Fig. 50.1
(a, b) Epidural abscess seen on the above T2 and T1 axial images of the lumbar spine resulting in compression of the exiting right L5 spinal nerve. It occurred following a right L5/S1 intra-articular zygapophysial joint injection
Other documented complications of interlaminar epidural injections include arachnoiditis, intrinsic spinal cord injury, spinal anesthesia, transient paralysis, arterial gas embolism, and transient blindness [28, 29]. Controversy exists over whether arachnoiditis can complicate epidural steroid injection [19, 20].
Anatomy
Understanding the anatomy of the epidural space is important. It is triangular in shape, and 1–2 mm in depth in the upper cervical spine, with 3 mm in depth in the lower cervical spine, this increases to up to 5 mm in the upper thoracic spine and is 5–6 mm in depth in the midlumbar spine. Thirty-four percent of the time, the ligamentum flavum is adherent to the dura above C5 [30].
Recommendation
The needle entry point for cervical interlaminar epidural steroid injections should be at the C7/T1 level or below, and the epidural space should be entered in the midline where depth is greatest. The needle should be anchored at the skin with the nondominant hand and advanced with the dominant hand.
When the epidural space is identified with the loss of resistance technique, a catheter should be thread to the appropriate level and contrast injected to confirm the correct level, no vascular uptake and an epidurogram (Figs. 50.2 and 50.3) [31–34]. One should minimize the volume injected to 2–3 cc, and the solution should be injected slowly. AP, oblique, and lateral fluoroscopic views should be taken to document unequivocal epidural spread of contrast prior to injection of medication. Contrast should be injected under live fluoroscopy to confirm no concomitant vascular uptake (Fig. 50.4). Sedation should also be minimized because oversedation may cause loss of communication and the ability to monitor the patient. Oversedation also increases the potential for unintentional patient movement or startle and increases the potential for cardiopulmonary complications. It is generally accepted in the pain medicine community that oversedation or deep monitored anesthesia care (MAC) should not be utilized because it increases the potential for catastrophic complications as spinal cord trauma.
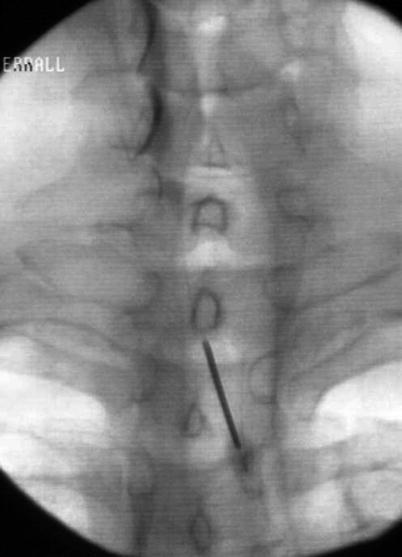
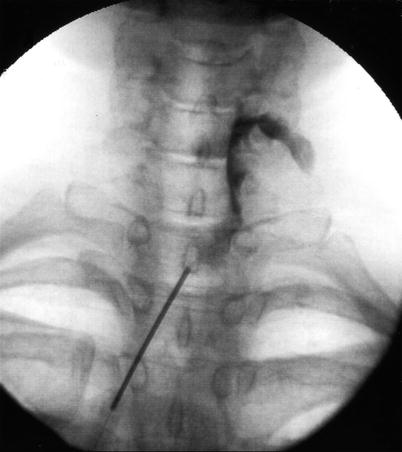
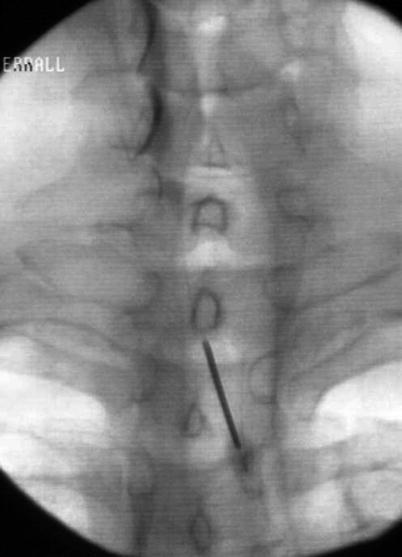
Fig. 50.2
AP fluoroscopic image of a cervical interlaminar epidural steroid injection with a catheter thread to C6/7 in a patient with a left C7 radiculopathy. Note needle entry at T2/3
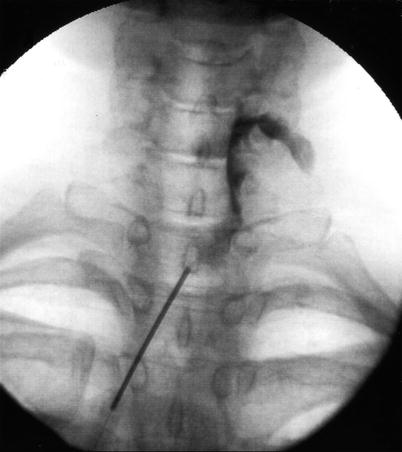
Fig. 50.3
AP fluoroscopic image of a cervical interlaminar epidural steroid injection with a catheter thread to C5/6 in a patient with a right C6 radiculopathy. Note needle entry at T1/2
Fig. 50.4
(a) AP fluoroscopic image of a right C5/6 transforaminal epidural steroid injection. (b) AP fluoroscopic image of a right C5/6 transforaminal epidural steroid injection. Please note the vascular uptake not seen on the previous image is apparent with contrast injection under live fluoroscopy
The advantage of this technique is to reduce the chance of dural puncture, spinal anesthesia, and spinal cord injury. Entering the epidural space at the midline position, where there are fewer epidural veins, will also reduce the potential risk of epidural hematoma.
Transforaminal epidural steroid injections are felt in general to be safe, although the prevalence of complications remains underreported [35]. Complications from the transforaminal approach are similar to interlaminar epidural steroid injections but also include the catastrophic complication of anterior spinal cord syndrome. This can follow inadvertent injection into the radiculomedullary artery (Adamkiewicz) in the lumbar or thoracic spine or cervical radicular artery in the cervical spine. Locked-in syndrome or brain stem infarct may follow unrecognized vertebral artery injection during cervical transforaminal injection (Fig. 50.4).
In the thoracic and lumbar spines, two unfortunate circumstances need to be present. Firstly, the artery of Adamkiewicz (radicular medullary artery) needs to be present at the symptomatic level and, secondly, undetected arterial penetration with subsequent injection. The artery of Adamkiewicz usually arises on the left between T7 and L4 but may be as low lying as S1 on the left or right. It runs with the spinal nerve in the anterosuperior aspect of the foramen and therefore may be penetrated inadvertently at this site [36, 37].
Proposed theories for this include intravascular injection of particulate steroid, resulting in spasm or thrombosis, which results in anterior spinal cord infarction because of the absence of collateral circulation. In the cervical spine, the sole vascular supply to the anterior spinal cord again comes from the anterior spinal artery, and the feeding radicular arteries are highly variable in number, location, and side. Similarly, the presence of a radicular artery at the symptomatic level, and undetected interarterial injection, can result in anterior spinal cord infarction and quadriplegia [38–47].
Strategies to reduce the chance of this catastrophic complication include the following: (1) understanding the fluoroscopic anatomy; (2) understanding contrast flow patterns; (3) optimizing interventional skills; (4) use of extension tubing and injection of contrast under live fluoroscopy to avoid the need to recannulate the needle after contrast is injected; (5) use of digital subtraction imaging; (6) use of nonparticulation solution such as dexamethasone and betamethasone; (7) in addition, some experts have recommended using blunt tip needles, as these are less likely to penetrate an artery [48, 49]; and (8) needle placement in the posteroinferior aspect of the foramen (lumbar, thoracic) to avoid the artery of Adamkiewicz which runs with the spinal nerve in the anterosuperior aspect of the foramen.
Trigger Point Injection
Trigger point injections are generally considered to be fairly straightforward; however, some catastrophic complications have been described in cases without fluoroscopy. In a closed claims study, the second most common cause of pneumothorax behind intercostal nerve block was trigger point injection, being responsible for 21 % of cases [5].
Other documented complications include local infection, cellulitis, hematoma, epidural abscess, pneumothorax, spinal anesthesia, spinal cord injury, anaphylaxis, and death.
Use of fluoroscopy for trigger point injections in the cervical or thoracic area will help reduce needle misplacement, either into the epidural, subdural, subarachnoid space, or into the spinal cord, which has occurred with trigger point injections of paraspinal muscles. The use of lateral fluoroscopic guidance for trigger point injections of any posterior thoracic wall musculature will document needle depth and prevent pneumothorax by remaining superficial to the ribs [50–52].
Zygapophysial Joint Injection/Medial Branch Block
In general, lumbar zygapophysial (facet) joint injection is a safe procedure, although complications similar to epidural steroid injections have been described. These include infection with resulting cellulitis or epidural abscess, epidural hematoma, intravascular injection, dural puncture, spinal anesthesia, spinal cord trauma, neural trauma, chemical meningitis, and pneumothorax. Vertebral artery damage or injection is a potential risk with cervical facet joint injections [53–59]. With the use of fluoroscopy and contrast injection in experienced hands, serious complications should not occur. In the cervical spine, a posterior parasagittal approach to the medial branch nerves or posterior approach to the interarticular z-joint injection is safer than a lateral approach (Fig. 50.5). A lateral approach brings the contents of the spinal canal potentially into the path of the needle, especially if the clinician is unable to eliminate parallax and get a true lateral fluoroscopic image. Potential for going through and through a facet joint is real if needle depth is not checked frequently as the needle is advanced. Ideally, under tunnel vision, the periosteum of the adjacent articular process should be intentionally contacted prior to entering the joint to confirm depth and then the needle rotated into the joint. This will help prevent the needle going through the joint to the adjacent tissue [60].


Fig. 50.5
Lateral cervical spine fluoroscopic image of C4 medial branch block showing vascular uptake
Stellate Ganglion Block
Many techniques have been described for stellate ganglion block, some of which are without fluoroscopic guidance [61–63]. Multiple complications have been described, most of which have occurred from nonfluoroscopically guided injections that have resulted in inadvertent needle placement into the vertebral artery, adjacent disc, neurotissue, esophagus, intrathecal space, or pleura. These complications have included seizures from intravascular injection, spinal anesthesia, cervical epidural abscess, brachial plexus block, intercostal neuralgia, locked-in syndrome, pneumochylothorax, pneumothorax, reversible blindness, hoarseness, dysphagia, and death [64–74]. These complications can be reduced or hopefully eliminated with a technique described by Abdi et al. [75].
Under ipsilateral oblique fluoroscopic guidance, the respective endplates are squared off, and the C-arm is obliqued until a crisp C7 uncinate process is visualized. Then a 25-gauge spinal needle is advanced down, under tunnel vision, to the base of the uncinate process at the junction of the vertebral body. Under live fluoroscopic guidance with extension tubing, injection of contrast is performed to confirm appropriate nonvascular contrast flow. The needle will lie anterior to the vertebral artery, posterior to the common carotid artery, and lateral to the esophagus. A total of 5 cc should be adequate to obtain stellate ganglion blockade.
Discography
In experienced hands, discography is safe, whether that be in the cervical, lumbar, or thoracic spine. Understanding indications and contraindications to discography is important. Coagulopathy and active infection are general contraindications, but central spinal stenosis, myelopathy, and large disc protrusion are contraindications to cervical or thoracic discography [76].
Potential and described complications pertinent to all three areas include superficial infection, epidural abscess, discitis, or nerve root injury. In the cervical or thoracic spine, the potential for spinal cord injury exists. Quadriplegia has been described following epidural hematoma, epidural abscess, and from subdural empyema [77–84]. It has also occurred secondary to cervical disc herniation from disc pressurization at discography. Keeping the contrast volume in cervical or thoracic discography to a minimum is also important, with less than 0.5 cc/disc usually sufficient for cervical discography.
While infection is a real concern, the administration of preoperative intravenous antibiotics, intradiscal antibiotics, and/or a coaxial needle technique has been described in the literature to be able to reduce the incidence of infection (Fig. 50.6).


Fig. 50.6
T2-weighted MRI scan of lumbar spine demonstrating L4/5 discitis
A coaxial needle technique has been shown to reduce the chance of discitis from 2.7 to 0.7 % in 220 patients [85]. Preoperative intravenous cefazolin has been shown to reduce the chance of disc infection from 1 to 4 % down to 0 %. Utilizing cefazolin in a concentration of 1 mg/cc intradiscally resulted in no intradiscal infections of 127 patients [86, 87].
The prophylactic antibiotics commonly utilized do not prevent anaerobic discitis, which may occur with the anterior approach to cervical discography, where esophageal penetration is possible. Utilizing a right anterolateral (oblique) approach reduces the chance for esophageal perforation and consequent potential anaerobic discitis. Auscultation of the carotid artery should be performed and ultrasound ordered if carotid bruits are heard prior to discography if an oblique approach is utilized, because of the potential of the needle traversing the carotid and dislodging an unstable plaque.
Patients with discitis usually present with pain and fever, 3 days to 2 weeks post-discography. Erythrocyte sedimentation rate, white cell count, and C-reactive protein are usually positive within the first week. It may take anywhere from 2 to 5 weeks for a bone scan to become positive. MRI with or without gadolinium is now considered the gold standard imaging study. If discitis is suspected, infectious disease consultation, disc biopsy, and culture should be taken. IV antibiotics should be started, and consideration should be given for surgical exploration and/or bracing.
Many of the complications reported with lumbar discography were reported prior to 1970, with many of them in the 1950s. Today with preoperative intravenous antibiotics, intradiscal antibiotics, and a coaxial needle technique, with extrapedicular, extradural fluoroscopically guided approach, these complications should be minimal [88, 89].
If a posterior transdural approach to a disc is planned, then it is important not to utilize intradiscal cefazolin because of the potential for intractable seizures with inadvertent intrathecal cefazolin injection. Therefore, in a patient with previous posterolateral intratransverse bony fusion mass, when posterior transdural approach is considered, or if inadvertent dural puncture occurs with extrapedicular, extradural approach to the disc, then contrast should be mixed with another antibiotic besides cefazolin, such as ceftriaxone, gentamicin, or clindamycin [90].
Pneumothorax has been described as a complication of thoracic discography but could also occur with cervical discography at the C7/T1 level.
In general, cervical or thoracic discography, because of the more challenging technical aspects, and potential for more catastrophic complications, should only be performed by highly skilled and experienced interventionalists.
Summary
It is important to know the literature on current technical standards, modify practice accordingly, and understand that many complications are never published. History and physical examination should be performed on all patients prior to spinal injections. Physicians should review pertinent imaging studies, understand indications and contraindications of procedures, and obtain informed consent. Knowledge of regional and fluoroscopic anatomy is important before attaining technical expertise in a supervised training environment. Familiarization with all contrast flow patterns under live fluoroscopy is imperative. Above all, understand that complications are inevitable, and it is imperative to identify and treat these problems promptly to minimize their impact when they occur and communicate these issues with the patient.
Patient Pertinent Issues
A thorough history and physical examination is vital on all patients prior to neuraxial blockade, regardless of practice set-up or referral pattern. Important points of the history of a patient undergoing an interventional procedure will be addressed.
Past Medical History
This should include any bleeding diathesis, any immune suppressive disorder, history of allergy, anaphylaxis or asthma, and whether they have valvular heart disease.
Medications
It is important to note whether the patient is taking any oral steroid, antibiotics, anticoagulants, or Glucophage, as these will impact patient outcome. Glucophage is generally considered safe in patients with normal renal function when a small amount of nonionic contrast is utilized. It should be temporarily discontinued in patients with impaired renal function undergoing procedures requiring larger amounts of contrast, as it may result in the patient developing lactic acidosis.
Patients taking oral steroids will not only be immunosuppressed but also at increased risk of potential side effects from steroids [91].
Anticoagulants will clearly put patients at risk for hemorrhagic complications. Knowledge of prescription and over-the-counter medications and herbal remedies is important in risk-stratifying patients.
Neuraxial blocks on patients with an active infection requiring antibiotics should be postponed because of the potential for bacteremia and introduction of bacteria to the epidural space.
Allergies
Knowledge of patient allergic to medications that may be utilized in a procedure such as steroid, local anesthetic, or antibiotics is important in reducing the chance of anaphylactic reaction. It is also important to document any known allergy to shellfish or iodine if contrast is to be utilized and any latex allergy, as these procedures need to be done, first case of the day, in a latex-free environment. (Gadolinium may be used in iodine-allergic patients, although there is a documented cross allergy to gadolinium.)
Review of Systems
Thorough review of systems should help rule out any occult coagulopathy, infection, cord compression, malignancy, or pregnant state.
Social History
This should include any prior litigation as even more thorough documentation and informed consent may be required.
Physical Examination
A general but also procedure-specific physical examination should be performed. Attention should be paid to whether the patient is hemodynamically unstable or febrile, as elective procedures should be rescheduled in that event.
A thorough neurological examination is important to establish as a baseline, especially in the event of an adverse neurological outcome. Knowledge of a carotid bruit and subsequent Doppler study result is vital in patients undergoing procedures, in which the carotid artery may be penetrated, such as cervical discography, as the potential for dislodging a mobile thrombus is real. A thorough cardiopulmonary assessment is important in patients undergoing conscious sedation.
Imaging Study
Interventional pain physicians should be to the spine, what the cardiologist is to the heart. They should be comfortable with not only the medical and interventional management of these patients but as good, if not better, than the radiologist in interpreting pertinent spinal imaging studies. Reviewing the imaging prior to procedure in all patients is important [30, 76].
The Nurse
Time should be taken to train nursing staff and allied health professionals in interventional pain medicine, as they play a vital role in reducing significant complications.
Probably the most important checklist that medical assistants, nurses, and surgical technicians should review with all patients includes:
1.
Allergies – Knowledge of nonmedication (shellfish, latex, iodine) and medication allergies is imperative as outlined above.
2.
Pregnancy – Documentation of the last menstrual period and a pregnancy test if there is any concern should be required if fluoroscopy is utilized.
3.
Anticoagulants – Prescription anticoagulation or over-the-counter medication or herbal remedies taken by the patient, which have potential for impairing normal coagulation, need to be known. This will be discussed in more detail later.
4.
Diabetes – If the patient is a diabetic, knowledge of their finger-stick blood glucose is important, as they may be hypoglycemic if fasting or at risk of hyperglycemic complication if steroid injection is planned.
5.
Fever – Elective spinal injections should be postponed in a febrile patient, as the risk of infectious complication increases.
6.
Fasting – Knowledge of the last time a patient ate or drank is important if conscious sedation is anticipated.
7.
Side – The side of the patient’s symptoms should be marked with an X to help reduce one of the more common preventable surgical errors.
This checklist should be issued to all staff members who interact with the patient and should be communicated to the physician in the operating room prior to each procedure.
Nurse/Surgical Technician Preparation
If the physician is not drawing up the medications for injection, then appropriate education and training of the surgical staff is vital in reducing medication errors. Medication should be drawn up by a surgical technician with nursing supervision. All syringes should be labeled, and clearly, sterile precautions must be followed.
If you practice in a setting that is used by different specialists, such as a radiology suite at a hospital, it is important that the physician reviews all the medications prior to each procedure, to ensure no medication error. Specifically, that preservative-free local anesthetics are utilized (for epidural injections), and nonionic contrast that is safe for intrathecal use, such as Omnipaque or Isovue, and not an ionic contrast medium that may be used for urologic or gastrointestinal imaging.
Appropriate sterile preparation is mandatory and should include povidone-iodine preparation, allowing it to dry. In patients with iodine allergy, chlorhexidine gluconate and/or isopropyl alcohol may be used. For more invasive procedures such as implant or discography, some practices utilize a triple scrub, including isopropyl alcohol, chlorhexidine gluconate, and povidone-iodine. While sterile towels are adequate for draping an area for most procedures, in the case of more invasive spinal procedures, full-body draping with iodine-impregnated fenestrated adhesive biodrapes, sterile towels, and half sheets should be used [92, 93].
Patient Monitoring
Appropriate perioperative monitoring is important for all procedures and should include IV access, pulse oximetry, cardiac monitoring with ECG tracing, and blood pressure and heart rate monitoring. A fully stocked, regularly updated crash cart should be easily accessible. ACLS-trained personnel should be available. Mock codes should be run at least quarterly. This will help minimize the impact of an adverse reaction or complication.
In the postoperative patient recovery room, trained staff knowledgeable in recognizing post-procedural complications should be available. Such complications include hypotension, vasovagal reactions, sensory motor blockade, excessive somnolence, respiratory suppression, and cardiovascular complications.
Depending upon the procedure and the amount of sedation utilized, patients will be in a monitored postoperative setting, anywhere from 20 min to 8 h, until discharge criteria are met. These include an alert, oriented patient who is hemodynamically stable, with stable cardiovascular and neurologic examination and ambulating as well as expected, with someone else to drive them home if they have had sedation.
Physician
Physicians from numerous subspecialties have converged on the field of interventional pain medicine, all with varying levels of training and competence. Until recently, the standard interventional pain training occurred in the fellowship setting. Interventional pain medicine, now a recognized subspecialty of medicine, will soon have formal residency training programs.
There are still physicians performing interventional pain techniques that were learned at weekend courses. While these courses are helpful, they are by no means sufficient. A thorough understanding of spinal anatomy and how that relates to fluoroscopic anatomy is vital. Unfortunately, at these conferences, the optimum fluoroscopic image is already set, and physicians may struggle with reproducing this in their clinical practice. Contrast flow patterns are not generally taught, and therefore, the ability to recognize vascular uptake or to differentiate between a myelogram, epidurogram, or subdural contrast flow is not learned.
Physicians should be cognizant of all potential complications pertinent to a given procedure being performed. The mindset of anticipating complications will hopefully lead to earlier recognition, a more prompt and appropriate response, and minimize the effect of that complication. It is inevitable that a complication will occur to every interventionalist. How it is dealt with will frequently determine the outcome.
The physician should not be afraid to reschedule the procedure if difficulties are encountered with a particular procedure on a given day. If, for example, while performing a cervical transforaminal epidural steroid injection, vascular uptake is noted despite repositioning the needle multiple times in the foramen, the appropriate course of action may be to reschedule the patient or consider an interlaminar approach.
The minimum experience level required for certain procedures is somewhat controversial. Clearly the level of expertise required to perform an uncomplicated interlaminar lumbar epidural steroid injection on a healthy patient is far less than that required for a cervical transforaminal epidural steroid injection. Cadaver courses may help develop some of those skills, but supervised training in the clinical setting is strongly advised.
Equipment
The physician should be familiar with all equipment that may be required for a given procedure. They should be able to operate all the equipment independently and problem solve in the event of equipment malfunction. Reliance on company representatives or surgical technicians may result in operator error and avoidable complication. The physician should know how to run the fluoroscope and obtain optimal fluoroscopic images and minimize radiation exposure to all personnel.









