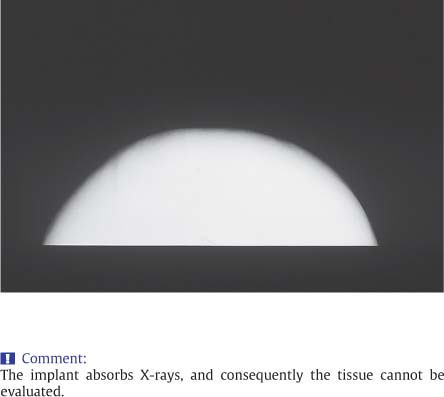
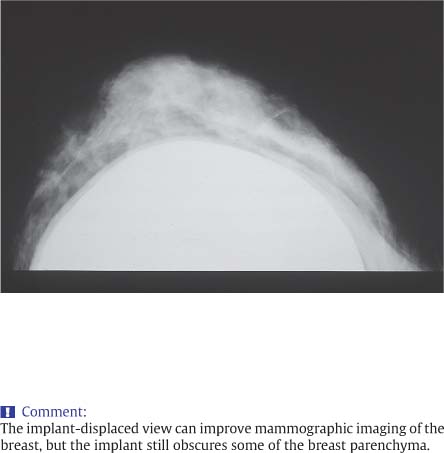
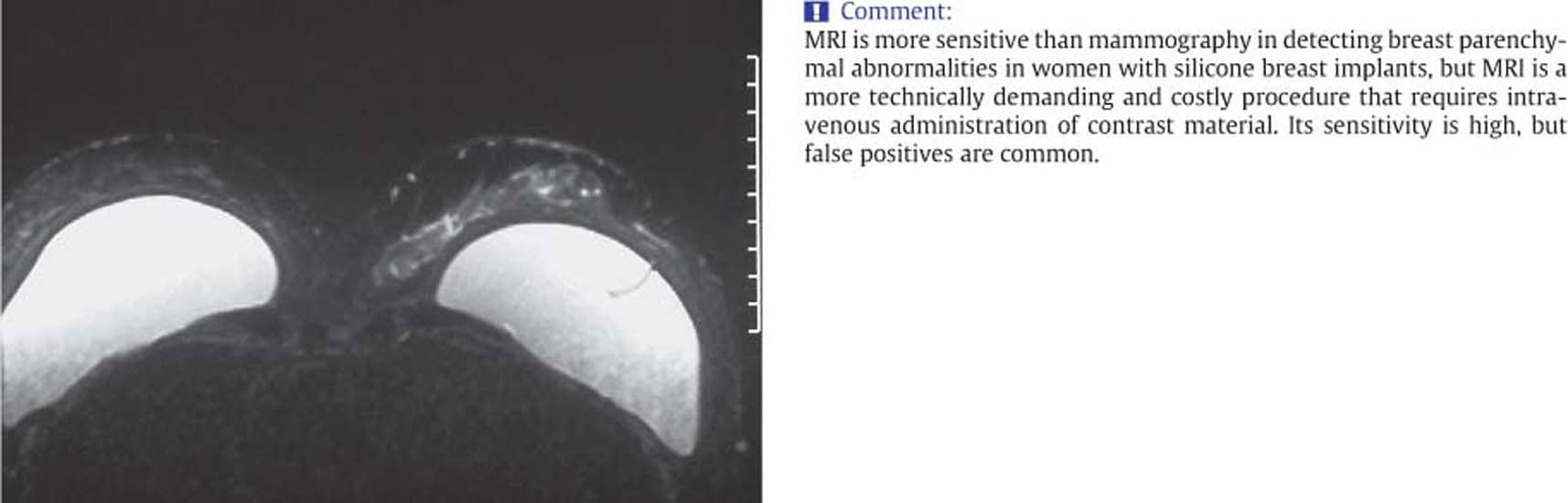
8 Breast Implants Breast implants are used for cosmetic augmentation or for breast reconstruction after mastectomy (Tables 8.1, 8.2). There are many different types of breast prostheses, each purporting to minimize complications such as fibrous encapsulation or rupture (Table 8.3). For imaging purposes, most of these may be regarded as large artificial cysts filled with either silicone gel or saline. Because implants strongly absorb X-rays, the surrounding breast tissue is compressed and difficult to evaluate with mammography until implant displacement techniques reported by G.W. Eklund in 1988 became widely adopted as the standard of care for radiographing augmented breasts (Figs. 8.1, 8.2). Recognition of some of the limitations of X-ray mammography combined with the fear, most often unfounded, of causing implant rupture, led to other techniques being sought for breast cancer screening and the detection of rupture of silicone implants. MRI is currently acknowledged as the most sensitive imaging technique for confirming or excluding both intra-and extracapsular rupture in patients with breast implants (Fig. 8.3). However, the sequences used for MRI evaluation of possible rupture are carried out without the injection of gadolinium contrast agents, and they are therefore unsuitable and inadequate for breast cancer detection. With the 1992 restrictions on silicone implants recently being relaxed by the United States Food and Drug Administration (FDA), there is interest in broadening utilization of MRI techniques so that breast cancer screening as well as diagnosis of rupture might be accomplished at the same examination. In general, the cost of MRI and the requirement for an intravenously administered contrast agent are deterrents to using MRI for screening women whose risk of breast cancer is average and for whom mammography may or may not be significantly reduced in sensitivity.
Clinical Significance
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Fig. 8.1 Mammogram of a silicone breast implant used for primary reconstruction after mastectomy.
Fig. 8.2 Mammogram following breast augmentation with a silicone implant. This view was obtained by extending as much breast tissue as possible between the compression plates while pushing the implant back against the chest wall. Some of the breast tissue is visible, but a portion is obscured.
Fig. 8.3 MRI scan following bilateral augmentation with silicone implants.
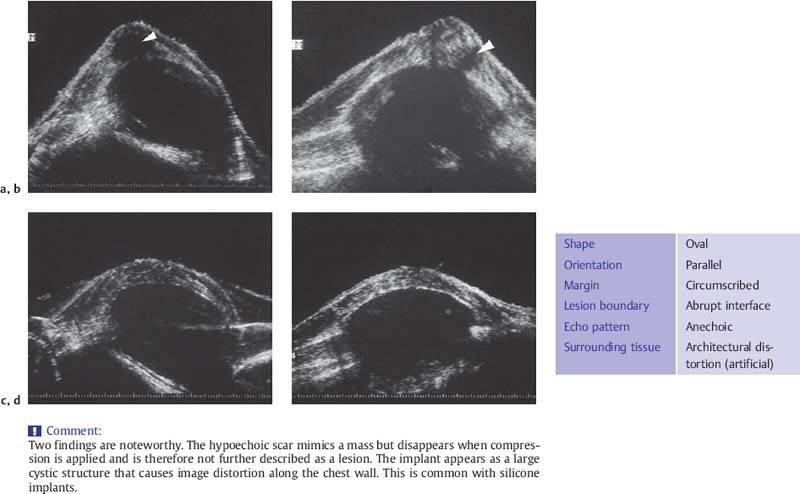
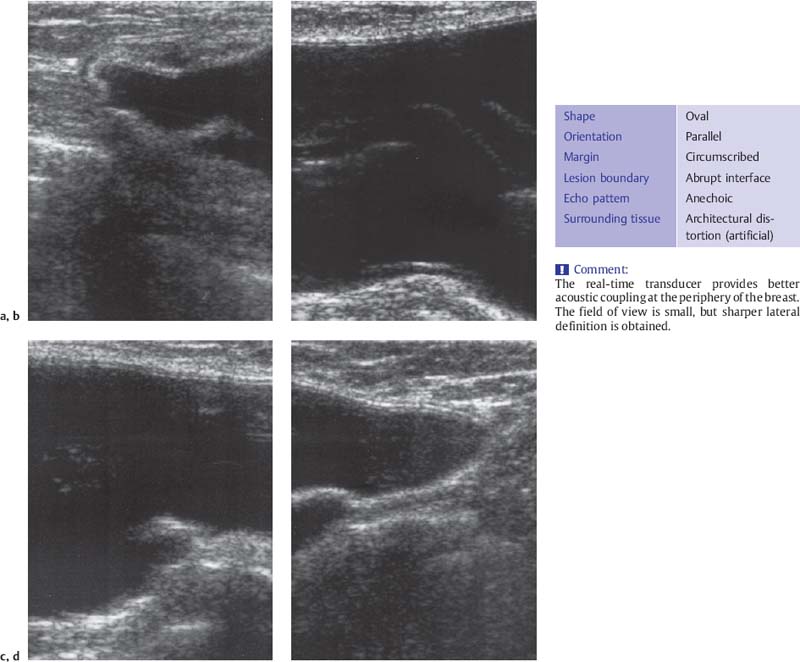
Fig. 8.4 a–d Water-bath immersion scans of silicone implants inserted through a periareolar incision.
a Transverse scan at the areolar margin. The hypoechoic scar is visible anteriorly (arrow), and below it is the anechoic implant. The chest wall is posterior.
b On the sagittal scan, the scar is visible below the nipple (arrow).
c Transverse scan with compression.
d Sagittal scan with compression. The hypoechoic scar disappears, and the implant-related artifacts are seen more clearly.
Breast ultrasound provides an important option, particularly for detecting rupture of silicone implants through the fibrous capsule or lymph nodal uptake of gel bleed, the ooze of silicone gel through micropores of the silicone polymer envelopes. Familiarity with the ultrasound findings, which may be confusing initially, will help to increase specificity in attributing the origin of a mass or other ultrasound abnormality to an implant-related phenomenon or to the breast tissue itself. Water-immersion images, which provide a broader perspective, and real-time scanning examples, can familiarize the ultrasound practitioner with the variety of sonographic manifestations. (Figs. 8.4 a–d, 8.5 a–d).
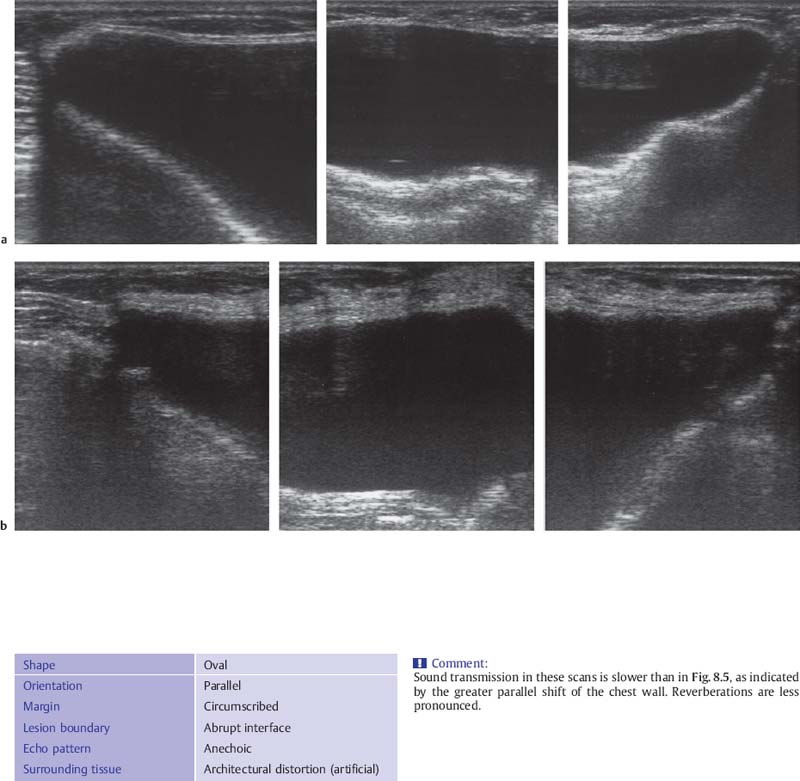
Fig. 8.5 a–d Real-time sagittal scans of a silicone implant. a Superior extension of breast. b, c Center of breast. d Inferior extension. Because of the small field of view, multiple scans are needed to cover the whole implant. Again, reverberations and projection artifacts are seen.
Sonographic Findings
Breast implants resemble large cysts and do not significantly attenuate ultrasound (Table 8.4). As in other types of examination, the instrument settings should be adjusted to eliminate reverberations and optimize image quality. It is particularly important to achieve complete breast coverage by scanning in contiguous planes. Silicone-filled implants transmit sound at a lower sound velocity than aqueous cysts or tissue, resulting in distortion of the ultrasound image and causing the implant to appear larger in an anterior–posterior dimension than its actual size (Fig. 8.4 a–d). This effect, the magnitude of which depends on the material properties of the implant, creates an apparent discontinuity at sites where the implant overlies normal tissues. In particular, the chest wall appears shifted to a deeper level. This is most apparent when the pectoralis major muscle is traced from the periphery to the implant. For real-time scanning, the field of view should be deepened, although visualization of the back wall of a silicone implant may still not be possible with the high-resolution linear broadband transducers commonly used for breast ultrasound.
Shape | Oval |
Orientation | Parallel |
Margin | Circumscribed |
Lesion boundary | Abrupt interface |
Echo pattern | Anechoic |
Posterior acoustic features | Enhancement |
Surrounding tissue | Architectural distortion (artificial) |
Different types of implants transmit sound at different velocities, resulting in varying degrees of image distortion (Figs. 8.4 a–d–8.6 a, b). Because implant placement is either subpectoral or prepectoral (subglandular), and the relationship of the implant to the muscle is easy to identify with ultrasound, the breast tissue to be examined is anterior to the implant. This is important particularly in breast cancer patients treated with mastectomy, because tumors that recur after reconstruction will develop between the implant and the skin, at skin incision sites, and for some, at the chest wall. Most of the tissue region at risk is accessible to ultrasound imaging. The significance of sonographic findings will vary according to the reason for cosmetic surgery: postmastectomy reconstruction, reconstruction after skin-sparing mastectomy, or primary augmentation for mammary hypoplasia (Figs. 8.6 a, b, 8.7 a, b).
Fig. 8.6 a, b Evaluation of the breast tissue around a silicone implant.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Augmentation of hypoplastic breasts
Augmentation of hypoplastic breasts Cosmetic breast enlargement
Cosmetic breast enlargement Symmetrization of unequal breasts
Symmetrization of unequal breasts Postmastectomy reconstruction
Postmastectomy reconstruction Inlays for replacement of tissue defects
Inlays for replacement of tissue defects Subglandular, prepectoral
Subglandular, prepectoral Subpectoral, submuscular
Subpectoral, submuscular Prepectoral (subcutaneous), subglandular
Prepectoral (subcutaneous), subglandular Intramammary (inlays)
Intramammary (inlays) Smooth-walled silicone implants
Smooth-walled silicone implants Polyurethane-coated or textured silicone implants
Polyurethane-coated or textured silicone implants Free silicone injection (obsolete)
Free silicone injection (obsolete) Saline-filled implants
Saline-filled implants Expanders (for postmastectomy reconstruction)
Expanders (for postmastectomy reconstruction) Autologous tissue (myocutaneous transfers)
Autologous tissue (myocutaneous transfers) Heterologous tissue (fat allograft)
Heterologous tissue (fat allograft)