16
Breast Cancer
Eugene C. Lin, Marie E. Lee, and Abass Alavi
Positron emission tomography (PET) is sensitive for detecting breast lesions that are > 1 cm, but it is not currently used as a screening modality due to cost. PET may be more cost-effective with dedicated breast imaging PET machines. High-resolution positron emission mammography (PEM) is an approved device to perform PET imaging of the breast under gentle compression. Advantages of PEM are higher spatial resolution, shorter imaging time, and reduced soft tissue attenuation. PEM may be of value to define extent of disease for surgical planning, detect multifocal or bilateral disease, and monitor response to therapy. There are ongoing trials to evaluate PEM versus breast magnetic resonance imaging (MRI).
Not infrequently, breast lesions are detected as incidental findings on PET studies performed for other indications and should be reported when discovered.
- PET. Sensitivity 89%, specificity 80%1
- PEM. Sensitivity 90%, specificity 86%2
- PEM was able to identify ductal carcinoma in situ in 10 of 11 cases.
- Tumor size. Sensitivity is highly dependent on tumor size3 and grade.4
- Detection rate for T1a and b tumors (< 1 cm) is low, and tumors < 0.5 cm (T1a) will likely not be detected.
- Sensitivity increases substantially for T2 lesions (2 to 5 cm) and T3 lesions (> 5 cm).
Comparison with Other Modalities
- Technetium (Tc) 99m-sestamibi
- The sensitivity of PET and sestamibi for breast lesions is comparable.5
- Tumors usually have higher uptake relative to normal tissue on PET than on sestamibi.
- Contrast-enhanced breast MRI
- PET is less sensitive but more specific than MRI for characterizing and detecting breast lesions.6
- MRI has superior sensitivity for lesions < 1 cm and lob ular carcinoma.
- Standardized uptake value (SUV). An SUV of 2.0 and a tumor-to-background ratio of 2.5 are both potential cutoffs between benign and malignant.7–9
- However, as there are minimal data on SUV of breast lesions, any focal abnormal uptake of fluorodeoxyglucose (FDG) should undergo further work-up.
- In general, breast cancer has lower metabolic activity than most other malignancies.
- Incidental breast uptake. Focal FDG uptake in the breast is sometimes seen incidentally and is associated with a high likelihood of malignancy.10 Initial work-up of incidentally detected breast abnormality on PET should include the standard examinations in such settings: physical examination and mammography. Contrast-enhanced breast MRI may be particularly helpful after negative initial work-up due to its high sensitivity for breast lesions. Ultrasound may also be helpful in selected circumstances.
- Delayed/dual time point imaging. Delayed imaging increases tumor visualization by PET.11 Tumors will accumulate FDG over time, whereas normal breast tissue will reveal decreased or unchanged FDG uptake. Dual time point imaging improves the sensitivity and accuracy of PET for primary breast cancer, particularly for noninvasive, small invasive, and invasive lobular and mixed carcinomas.12
- Dense breasts. Dense breasts have more FDG uptake, but the uptake in dense breasts is not substantial and therefore will not interfere with detectability of breast lesions. Even in dense breasts, the maximum SUV in normal tissue is usually relatively low (< 1).13
- Estrogen and progesterone receptors. Estrogen receptor (ER)–positive tumors have lower SUVs than ER negative tumors. Progesterone receptor status does not affect FDG uptake.14
- False negatives. Small lesions, invasive lobular carcinoma, tubular carcinoma, carcinoma in situ, ER-positive tumors
- False positives
- Inflammatory. Abscess, soft tissue inflammation, tuberculosis, sarcoidosis
- Traumatic. Postbiopsy, hematoma, seroma (Fig. 16.1) (often has a ringlike pattern of uptake)
- Benign neoplasms. Ductal adenoma, fibrous dysplasia, fibroadenomas (rare, the majority of fibroadenomas do not have significant uptake)3
PET is relatively insensitive for axillary nodal metastasis but has a high specificity. Although PET cannot replace sentinel node biopsy, a positive PET scan suggests that axillary nodal dissection could be performed instead of sentinel node biopsy.15,16 However, in practice most surgeons will want pathological proof and may biopsy abnormal nodes seen on sonography before node dissection. PET is superior to computed tomography (CT) for the detection of mediastinal and internal mammary nodal metastases.17 PET is also relatively sensitive in detecting distant metastases. PET is most valuable in staging in specific circumstances:18,19
- The primary tumor is T3 or T4.
- Stage 4 disease
- Neoadjuvant therapy is planned without axillary dissection or sentinel node sampling.
- Equivocal findings are seen on CT, ultrasound, or MRI.
- The primary lesion is medial or superior, which indicates a higher risk for internal mammary metastases or supraclavicular metastases. Patients with inner quadrant breast tumors are 6 times more likely to have isolated extra-axillary metastases identified by PET.20
- Multifocal disease: PET. Sensitivity 92%, specificity 90%
- PET is superior to conventional imaging (mammography and ultrasound combined).
- However, contrast-enhanced MRI is more sensitive than PET (Fig. 16.2).6,21
- Axillary staging
- PET does not substitute for axillary nodal dissection in most patients.
- PET: Sensitivity 61%, specificity 80%22
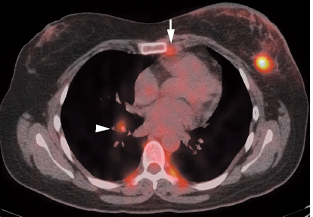
- Other nodal groups. PET is more accurate than CT for the diagnosis of internal mammary (Fig. 16.3) and mediastinal nodal metastases (Fig. 16.4, Table 16.1).17,23
- Distant staging. PET has a sensitivity of 84 to 93% and a specificity of 55 to 86% for the detection of distant metastases.17 In patients with locally advanced breast cancer, the addition of PET to the work-up for staging will result in detection of distant metastases not detected by conventional imaging in 8% of cases.24
- Bone marrow metastases
- Overall sensitivity of PET and bone scan is comparable, but PET has superior specificity.25
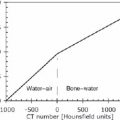
- FDG PET is superior to bone scan for detecting osteo lytic metastases, but it is inferior for visualizing osteo blastic metastases. PET is more sensitive than bone scan for mixed lytic and sclerotic metastases and substantially more sensitive for invisible (not detected on CT) metastases.26 Overall, FDG PET cannot replace a bone scan for detection of bone metastases in breast cancer due to relatively low sensitivity (56 to 74%)26,27 for blastic metastasis. However, many blastic me-tastases missed on PET could potentially be detected on the CT portion of a PET/CT study.
- Patients with more aggressive tumors may benefit more from PET, given the high likelihood of osteolytic bone metastases with these malignancies.
 Detection of Breast Masses
Detection of Breast Masses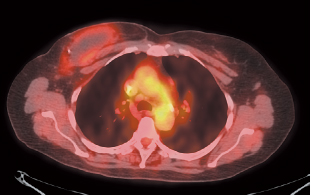
 Staging of Breast Cancer
Staging of Breast Cancer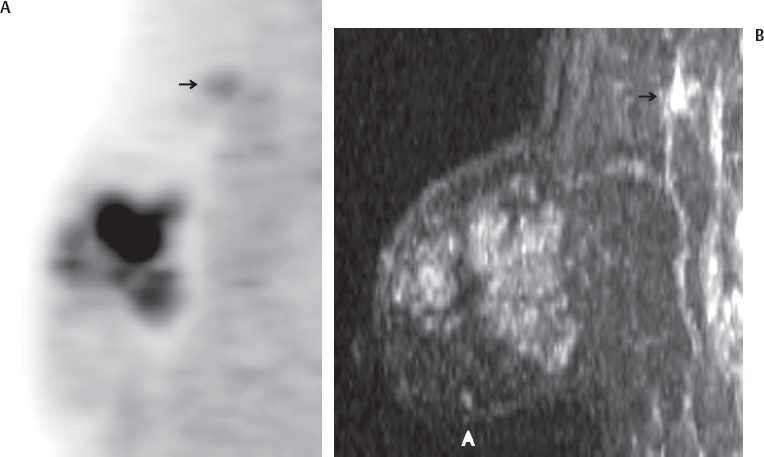
![]()