Hypopharynx, Larynx, and Infrahyoid Neck Axial 1

Diagnostic Consideration
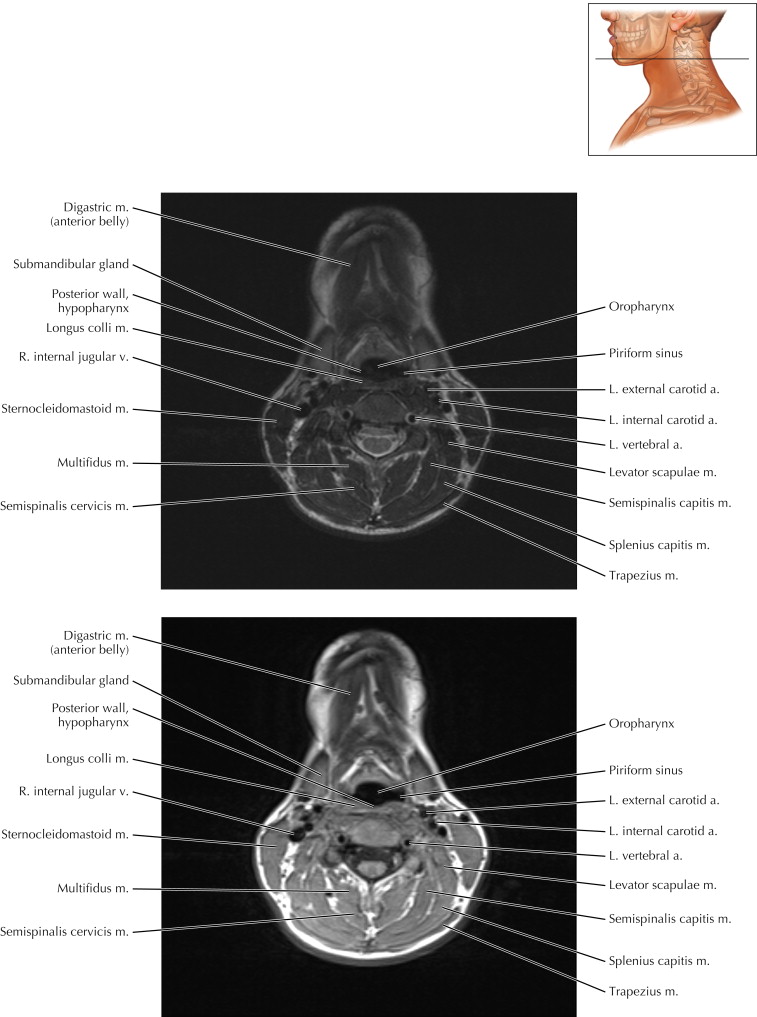
Axial 1 on the next page shows both a T2-weighted sequence (upper image) and a T1-weighted image (lower). Note that cerebrospinal fluid (CSF) around the spinal cord is bright on T2-weighted magnetic resonance imaging and dark gray on T1-weighted MRI. Usually the brightest structure on T1-weighted imaging is fat. Note that the fat is somewhat bright on T2-weighted imaging because most T2 MRIs are now performed with fast spin-echo or “turbo” spin-echo techniques that use multiple radiofrequency (RF) pulses per echo time and make fat signal appear more like water signal.
Hypopharynx, Larynx, and Infrahyoid Neck Axial 2

Diagnostic Consideration
Imaging of the neck can be difficult because many critical structures are compressed within a relatively small space. One diagnostic approach to MRI and CT of the neck is to assess the structures from central to peripheral, starting with the airway. Impending airway obstruction should be recognized early in evaluation of the neck. The airway is often the first structure to be exposed to carcinogenic agents and viruses. A primary hypopharyngeal squamous cell carcinoma may first appear as a slight asymmetry in the mucosal surfaces of the hypopharynx.
The next structure to assess is the usual site of malignancy spread, the lymph nodes, which generally follow the venous structures. The largest venous structure in the neck is the internal jugular vein, and thus the jugular lymph node chain typically contains the largest lymph nodes. The largest node is at the top of this chain, the jugulodigastric lymph node, which serves as a common point of lymphatic drainage for the head.
Next, specialized glands of the head and neck can be assessed, including parotid, submandibular, and thyroid glands. Finally, structures are assessed at the edge of a neck study, such as the brain above, the spine and top of the lungs, and structures common to many parts of the body (e.g., vessels, bones, muscles, subcutaneous tissue, skin contours).
Hypopharynx, Larynx, and Infrahyoid Neck Axial 3

Pathologic Consideration
Note the medial deviation of the right vocal cord with a focus of dark signal deep to the mucosal surface. This finding suggests previous Teflon injection for vocal cord paralysis, to help bring one cord in contact with the normal-moving cord.
Hypopharynx, Larynx, and Infrahyoid Neck Axial 4

Imaging Technique Consideration
The vocal cords should be symmetric. Medial deviation of one of the vocal cords suggests palsy, and the neuroradiologist should look carefully for a lesion or enlarged lymph node along the course of the recurrent laryngeal nerves.
Hypopharynx, Larynx, and Infrahyoid Neck Axial 5

Pathologic Process
The membranous space in the midline between the thyroid cartilage caudally and the cricoid ring caudally is the site for emergency cricothyrotomy (cricoid tracheotomy). Puncture of the cricothyroid membrane with an angiocatheter allows airway access in cases of obstruction at the level of the vocal cords or higher. The subcutaneous spaces in the midline are relatively avascular.
Hypopharynx, Larynx, and Infrahyoid Neck Axial 8

Surgical Consideration
The left innominate (brachiocephalic) vein passes immediately posterior to the suprasternal notch. It drains venous blood from the left internal jugular vein and left subclavian vein, crosses the midline, and joins right innominate vein to form the superior vena cava. In midline sternotomy, when injury involves the left innominate vein, control can be obtained by hooking a finger deep to the suprasternal notch and pulling upward.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree