted in 2.5 %.
The brachial plexus is typically further categorized into four major components or sections as it passes into the upper extremity (Fig. 27.2). Each of these components is bounded by distinct anatomical structures [8]:
Three trunks. The anterior rami of the plexus roots commonly coalesce into three major trunks with roots: C5 and C6 forming the superior trunk, C7 contributing to the middle trunk, and C8 and T1 making up the inferior trunk. The trunks are most easily identified as they pass between the anterior and middle scalene muscles. Anatomical variation exists in the relationship between the scalene muscles and the trunks with the most common variation being penetration of the anterior scalene muscle by the C5 and/or C6 roots [9]. These anatomical variants can have clinical significant when performing regional anesthetic blocks of the brachial plexus trunks.
Six divisions. Each trunk divides into an anterior division (anterior flexor nerves of the arm) and a posterior division (posterior extensor nerves of the arm) for a total of six divisions (three anterior, three posterior). The separation of the trunks into divisions occurs at the level of the first rib. The divisions then pass posterior to the midpoint of the clavicle through the cervicoaxillary canal.
Three cords. The six divisions emerge posterior to the clavicle to coalesce once again to form three cords. The cords are named based on their position in relation to the axillary artery as this neurovascular bundle passes into the axilla. The lateral cord (lateral to the axillary artery) is composed of the anterior divisions of the superior and middle trunk. The medial cord consists of only a continuation of the anterior division of the inferior trunk. The lateral and medial cords therefore give rise to nerves that ultimately service the flexor surface of the arm. The posterior cord is formed from the posterior divisions of all three cords. The posterior cord contains all of the nerves that will supply the extensor surface of the arm.
Five terminal branches. The five major nerves of the upper extremity are derived from the three cords. The musculocutaneous nerve (C5–C7) arises from the lateral cord and supplies the coracobrachialis, biceps brachii and brachialis muscles, and the skin to the lateral forearm. The lateral cord (C6–C7) and medial cord (C8–T1) both contribute to the formation of the median nerve which innervates anterior forearm muscles and the thenar half of the skin and muscles of the palm. The ulnar nerve is a branch of the medial cord (C7–T1) and supplies the forearm and hand medial to the midpoint of digit four. The shoulder joint and lateral skin over the deltoid muscle are innervated by the axillary nerve that branches from the posterior cord. Finally, the largest branch of the posterior cord gives rise to the radial nerve (C5–T1) which supplies all of the posterior compartment muscles and most of the posterior skin of the arm. Numerous other named nerves branch off of the brachial plexus though knowledge of the five major nerves is adequate for most clinical blocks of the brachial plexus.
A discussion of brachial plexus anatomy would be incomplete without addressing the considerable controversy that surrounds the existence of a “sheath” surrounding the brachial plexus and includes the artery, vein, and investing connective tissue. Multiple authors have described the anatomical structure referred to as a sheath, perhaps most famously by Winnie [1] who noted the muscles surrounding the brachial plexus contribute fascia that we “conceive of as the ‘sheath of the brachial plexus.’” Other authors have debated whether the sheath is a single tube or compartmented structure [10, 11]. Still others have rejected the existence of the sheath outright [12]. Recently, Franco et al. [13] performed systematic dissections on 11 embalmed cadavers and determined that a sheath-like structure surrounding the brachial plexus filled with loose connective tissue could be demonstrated in every specimen (Fig. 27.3a, b). The clinical significance and existence of a structure enveloping the brachial plexus has been suggested by both radiopaque local anesthetic injections [14] and observations during injections under direct ultrasound guidance [15]. Regardless of the term used to describe the investment of fascia that surrounds neurovascular structures, the preponderance of evidence suggests the brachial plexus sheath is a reality. The clinical significance of this structure continues to be debated and is worthy of additional study.
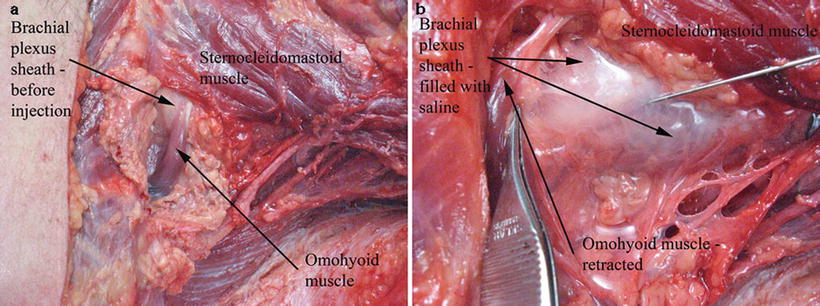
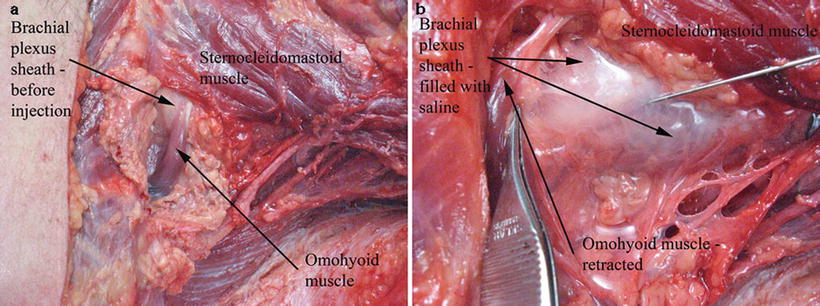
Fig. 27.3
(a) Brachial plexus sheath before and after injection with saline in a fresh cadaver specimen. Before: Prior to injection with saline. (b) Brachial plexus sheath before and after injection with saline in a fresh cadaver specimen. Before: prior to injection with saline (With permission from Buckenmaier and Bleckner [71])
Subsequent sections of this chapter will describe common regional anesthesia blocks for the brachial plexus to include interscalene, supraclavicular, infraclavicular, and axillary block. Each block will be presented with a discussion of pertinent anatomy, followed by approaches using both nerve stimulation and ultrasound guided. The approaches described in detail are preferred by the author and used in daily clinical practice. This should not deter the reader from exploring other methodologies that are referenced with no further explanation.
Interscalene Block of the Brachial Plexus
The interscalene block described by Winnie in 1970 [16] is performed at the level of the C6 vertebral body (Chassaignac’s tubercle). At this level, the roots of the brachial plexus pass the transverse processes of the vertebral bodies where they are invested between the fascia of the anterior and middle scalene muscles as the plexus passes between these muscles (Fig. 27.4). This provides a convenient compartment that local anesthetic can be deposited, to bathe the C5–C7 roots, resulting in consistent block of the shoulder muscles to include the deltoid, supraspinatus infraspinatus, and teres major muscles. Therefore, interscalene block of the brachial plexus is most commonly selected for operations on the shoulder, clavicle, or upper arm. This block is typically not selected for operations of the hand or forearm due to unpredictable spread of local anesthetic to the C8–T1 nerve roots (ulnar nerve). Inconsistent spread of local anesthetic to C3–C4 can result in posterior shoulder (cape area) sparing that should be considered for large operations on the shoulder (Fig. 27.5). Supplemental blocks such as an intercostobrachial nerve block (subcutaneous injection of local anesthetic from the axilla to the midpoint of the clavicle) are used to supplement the interscalene block for major shoulder surgery. Paravertebral blocks at T1–T2 can be added for procedures that include significant posterior shoulder dissections.
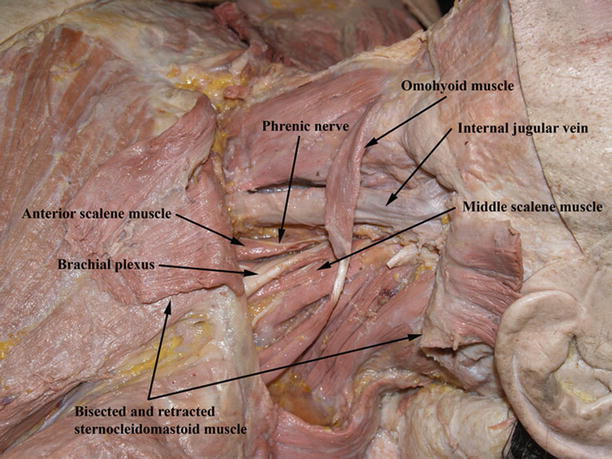
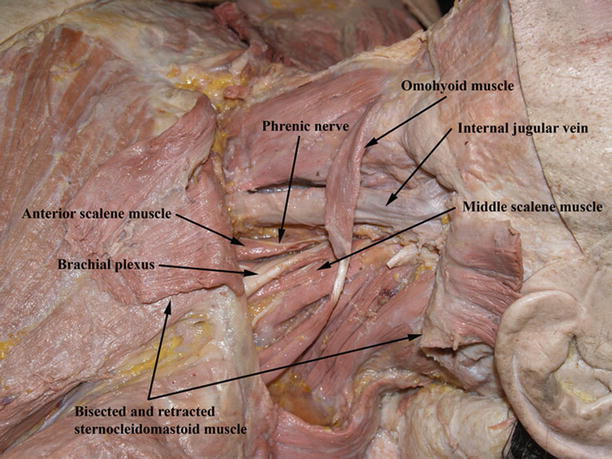
Fig. 27.4
Brachial plexus dissection above the clavicle (With permission from Buckenmaier and Bleckner [71])
Fig. 27.5
Dermatomes anesthetized with the interscalene block (dark blue)
The close proximity of the phrenic nerve lying anterior on the anterior scalene muscle usually results in paresis of the hemidiaphragm on the side blocked. Though most patients tolerate the loss of one hemidiaphragm with ease, the use of this block should be reconsidered in a patient that cannot tolerate a reduction in pulmonary function. Proximal spread of local anesthetic to the cervical plexus (C3, C4) and cervical sympathetic chain can result in a transient Horner’s syndrome and vocal hoarseness in some patients [17]. While this condition is self-limited, patients can become unnecessarily concerned if the possible occurrence of this side effect is not part of pre-block counseling. Perhaps the most devastating complication associated with this block is the unintended injection of local anesthetic into the vertebral artery located posterior and medial to the brachial plexus at this level. This error can lead to rapid cardiovascular collapse with few, if any, clinical signs warning of systemic local anesthetic toxicity [18]. Proper slow injection technique, with frequent gentle aspiration for blood every 3–5 mL of local anesthetic injected, is critical to guard against intravascular needle placement.
Procedure
The patient is placed supine with the head turned to the nonoperative side. Major external landmarks include the lateral border of the sternocleidomastoid muscle (SCM – best defined by having the patient lift their head off the bed 1 in.), the external jugular vein, the cricoid cartilage which corresponds to the C6 level, and the clavicle (Fig. 27.6). Regardless of the technology used to perform any block of the brachial plexus, it is worthwhile to examine and mark the patient’s pertinent anatomy prior to attempting needle placement. It is important not to confuse the more medial sternal head of the SCM with the clavicular head when palpating the lateral edge of this muscle, especially in obese patients. The jugular vein often crosses the lateral boarder of the SCM at the level of C6 (not the case in Fig. 27.6). At the level of C6, the lateral border of the SCM is gently palpated, and then fingers are moved just lateral to palpate the interscalene grove (between the anterior and middle scalene muscles). Initial needle placement is within the groove at the level of C6.
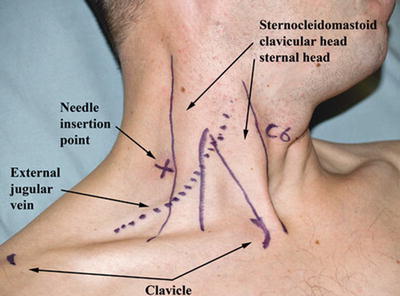
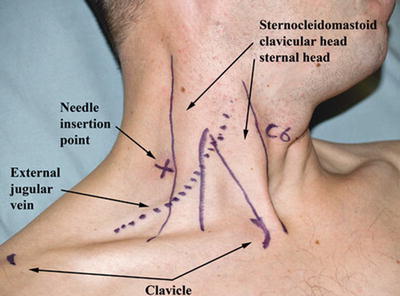
Fig. 27.6
External anatomy for interscalene block labeled (With permission from Buckenmaier and Bleckner [71])
Stimulation blocks are typically performed with 22-gauge, 5-cm, insulated needles with the stimulator initially set at 1.0–1.2 mA (Fig. 27.7). References are available for the technique and clinical applications of peripheral nerve stimulation [19]. A muscle twitch of the deltoid, biceps, or triceps at 0.5 mA or less indicates adequate proximity of the needle tip to the plexus for local anesthetic injection [20]. In most adults, the brachial plexus is rarely deeper than 1–2 cm below the skin. Trapezoid muscle stimulation suggests that the needle tip is posterior to the plexus while diaphragm stimulation indicates a needle tip that is too anterior. Local anesthetic volumes of 30–40 mL are sufficient to block the plexus in most adults. Modifications of the described interscalene method have been proposed to facilitate indwelling catheters [21], and posterior approaches have also been described [22]. Dagli et al. [23] compared the variations of the interscalene block and determined there was no reduction in complications and less satisfactory anesthesia compared to Winnie’s classic approach.


Fig. 27.7
Stimulating needle position for interscalene block (With permission from Buckenmaier and Bleckner [71])
Beginning with the last decade of the twentieth century, ultrasound technology has become a powerful tool to identify nerves and accurately place needles and local anesthetics. Preliminary data suggests that the addition of ultrasound to block procedures can improve success rates and decrease complications [15, 24, 25]. In some cases, ultrasound technology may be the only option available to place a regional anesthetic block when it is indicated [26]. A discussion on the physics and use of ultrasound is beyond the scope of this chapter though excellent references are available [27, 28]. The interscalene block is particularly well suited for ultrasound guidance due to the presence of good ultrasound landmarks and the superficial location of the brachial plexus at this level.
Preparation for an ultrasound-guided block is similar to a stimulation block. The use of external landmarks, when preparing for an ultrasound block, is no less important than when preparing for stimulation blocks. The external marks facilitate optimal ultrasound probe position and can reduce anatomy identification errors. The concurrent use of nerve stimulation with ultrasound can enhance block accuracy by providing objective evidence (motor nerve stimulation) that ultrasound-imaged targets are indeed nerves [29]. A high-frequency (5–12 MHz) linear probe is usually selected. Anatomical identification of the plexus at the C6 level is made easier if the probe is initially placed at the level of a supraclavicular block to identify the brachial plexus just lateral to the readily detectable subclavian artery. Once the plexus is located, it can be slowly traced cephalad to observe the three nerve trunks of the plexus as they pass between the middle and anterior scalene muscles (Fig. 27.8). The plexus is usually approached with the needle placed lateral within the plane of the ultrasound probe beam (Fig. 27.9). In-plane ultrasound-guided interscalene block allows real-time imaging of the needle in relation to target nerves and surrounding structures (Fig. 27.10). It also supports visualization of the local anesthetic injection allowing more accurate placement of medication around target nerves [30]. Many providers prefer out of plane needle placement when using ultrasound, though needle tip localization can be more difficult with this approach [31]. Practitioners often distribute local anesthetic to create the “donut sign” which is produced when hypoechoic local anesthetic surrounds the more echogenic nervous tissue. The most efficient block of the brachial plexus is produced when local anesthetic encircles the nerve structures. Authors have suggested that ultrasound guidance my also result in lower local anesthetic dosage requirements [32].
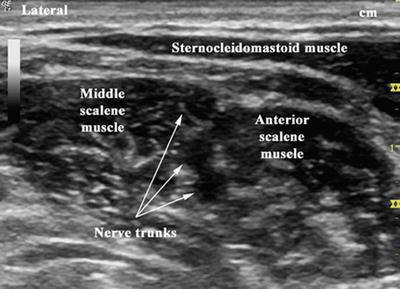
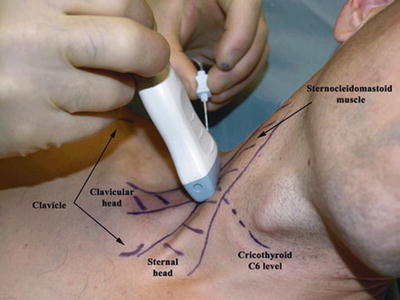
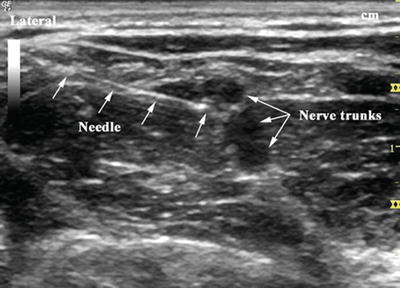
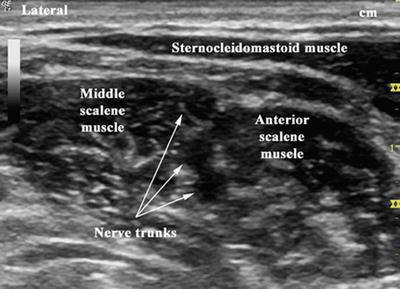
Fig. 27.8
Brachial plexus trunks at the level of C6 with ultrasound (With permission from Buckenmaier and Bleckner [71])
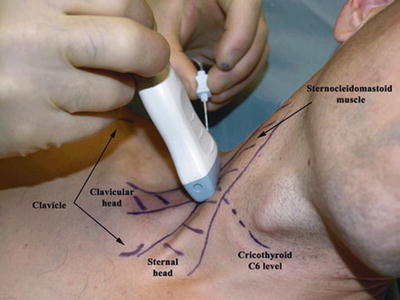
Fig. 27.9
Ultrasound-guided interscalene brachial plexus block (With permission from Buckenmaier and Bleckner [71])
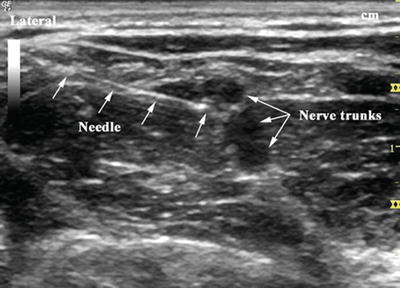
Fig. 27.10
In-plane needle placement during ultrasound-guided interscalene block (With permission from Buckenmaier and Bleckner [71])
Supraclavicular Block of the Brachial Plexus
The supraclavicular approach, or subclavian perivascular technique [33], for blocking the brachial plexus is ideal for anesthesia and analgesia of the upper arm from the midhumeral level down to the hand (Fig. 27.11). If a tourniquet of the brachium is planned for surgery, an intercostobrachial nerve block should be considered as a supplemental block. Anatomically, blockade of the brachial plexus just cephalad to the clavicle is facilitated by the compactness of the plexus trunks and divisions as these nerves pass under the midpoint of the clavicle. Packed together at this point, the brachial plexus is more easily surrounded by local anesthetic resulting in rapid block onset and high success rates. Franco et al. [34] determined that the unique supraclavicular anatomy of the brachial plexus allowed injection of local anesthetic during stimulation-assisted block at currents as high as 0.9 mA rather than the typical 0.5 mA recommended for most stimulating blocks with no reduction in block success.
Fig. 27.11
Dermatomes anesthetized with the supraclavicular block (dark blue)
Unlike the interscalene approach which results in a 100 % incidence of hemidiaphragmatic paresis that can result in subjective symptoms of respiratory difficulty, the supraclavicular approach results in hemidiaphragmatic paresis only about 50 % of the time and is rarely associated with respiratory complaints [35]. At the level of the clavicle, the apex of the lung is just medial and posterior to the brachial plexus (deep to the first rib), so the complication most often associated with the supraclavicular block approach is pneumothorax. Using paresthesia techniques, authors in the 1960s described incidences of pneumothorax greater than 6 % [36]. For this reason, the technique fell out of favor until modern block technology and refinements in the approach reduced the incidence of this complication to less than 1 % [37–39]. Signs and symptoms of a large pneumothorax include sudden cough and shortness of breath. Should these symptoms manifest during the block procedure, the patient should undergo a chest X-ray prior to going to the operating room.
Procedure
The head of the supine patient is turned to the nonoperative side. External landmarks for the supraclavicular approach are similar to those used for the interscalene block (Fig. 27.12). The interscalene groove is palpated at the level of C6, and the fingers are then moved caudad within the groove to a point approximately 1 cm cephalad from the clavicle. This is the needle insertion point for stimulating blocks. The groove below C6 can sometimes be difficult to palpate due to the overlying omohyoid muscle. The subclavian arterial pulse is often palpable just medial to the needle insertion point by rolling the index finger over the top of the clavicle. This can be used as an additional confirmatory landmark.


Fig. 27.12
External anatomy for the supraclavicular block labeled (With permission from Buckenmaier and Bleckner [71])
Supraclavicular stimulation blocks are typically performed with 22-gauge, 5-cm, insulated needles with the stimulator initially set at 1.0–1.2 mA. The provider stands at the patients head and directs the needle toward the axilla (Fig. 27.13). Proper needle placement in proximity to the brachial plexus is indicated by flexion or extension of the digits at 0.9–0.5 mA or less [34, 37]. Aspiration of blood or blood observed in the clear tubing suggests the needle tip is too medial and may have penetrated the subclavian artery. Persistent musculocutaneous nerve stimulation (biceps contractions) with needle advancement suggests too lateral a needle placement. Pectoralis muscle stimulation indicates anterior needle placement, and scapular stimulation suggests the needle is posterior to the brachial plexus. Local anesthetic volumes of 30–40 mL are usually injected to block the brachial plexus using this approach. Other stimulating supraclavicular block techniques have been described that purportedly reduce the risk of pneumothorax [40, 41].
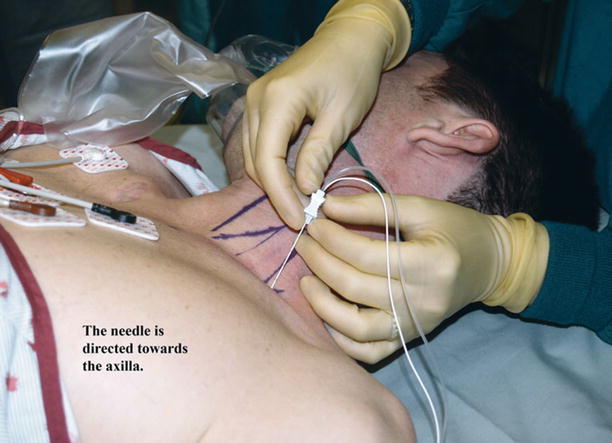
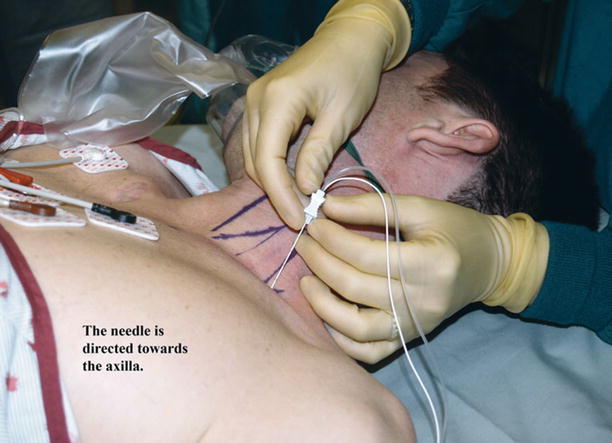
Fig. 27.13
Stimulating needle position for supraclavicular block (With permission from Buckenmaier and Bleckner [71])
Authors have suggested that the addition of ultrasound technology to the supraclavicular block has enhanced speed of block placement, improved block success, and provided superior anatomy identification compared to use of stimulation for the block [42, 43]. A high-frequency (5–12 MHz) linear probe is used for this block. The ultrasound probe is positioned directly above the clavicle in the supraclavicular fossa (Fig. 27.14). This plane gives the best transverse view of the brachial plexus, typically located lateral and slightly superior to the subclavian artery at a depth of 2–4 cm. The nerves appear as hypoechoic circles with hyperechoic rings that are sometimes described as a “bundle of grapes” (Fig. 27.15). The needle is inserted at the lateral end of the ultrasound probe and advanced under direct visualization of the entire needle shaft down to the brachial plexus. It is very important to always keep the tip and shaft of the needle in clear view to ensure the needle is not being placed in areas that can result in pneumothorax or vascular puncture. The local anesthetic can be spread precisely by injecting small aliquots, observing spread, and adjusting the needle as necessary for complete envelopment of the brachial plexus (Fig. 27.16). Supraclavicular blocks can also be performed using out-of-plane approaches though there is no clinical data to support any particular out-of-plane technique [31].






Fig. 27.14
Ultrasound-guided supraclavicular brachial plexus block (With permission from Buckenmaier and Bleckner [71])
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree