Brain Herniation
Joshua Smith
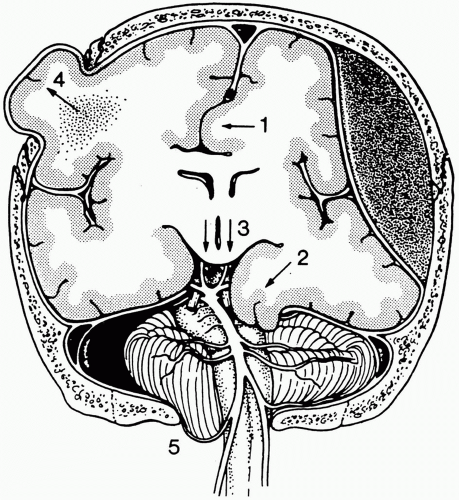
Brain herniation may occur across the falx cerebri, tentorium cerebelli, or through openings such as foramen magnum and craniectomy defects. Any process that causes an elevation in the intracranial pressure can result in brain herniation. Space-occupying lesions (e.g., tumor, abscess, hematoma, and stroke), diffuse processes (e.g., edema, encephalitis, and subarachnoid hemorrhage), or increased cerebrospinal fluid (CSF) (e.g., hydrocephalus) are examples. Herniations of the brain are classified into five categories: (1) transtentorial, (2) subfalcine, (3) tonsillar, (4) alar, and (5) extracranial (Fig. 15-1).
Imaging findings related to herniation have a similar appearance on both computed tomography (CT) and magnetic resonance imaging (MRI) although they are better depicted on MRI due to multiplanar capability and superior soft tissue contrast. Each category of herniation may occur in isolation or conjunction with other categories.
Each category of herniation may be associated with a specific neurologic syndrome, described subsequently. Early, nonspecific signs of herniation reflect elevated intracranial pressure and include headache, nausea, vomiting, vision disturbance, papilledema, altered level of consciousness, and Cushing’s triad (alteration in respiration, bradycardia, and systemic hypertension). Late signs of herniation include decorticate and decerebrate posturing. Each category of herniation may rapidly progress to death, and because of this, it is imperative that the clinician be promptly notified of any imaging findings suggestive of herniation.
Subfalcine herniation is the most common form of herniation and occurs when mass effect displaces brain medially and forces the cingulate gyrus underneath the falx cerebri. The falx cerebri is a sickle-shaped fold of dura mater which lies within the longitudinal fissure, separating the cerebral hemispheres. The paired pericallosal arteries, branches of the anterior cerebral artery (ACA), travel along the free edge of the falx.
Clinical Findings
The clinical syndrome associated with subfalcine herniation relates to compression of the ipsilateral ACA which may get pinned against the relatively fixed falx, leading to infarction in its vascular distribution and the clinical syndrome of contralateral leg weakness.
Possible Findings (Fig. 15-2)
Best depicted on the coronal scan.
Midline shift of septum pellucidum. Measurement of septum pellucidum midline shift is performed in two easy steps. First, draw a straight line from the anterior-most to the posterior- most aspects of the falx. This represents the expected normal location of the septum pellucidum. Next, draw a perpendicular line from the displaced septum pellucidum to this first line. Serial measurements should be performed at the same approximate level to accurately document change in midline shift over time.
Compression of the ipsilateral lateral ventricle.
Dilatation of contralateral ventricle due to foramen of Monro obstruction.
Widened subarachnoid space on side of falx away from mass lesion.
Displacement of lateral ventricle and corpus callosum away from mass lesion.
Displacement of the ACA.
Infarct in ACA distribution.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree