Biopsy
9.1.1 Objective of Percutaneous Tissue Sampling
In the year 2000 in Europe, approximately 80% of open diagnostic excisional breast biopsies yielded benign results on histological examination. Since then, concrete guidelines have been developed that recommend initial percutaneous biopsies in the diagnostic work-up for ambiguous breast findings in order to reduce the number of unnecessary open breast biopsies. As well as avoiding unnecessary scars, women are spared unnecessary hospital stays and potential surgical risks.
Surgical intervention can usually be avoided if there is a history of benign results from the percutaneous tissue sampling. If the results indicate a lesion with histologically ambiguous biological potential, the further action can be determined in an interdisciplinary conference. When the findings are malignant, the subsequent treatment—usually primary surgery or a neoadjuvant treatment plan—has to be decided, and, in the case of surgery, the extent of the surgical intervention should be clearly defined preoperatively and discussed in detail with the patient.
Take Home Points
Image-Guided Minimally Invasive Biopsy
Image-guided tissue sampling for histopathological confirmation of the diagnosis and for treatment planning should be performed in cases with:
Mammographic findings of MX BI-RADS 4/5 and/or
Sonographic findings of US BI-RADS 4/5 and/or
MRI findings of MR BI-RADS 4/5.
The sample required to clarify the histological diagnosis should be obtained by core needle biopsy, vacuum-assisted biopsy, or open biopsy. The core needle biopsy and the vacuum-assisted biopsy can be done with mammographic, ultrasound, or MRI guidance.
The image-guided tissue sampling should be done with the imaging method that best visualized the findings and the procedure that is least invasive.
Primary open diagnostic excisional biopsies should be done only in exceptional cases in which an image-guided intervention is not possible or is considered to be high risk.
9.1.2 Percutaneous Tissue Sampling Equipment and Implementation
There are currently several puncture techniques available for carrying out ambulatory percutaneous breast tissue sampling. The main ones are fine needle aspiration, core needle biopsy, and vacuum-assisted biopsy.
Fine Needle Aspiration
In the second half of the twentieth century, fine needle aspiration was at first the only method and later the predominant one used for breast biopsies. Today it has largely been replaced by more complex mechanical biopsy systems.
The goal of fine needle aspiration is to extract fluid or to recover individual cells from a tissue complex for cytologic diagnosis. The lesion is punctured and a vacuum is manually created to aspirate the fluid or diagnostic material. Because diagnostic specimens acquired in this way are cytologically not assessable in up to 50% of cases, this minimally invasive technique has increasingly been abandoned.
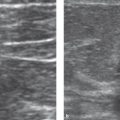
However, fine needle puncture still finds use in the diagnostic work-up of ambiguous or painful cysts. The cyst puncture is carried out under sonographic guidance using a special syringe holder (Cameco syringe pistol, Morton Medical). This holder enables the operator to guide the syringe and simultaneously pull back on the plunger to aspirate with one hand while using the other hand to guide the transducer of the ultrasound device (▶ Fig. 9.1). With correct placement of the needle tip, the intracystic fluid is aspirated and the cyst collapses (▶ Fig. 9.2). Thus, for this indication, fine needle aspiration is not only diagnostic but also therapeutic. The aspirate obtained is centrifuged and is then distributed onto a specimen slide, stained, and evaluated microscopically.
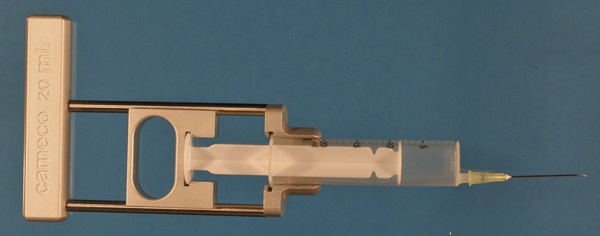
Fig. 9.1 Fine needle puncture. Cameco syringe pistol with syringe and puncture needle (Morton Medical, Cirencester, UK); puncture needle with Ciba beveled tip.
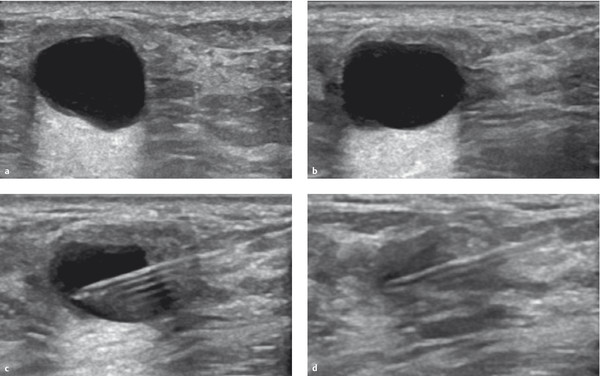
Fig. 9.2 Ultrasound-guided cyst puncture. (a) Anechoic cyst with pronounced posterior acoustic enhancement. (b) Acoustic artifact of puncture needle introduced from the right edge of the image with visualization of the needle point before the right cyst wall. (c) Puncture needle within the cyst. (d) Collapsing cyst during aspiration.
Take Home Point
Image-Guided Minimally Invasive Biopsy
Fine needle aspiration should not be used as a standard method to confirm the diagnosis of solid breast tumors.
Another application of the fine needle technique is the diagnostic work-up of ambiguous lymph nodes. Cytology provides very reliable differentiation between normal lymphocytes and metastatic cells from a breast carcinoma. In addition, fine needle puncture carries less risk than core needle biopsy, especially for punctures in the axilla with proximity to arterial blood vessels. To carry out fine needle biopsy, the needle is introduced into the lymph node under sonographic guidance. While simultaneously aspirating, the examiner repeatedly withdraws and advances the needle within the lymph node in a fan-like pattern (▶ Fig. 9.3). To end the process, the vacuum is slowly released and the needle is withdrawn. The material in the needle and the Luer adaptor of the syringe is then distributed onto a specimen slide and delivered for cytologic appraisal.
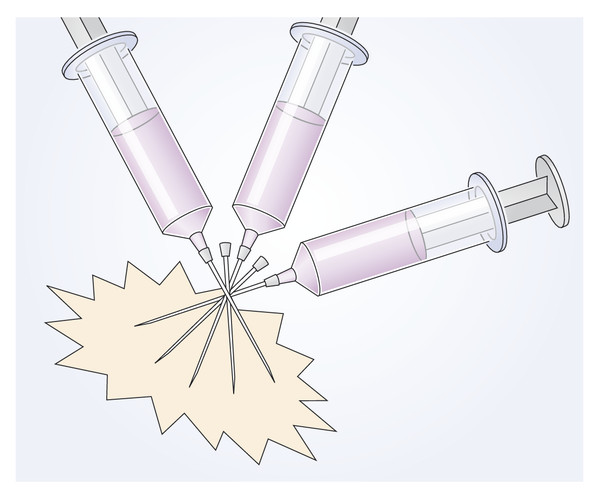
Fig. 9.3 Lymph node puncture. While simultaneously aspirating, the examiner repeatedly advances and withdraws the needle within the ambiguous lymph node in a fanlike pattern.
Core Needle Biopsy
In the late 1980s and 1990s, the high-velocity core needle biopsy was increasingly established as the standard technique for extracting tissue samples in breast diagnostics. By this means, entire cell aggregates from an ambiguous lesion can be harvested and thus yield histological diagnoses.
The biopsy needle used in the procedure has two components: an inner puncture needle and an outer hollow-bore needle. The solid puncture needle contains an approximately 2 cm long recess (notch) near the tip. When a tissue sample is being taken, this needle first penetrates into the lesion to be investigated. Then the hollow outer needle advances over the puncture needle and cuts the tissue lying within the recess from the tissue complex. Next, the biopsy needle is withdrawn from the breast to recover the tissue sample. After the spring mechanism of the needle holder has been reset, second, third, and fourth biopsies can be taken. Because it is recommended to take four tissue samples, a coaxial needle is commonly employed. This is positioned immediately before the lesion to be investigated and left in place in the breast after the first tissue sampling. Repeated piercings of the mammary gland tissue are thus avoided when taking multiple samples. The recommended diameter of the biopsy needle is 14G (ca. 2 mm) (▶ Fig. 9.4).

Fig. 9.4 Core biopsy needle. Needle with sampling notch (C.R. Bard GmbH, Karlsruhe, Germany).
Take Home Point
Image-Guided Minimally Invasive Biopsy
Percutaneous core needle biopsy is preferably performed under ultrasound guidance using a needle of 14G or larger to obtain three or more representative samples.
Typically, the high-velocity core needle biopsy is performed under sonographic guidance (▶ Fig. 9.5), allowing the procedure to be monitored in real time and the successful needle placement to be documented. In rare cases, this technique is also performed under mammographic imaging guidance with a stereotactic table in the diagnostic work-up of mammographic densities or mass lesions. An ultrasound-guided core needle biopsy can also be done to sample ambiguous MRI findings if, for example, the lesion in question is extensive and diffuse and, correspondingly, a sufficiently high accuracy of the ultrasound-guided biopsy can be assumed.
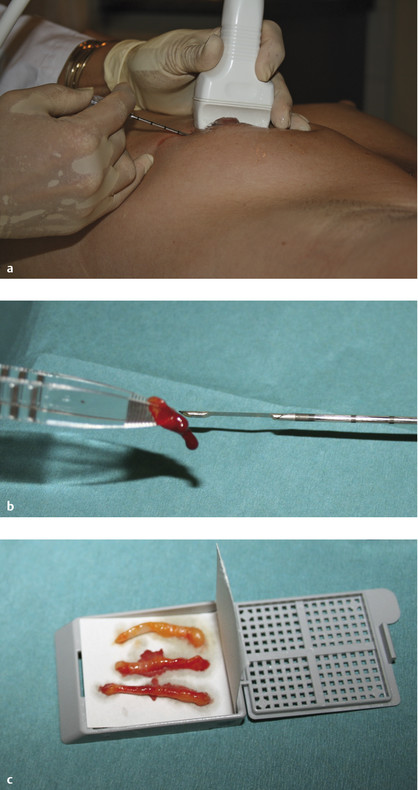
Fig. 9.5 Ultrasound-guided core needle biopsy. (a) Ultrasound transducer with coaxial needle, prepared for puncture. (b) Core needle biopsy showing tissue notch and harvested biopsy sample. (c) Three tissue samples in a histological specimen cassette (Sanowa, Leimen, Germany).
Vacuum-Assisted Biopsy
The vacuum-assisted biopsy technique was developed to improve the limited success rate of the high-velocity core needle biopsy in the diagnostic work-up of clustered microcalcifications. After the biopsy probe has been positioned under imaging guidance, a vacuum is applied to draw tissue from the target lesion into a laterally located “sampling window” near the tip of the needle. In a second step, a rotating cutting device then cuts this tissue from the tissue complex. The sampling window of the biopsy needle can be rotated 360° around the needle axis (▶ Fig. 9.6). In this manner, multiple contiguous cores of tissue can be obtained for histological examination. Depending on the diameter of the biopsy probe, the extraction of about 12 tissue samples (for a 10G probe) is recommended (▶ Fig. 9.7), yielding a volume of approximately 1 cm2 (roughly equivalent to that of a sugar cube). Because this technique extracts more extensive tissue, it features a higher success rate than core needle biopsy, especially for the diagnostic work-up of microcalcifications, for which the core needle biopsy often yields nonrepresentative tissue samples, termed a “mismatch.”
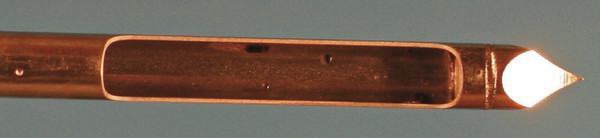
Fig. 9.6 Vacuum-assisted biopsy needle. Needle with lateral sampling window (C.R. Bard GmbH, Karlsruhe, Germany).
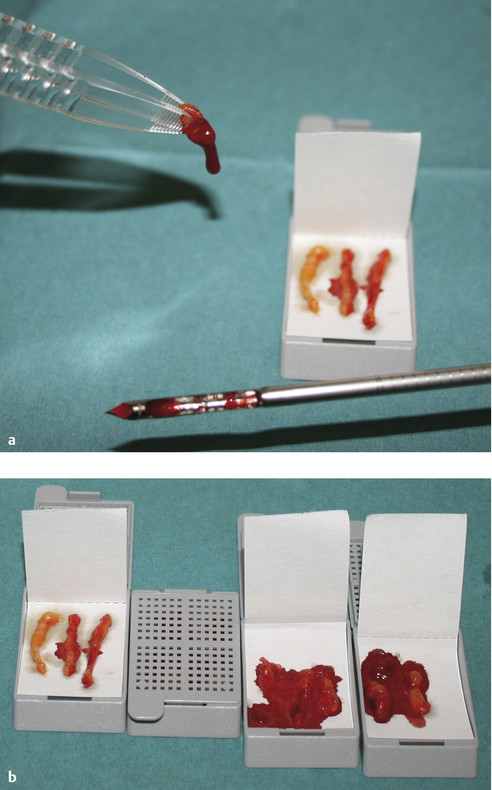
Fig. 9.7 Vacuum-assisted biopsy. (a) Vacuum-assisted biopsy needle with extracted biopsy sample. (b) Three tissue samples in each of three histological specimen cassettes (Sanowa, Leimen, Germany).
To extract sufficiently representative tissue samples for histological examination and to accommodate the rotating cutting device, vacuum-assisted biopsy probes are larger in diameter than core needle biopsy needles. Vacuum-assisted biopsy probes are usually 8 to 11G (ca. 5 mm to 2.5 mm).
Take Home Point
For a vacuum-assisted biopsy, it is recommended that 12 or more samples be obtained using a 10G probe. When using other calibers (between 8G and 11G), the number of samples taken should be adjusted to obtain an equivalent sample volume of ca. 1 cm2.
The harvested tissue samples are recovered from the breast in various ways depending on the particular vacuum-assisted biopsy system. Some systems use a collection receptacle, from which all the tissue samples can be extracted at the end of the procedure. Here the biopsy probe remains in the breast during harvesting. In other systems, each tissue sample is removed individually from the biopsy unit, requiring that the probe be completely removed from the breast for retrieval of each biopsy. In such cases, a coaxial guide needle maintains the path to the biopsy target position.
Several different vacuum-assisted biopsy systems are available that are compatible for use with MRI as well as for stereotactic use (▶ Fig. 9.8).

Fig. 9.8 Vacuum-assisted biopsy systems. (a) Vacora hand-held unit (C.R. Bard GmbH, Karlsruhe, Germany). (b) ATEC (Hologic, Bedford, MA, USA). (c) Mammotome (Mammotome, Norderstedt, Germany). (d) SenorX (C.R. Bard GmbH, Karlsruhe, Germany).
Punch Biopsy
Punch biopsy is used in the diagnostic work-up of ambiguous changes in the skin. For this, a small hollow instrument with extremely sharp metal cutting edges is placed over the lesion in question and pressed down through the skin layers after a local anesthetic has been applied (▶ Fig. 9.9). A cylinder of skin about 3 mm in diameter with about 1 cm of underlying cutaneous and subcutaneous tissue structures is recovered. The tissue cylinder can be removed from the biopsy sheath with forceps. Indications for this procedure in the breast are ambiguous inflammatory or pagetoid changes in the skin (▶ Fig. 9.10).
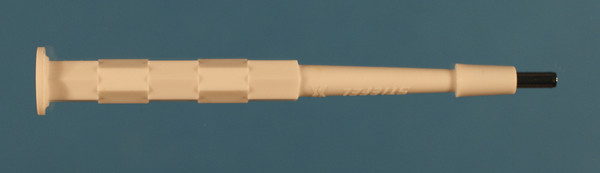
Fig. 9.9 Punch biopsy needle (Stiefel, Wächtersbach, Germany).

Fig. 9.10 Punch biopsy. Status post tissue sampling.
9.1.3 Interventional Imaging
Ultrasound-Guided Interventions
Over the last two decades, ultrasound-guided fine needle aspiration has been almost completely superseded by ultrasound-guided core needle biopsy. Sonography is the only imaging method that allows a biopsy procedure to be both monitored and documented in real time. Furthermore, ultrasound-guided interventions are simple, uncomplicated procedures that can be promptly implemented without major expense. For these reasons, ultrasound-guided core needle biopsy is by far the most common method used for the minimally invasive, histological diagnostic work-up of ambiguous findings.
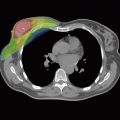
For quality assurance purposes, it is advisable to provide imaging documentation of the interventional procedure in the form of an image showing the needle’s position before it enters the lesion (pre-fire) and after it has entered the lesion (post-fire; in two planes; ▶ Fig. 9.11).
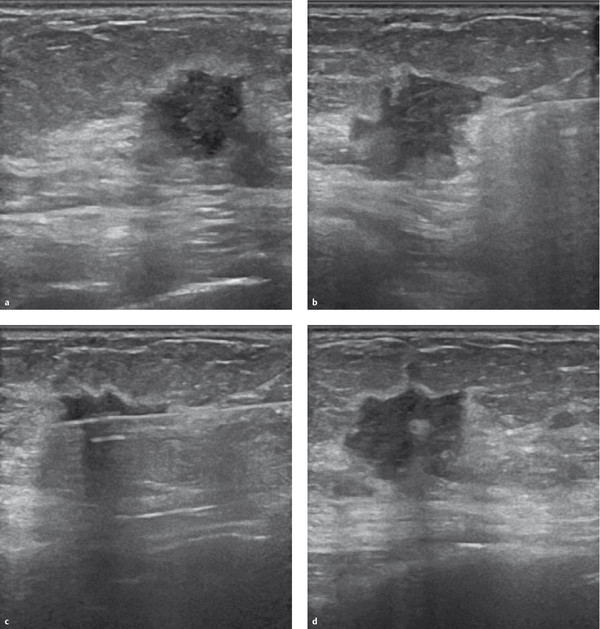
Fig. 9.11 Documentation of the ultrasound-guided core needle biopsy. (a) Hypoechoic mass with echogenic rim. (b) Acoustic artifact of the puncture needle introduced from the right edge of the image with visualization of the needle point before entering the mass (pre-fire). (c) Post-fire documentation of the puncture needle within the mass in the longitudinal axis. (d) Post-fire documentation of the puncture needle within the mass in the transverse axis.
In rare cases, sonographic imaging is also used in conjunction with therapeutic interventions. These range from the aspiration of painful cysts to the minimally invasive removal of small mass lesions. The latter applies especially to small papillomas, the resection of which is recommended because of an increased cancer risk. Vacuum-assisted biopsy is employed in therapeutic removal of tissue and can be used to completely remove lesions with a diameter up to about 1.5 cm.
Mammography-Guided Interventions (Stereotactic)
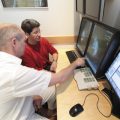
Interventional techniques utilizing mammographic imaging for guidance are termed “stereotactic interventions.” Because a mammographic image depicts only two planes, using a stereotactic table the exact location of a target lesion in the third plane must be determined by mathematical computation. The depth of a lesion can be calculated using supplemental images acquired at defined projection angles (stereo pairs). Stereotactic breast intervention systems are available for examination of patients in either the sitting or the prone position (▶ Fig. 9.12).

Fig. 9.12 Stereotactic vacuum-assisted biopsy. Positioning of the patient on a Lorad Premium Stereotactic Table (Hologic, Bedford, MA, USA). The breast hangs compressed under the table and the vacuum biopsy needle is positioned according to the target coordinates.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree