12
Brain Neoplasms
Eugene C. Lin and Abass Alavi
Although positron emission tomography (PET) imaging may not be indicated in the majority of newly diagnosed brain tumors, it is useful in specific situations:
- Determining the best biopsy site for optimal grading of the tumor
- Metabolic grading of the tumor: the degree of glucose metabolism correlates with prognosis and outcome in these patients (Fig. 12.1).
- Evaluating possible transformation of a low-grade glioma to a high-grade tumor
- Factors affecting fluorodeoxyglucose (FDG) uptake
- Corticosteroids. Corticosteroids decrease glucose metabolism in normal brain tissue but do not affect metabolism within brain tumors. However, corticosteroid administration will limit evaluation of brain tumors, as overall image quality and anatomical detail are adversely affected.2,3 Many of the effects of corticosteroids may be due to increased blood glucose levels.
- Cushing disease. Patients with Cushing disease have decreased brain glucose metabolism.
- Sedatives and anticonvulsants. Sedatives and anticonvulsants can also reduce glucose metabolism.
- Brain edema. Uptake of FDG is substantially reduced in any area of the brain that is adjacent to white matter edema seen on magnetic resonance imaging (MRI) or computed tomography (CT) images. This is probably a reversible process and should disappear with reduction in the degree of edema.3 The decreased gray matter uptake secondary to edema may improve the contrast between the tumor and adjacent structures.
- Glucose level. High blood glucose decreases FDG uptake in both the tumor and the cortex, but there is a greater decrease in cortical activity; thus, a higher tumor-to-background ratio is often noted in hyperglycemic states.
- Hyperglycemia. Although most patients should not be scanned in a hyperglycemic state, high blood glucose may potentially be advantageous in the detection of tumors near or in the cortex.4
- Delayed imaging. Delayed imaging (3 to 8 hours after injection) increases uptake in the tumor relative to normal brain. This is most helpful in tumors near the gray matter.5
- Standardized uptake value (SUV). SUV may not be as useful in the brain, as it may not correlate well with regional glucose metabolism. Tumor-to-white matter or tumor-to-cortex ratios may be preferable.6
- False-negatives. Small low-grade neoplasms are often undetectable on PET. A minority of high-grade tumors are also undetectable on PET.
- False-positives
- Low-grade neoplasms such as pilocytic astrocytoma, pleomorphic xanthoastrocytoma, ganglioglioma, and oligodendroglioma can be hypermetabolic.6,7
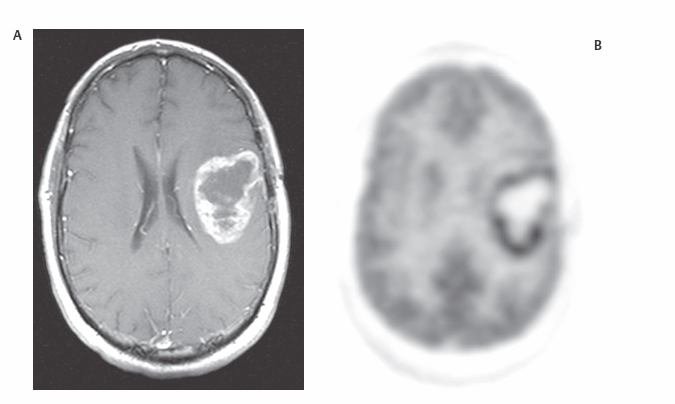
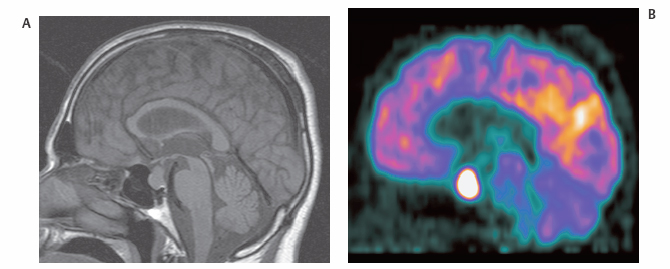
- Benign lesions such as meningioma (Fig. 12.2), pituitary adenoma (Fig. 12.3), and histiocytosis X can be hypermetabolic.
- Seizures at the time of FDG administration can cause false-positive results due to activated cortex adjacent to the tumor site.
- A hypermetabolic flare phenomenon may be seen in glioblastoma treated with chemotherapy if PET is performed 24 hours after the first dose.8 This may predict longer survival.
 Primary Brain Tumors1
Primary Brain Tumors1