Cranial Nerve I Axial 1
Normal Anatomy
The olfactory nerve, or cranial nerve (CN) I, is the first of 12 cranial nerves and provides innervation for the sense of smell. CN I can often be seen on axial magnetic resonance imaging of the brain at the level of the temporal lobes. Nerve fibers from the olfactory mucosa in the anterosuperior nasal cavity join with the olfactory bulb, from which signals pass through nerves running within olfactory foramina in the cribriform plate in the superior nasal cavity.
Cranial Nerve I Coronal 1

Imaging Technique Consideration
Clinicians should always approach loss of smell as a serious symptom and explore anatomic causes. The best imaging plane to assess the olfactory nerves is coronal, perpendicular to the long axis of the nerves. T2-weighted MR coronal images help to delineate the olfactory nerves, with surrounding cerebrospinal fluid (CSF) between the nerves and the bony walls of the olfactory grooves. In some patients, one olfactory groove may be asymmetrically lower than the other, an important consideration if the patient may be undergoing functional endoscopic sinus surgery (FES). One notable tumor centered on the olfactory nerves is esthesioneuroblastoma (olfactory neuroblastoma).
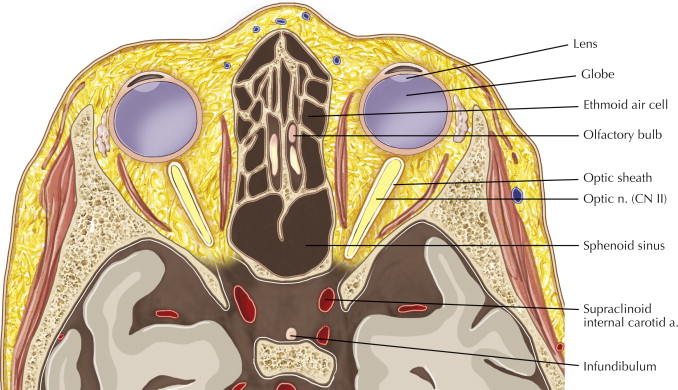
Cranial Nerve II Axial 1
Diagnostic Consideration
The optic nerve (second cranial, CN II) is the only cranial nerve that is part of the central nervous system. CN II is a direct extension of the brain and thus is surrounded by CSF and a dural sheath. Ophthalmoscopic (funduscopic) examination of the eyes can reveal papilledema when intracranial pressure is increased. On axial imaging, flattening of the posterior aspect of the globes has been described as the most specific sign of idiopathic intracranial hypertension, also called benign intracranial hypertension or pseudotumor cerebri.
Cranial Nerve II Axial 2

Normal Anatomy and Pathologic Consideration
Sensory signals from the retina transmit posteriorly along the optic nerves until the signals join at the optic chiasm, where the medial fibers of each nerve cross to the other side. The optic chiasm is immediately superior to the pituitary gland (hypophysis) and suprasellar cistern. A large pituitary adenoma therefore can compress the crossing fibers, leading to bitemporal hemanopia (or hemianopsia), with defects in the temporal, or lateral, half of the visual field in each eye. A light object in the temporal (lateral) field of view sends light through the lens to the nasal (medial) retina, which then sends signals through the medial fibers of the optic nerves, which in turn cross midline at the optic chiasm.
Cranial Nerve II Axial 3

Normal Anatomy
The optic tract contains the lateral, or temporal, nerves of the ipsilateral optic nerve and the medial, or nasal, nerves of the contralateral optic nerve. The optic tract joins the optic chiasm to the lateral geniculate nucleus (LGN). The LGN is located within the thalamus and is the primary relay center for visual information received from the retina. A mass along the optic tract can cause contralateral hemianopia, with blocked signals at the right optic tract causing a left-sided hemianopia.
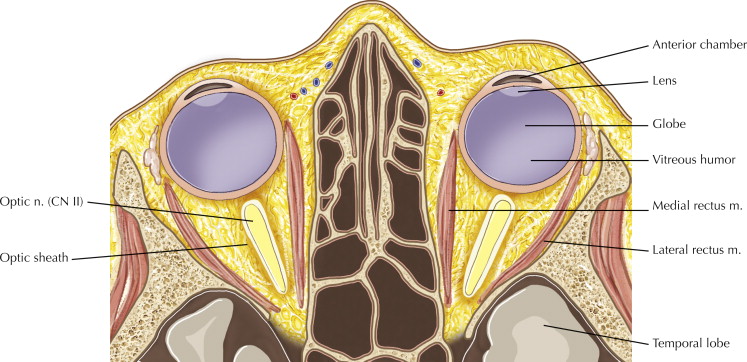
Cranial Nerve II Coronal 1

Diagnostic Consideration
The coronal plane is often the best imaging plane to assess the optic nerve (CN II). Note the ring of cerebrospinal fluid around the optic nerves. As an extension of the brain and dura, the optic nerve sheath complex is subject to the same pathology, such as a glioma of the optic nerves or meningioma of the surrounding dural sheath. This coronal plane is often the best plane to identify a mass arising from the sheath and compressing the optic nerve, versus an expansion of the optic nerve.
Diagnostic Consideration
As the optic nerve passes posteriorly in the orbit toward the apex, it is often difficult to separate the nerve from the surrounding orbital muscles and bony walls of the apex. Subtle lesions may be detected best on a coronal oblique image aligned perpendicular to the optic nerve, as seen in this image.
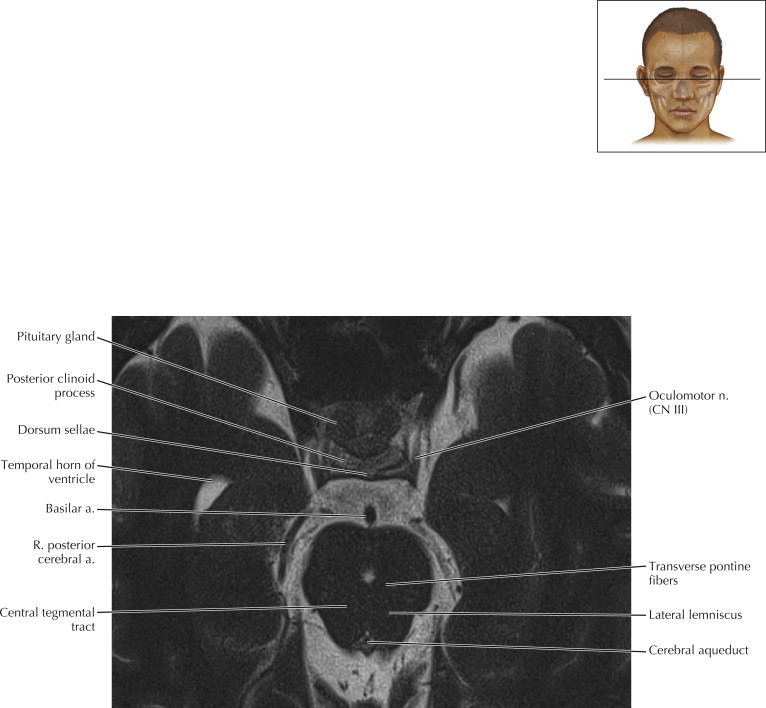
Cranial Nerve III Axial 1

Normal Anatomy
The oculomotor nerve (CN III) is the third of the 12 pairs of cranial nerves. CN III arises from two nuclei. The oculomotor nucleus originates at the level of the superior colliculus and controls the striated muscle in the levator palpebrae superioris and all extraocular muscles, except the superior oblique and lateral rectus muscles (see also Optic Coronal 6). Edinger-Westphal (accessory oculomotor) nuclei supply parasympathetic fibers to the eye through the ciliary ganglia and control the sphincter pupillae muscle for pupil constriction and the ciliary muscle for accommodation.
Fibers for the oculomotor nerve pass anteriorly from the oculomotor nucleus through the red nucleus and substantia nigra and exit the brainstem at the interpeduncular fossa.
Cranial Nerve III Axial 2

Pathologic Process
The cisternal segment of the oculomotor nerve is intimately associated with blood vessels of the circle of Willis. After exiting the brainstem, CN III passes anteriorly between the posterior cerebral and superior cerebellar arteries and parallels the posterior communicating artery before entering the cavernous sinus. An aneurysm arising from the origin of the posterior communicating artery off the internal carotid artery classically causes compression of CN III, leading to oculomotor nerve palsy.
Cranial Nerve III Coronal 1