Mammography is the only imaging modality that has been validated by multiple randomized clinical trials and meta-analyses to reduce mortality from breast cancer. Although it is demonstrated to be effective in reducing mortality from breast cancer, mammography has its limitations, especially in young high-risk women with dense breasts. Other imaging modalities have been pursued as an adjunct screening modality in this population. Of these, the most widely accepted is contrast-enhanced breast magnetic resonance (MR) imaging. This article reviews current recommendations and limitations of using MR imaging of the breast to screen asymptomatic women at high risk for breast cancer.
Key points
- •
Some of the factors placing a woman at increased risk of breast cancer include mutation of the BRCA1 or BRCA2 gene, a family or personal history of breast cancer, and a history of chest radiation for treatment of Hodgkin disease.
- •
In women with a known genetic predisposition to breast cancer and in those with a history of chest irradiation, the addition of annual magnetic resonance (MR) imaging of the breast to the annual mammogram should be considered.
- •
Although additional prospective studies need to be performed, more recent retrospective studies suggest that screening by MR imaging as an adjunct to annual mammography is also beneficial in subgroups of women at intermediate risk, including women with a personal history of breast cancer or lobular carcinoma in situ.
Introduction
Breast cancer is the most common cancer diagnosed in women in the United States and a leading cause of cancer death among women. In 2012, an estimated 280,675 new cases of either invasive or in situ cancer were diagnosed, and approximately 39,510 deaths due to breast cancer occurred. A woman’s average lifetime risk for developing cancer in the United States is approximately 1 in 8. However, the risk is not evenly distributed throughout the population. Some of the factors placing a woman at increased risk include mutation of the BRCA1 or BRCA2 gene, a family or personal history of breast cancer, and a history of chest radiation for treatment of Hodgkin disease.
Mammography is the only imaging modality that has been validated by multiple randomized clinical trials and meta-analyses to reduce mortality from breast cancer. Current breast cancer screening recommendations in the United States are annual screening by mammography beginning at the age of 40 years for all women at average lifetime risk, and earlier screening in some women who are at increased risk for developing the disease at a young age. For example, mammography screening is recommended in women with a strong family history of breast cancer to begin 10 years earlier than the age at which the youngest first-degree family member was diagnosed. In women with a history of Hodgkin disease treated with mantle radiation before the age of 35, annual mammography screening is recommended beginning 8 years after completion of radiation therapy or at age 25, which ever comes later.
Although it is demonstrated to be effective in reducing mortality from breast cancer, mammography has its limitations, especially in young high-risk women with dense breasts. Compared with breast cancers occurring in women at normal risk for the disease, cancers that occur in high-risk women, and especially cancers in women with a genetic predisposition, tend to be more aggressive, develop at an earlier age, and are more difficult to detect mammographically. The sensitivity of mammography in young women with dense breasts is reported to be as low as 38% to 50%. In addition, because breast cancers developing in women at genetic risk tend to be more aggressive, approximately half of breast cancers detected by mammographic screening in these women have nodal involvement at the time of diagnosis.
Because of these shortcomings for mammography, other imaging modalities have been pursued as an adjunct screening modality in this population. Of these, the most widely accepted is contrast-enhanced breast magnetic resonance (MR) imaging. This article reviews current recommendations and limitations of using MR imaging of the breast to screen asymptomatic women at high risk for breast cancer.
Introduction
Breast cancer is the most common cancer diagnosed in women in the United States and a leading cause of cancer death among women. In 2012, an estimated 280,675 new cases of either invasive or in situ cancer were diagnosed, and approximately 39,510 deaths due to breast cancer occurred. A woman’s average lifetime risk for developing cancer in the United States is approximately 1 in 8. However, the risk is not evenly distributed throughout the population. Some of the factors placing a woman at increased risk include mutation of the BRCA1 or BRCA2 gene, a family or personal history of breast cancer, and a history of chest radiation for treatment of Hodgkin disease.
Mammography is the only imaging modality that has been validated by multiple randomized clinical trials and meta-analyses to reduce mortality from breast cancer. Current breast cancer screening recommendations in the United States are annual screening by mammography beginning at the age of 40 years for all women at average lifetime risk, and earlier screening in some women who are at increased risk for developing the disease at a young age. For example, mammography screening is recommended in women with a strong family history of breast cancer to begin 10 years earlier than the age at which the youngest first-degree family member was diagnosed. In women with a history of Hodgkin disease treated with mantle radiation before the age of 35, annual mammography screening is recommended beginning 8 years after completion of radiation therapy or at age 25, which ever comes later.
Although it is demonstrated to be effective in reducing mortality from breast cancer, mammography has its limitations, especially in young high-risk women with dense breasts. Compared with breast cancers occurring in women at normal risk for the disease, cancers that occur in high-risk women, and especially cancers in women with a genetic predisposition, tend to be more aggressive, develop at an earlier age, and are more difficult to detect mammographically. The sensitivity of mammography in young women with dense breasts is reported to be as low as 38% to 50%. In addition, because breast cancers developing in women at genetic risk tend to be more aggressive, approximately half of breast cancers detected by mammographic screening in these women have nodal involvement at the time of diagnosis.
Because of these shortcomings for mammography, other imaging modalities have been pursued as an adjunct screening modality in this population. Of these, the most widely accepted is contrast-enhanced breast magnetic resonance (MR) imaging. This article reviews current recommendations and limitations of using MR imaging of the breast to screen asymptomatic women at high risk for breast cancer.
Recommendations for breast screening using MR imaging
Several national organizations have developed similar guidelines for screening women at high risk for breast cancer. These include the American Cancer Society (ACS), the National Comprehensive Cancer Network (NCCN), and joint recommendations from the Society of Breast Imaging (SBI) and the American College of Radiology (ACR). Supplemental breast screening with MR imaging is recommended by all organizations for patients with a known BRCA1 or BRCA2 mutation and for their untested first-degree relatives, for women with a lifetime risk of 20% to 25% or greater, and for women with a history of chest irradiation. In intermediate-risk women with a 15% to 20% lifetime risk for breast cancer, the ACS states that there is insufficient evidence to recommend for or against screening using MR imaging; the NCCN and SBI/ACR guidelines state that MR imaging should be considered in these patients. These include women with a history of lobular carcinoma in situ (LCIS) or personal history of breast cancer. No organization has recommended screening with MR imaging for women with a lifetime risk of breast cancer less than 15%.
Hereditary/familial risk of breast cancer
Genetic abnormalities account for 5% to 10% of all cases of breast cancer. The most well known are mutations involving the BRCA1 and BRCA2 genes, identified in the 1990s. The prevalence of a BRCA mutation is approximately 1 in 500 in the general population and 1 in 50 in women with Jewish ancestry. The estimated risk for breast cancer by the age of 70 years ranges from 46% to 87% with a BRCA1 mutation and 37% to 84% with a BRCA2 mutation. The relative risk associated with a BRCA1 mutation declines with advancing age. Mutations in other genes, such as the TP53 and PTEN genes among others, are also known to confer a high risk for breast cancer but are much less common.
There has been increasing recognition of the role of tumor biology in BRCA1 and BRCA2 mutation carriers. BRCA1-related breast cancers differ from sporadic cancers in that they are often of higher histologic grade, tend to be of medullary or invasive ductal histopathology, show lymphocytic infiltration, and are more likely to be aneuploid and triple negative (estrogen, progesterone, and HER2/neu receptor negative). The interval cancer rate, that is, cancers detected in between annual screening, is also known to be high in BRCA mutation carriers. This is because of the rapid growth rate of tumors in these women. Studies have also shown that in BRCA1 or BRCA2 mutation carriers, the tumor growth rate is double that of nonmutation carriers and is highest in women who develop breast cancer at the youngest ages.
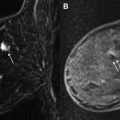
Despite the widespread evidence that mammographic screening improves mortality in the general population, there is no current evidence that mammographic screening reduces cancer mortality in high-risk mutation carriers. Multiple retrospective and prospective studies have demonstrated the limitations of mammography in high-risk patients, especially in those with a BRCA mutation. The sensitivity of mammography in young high-risk women with dense breast tissue is consistently reported to be less than 50%. In addition, of the cancers detected, 40% to 78% of the invasive cancers are greater than 1 cm in diameter and axillary nodes are involved in 20% to 56%. Explanations for the low sensitivity of mammography in these studies may include the higher breast density in younger women, a higher likelihood of rapidly growing tumors, and the more benign appearance of many BRCA1 cancers, making them more difficult to detect ( Fig. 1 ).
Beginning in the mid-1990s, multiple prospective studies were performed to evaluate the usefulness of MR imaging as an adjunctive screening tool in women with a known or likely genetic mutation predisposing them to breast cancer. Unfortunately, these studies are somewhat difficult to assess, particularly given the wide variability in the risk factors of the patient populations included. Despite these differences, all these studies showed a substantially higher sensitivity of MR imaging compared with mammography in the populations studied ( Table 1 ).
| Study, Year | Sensitivity (%)/Specificity (%) of Mammography | Sensitivity (%)/Specificity (%) of MR Imaging | % of Cancers Detected (Cancers Detected/Total Screened) | Cancer Yield from MR Imaging Alone (%) | PPV of Biopsies Based on MR Imaging Findings (%) |
|---|---|---|---|---|---|
| Kriege et al, 2004 | 40/95 | 71/90 | 2 (45/1909) | 1 (22/1909) | 57 |
| Warner et al, 2004 | 36/100 | 77/95 | 9 (22/236) | 3 (7/236) | 46 |
| Kuhl et al, 2005 | 33/97 | 91/97 | 8 (43/529) | 4 (19/529) | 50 |
| Lehman et al, 2005 | 25/NR | 100/NR | 1 (4/367) | 1 (3/367) | 17 |
| Leach et al, 2005 | 40/93 | 77/81 | 5 (33/649) | 3 (19/649) | 25 |
| Trecate et al, 2006 | 33/100 | 100/97 | 10 (12/116) | 5 (6/116) | NR |
| Lehman et al, 2007 | 33/91 | 100/79 | 4 (6/171) | 2 (4/171) | 43 |
| Sardanelli et al, 2007 | 59/NR | 94/NR | 7 (18/278) | 2 (6/278) | 60 |
Common to the data in all of these trials is that the prevalence of breast cancer in the first round of screening is extremely high at between 1.1% and 10%. This is about 10 times the expected rate in the general population. In studies in which more than 1 round of screening with MR imaging was performed, the incidence was found to be between 0.6% and 4% and indicates a continued benefit to screening with MR imaging in this population after the first screening round. Although some of these studies included women with a strong family history of breast cancer, it is not surprising that the highest cancer detection rates were reported in those studies evaluating patients with BRCA1 and BRCA12 mutations. In these trials, the sensitivity of MR imaging ranged from 71% to 100%, compared with 13% to 59% for mammography. The sensitivity for sonographic screening among these women was the same as for mammography, 13% to 65%. When data from 11 studies were combined in a meta-analysis, there was a sensitivity of 77% for MR imaging alone, 94% for a combination of MR imaging and mammography, and 39% for mammography alone. Therefore, the highest sensitivity was achieved using a combination of mammography and MR imaging. The addition of ultrasonography has not been shown to improve cancer detection rates beyond that achieved with MR imaging and mammography.
It should be appreciated that the usefulness of screening with MR imaging in BRCA1 and BRCA2 carriers may not be the same. One study has reported that the sensitivity of mammography in BRCA1 carriers was 25% compared with 62% in BRCA2 carriers. In the 599 carriers in this study, only BRCA1 carriers had any cancer diagnosed before age 30 years. In addition, screening of BRCA1 women failed to detect more cancers than in BRCA2 women; the interval cancer rates were 32% for BRCA1 women and only 6% for BRCA2 women.
Based on these trials, the recommended screening algorithm for women at high risk for hereditary breast cancer is a combination of mammography and MR imaging. A recent modeling study reported that the most efficacious screening strategy for BRCA mutation carriers in terms of increased life expectancy weighed against false-positives was to start screening with MR imaging annually at age 25 years and to add annual mammography at age 30 years, staggering the 2 examinations at 6-month intervals. Because breast cancer rarely develops before age 25 years in these women, screening should not commence earlier than this age.
History of chest irradiation
Patients with a history of pediatric or young adult cancers represent another population who are at increased risk of breast cancer as a result of treatment of their childhood cancer that included mediastinal/chest irradiation. This treatment delivers scatter radiation to the breasts, which is carcinogenic. The risk of breast cancer among these women is well established, and breast cancer is the leading cause of death in women who are long-term survivors of Hodgkin lymphoma. The risk of subsequent development of breast cancer is highest in women treated between the ages of 10 and 30 years old, because of the sensitivity of breast tissue to radiation in these 2 decades. The cumulative risk increases with the radiation dose delivered, the volume of the radiation field, and the time interval since completion of the radiation therapy.
The earliest reported breast cancer in these women developed 8 years after chest irradiation. It is estimated that by the age of 40 to 45 years, 13% to 20% of women treated with moderate to high doses of chest radiation for a pediatric cancer will be diagnosed with breast cancer. This incidence is similar to that among women with a BRCA gene mutation and is substantially higher than that in the general population, in whom the cumulative incidence of invasive breast cancer by age 45 years is only 1%.
Annual screening with mammography and MR imaging is recommended 8 years after completion of chest irradiation but not before the age of 25 years.
Several studies have evaluated breast cancer surveillance in women with a history of Hodgkin lymphoma treated with chest radiation. Most of these studies screened women using mammography alone, which detected between 27% and 90% of breast cancers. However, mammography has its limitations, especially given that approximately 50% to 60% of mammograms in women between the ages of 25 and 55 years who were treated with chest radiation have moderate to very dense breast tissue. Therefore, the ACS, the ACR, the SBI, and the Children’s Oncology Group recommend annual screening with MR imaging as an adjunct to mammography in women with a history of chest irradiation.
Two retrospective studies have evaluated the usefulness of screening with breast MR imaging in detecting otherwise occult breast cancers in women with a history of chest irradiation. Sung and colleagues reported a 4.4% incremental cancer detection rate of breast screening by MR imaging over mammography. The mammographically occult cancers detected by MR imaging were early stage, T1 invasive cancers. The positive predictive value (PPV, percentage of women in whom cancer was found) of biopsy based on MR imaging findings was 29%, which is within the accepted range for this recommendation when based on mammography. However, unlike those cancers in BRCA-positive women, which are often uncalcified, tumors in these women are more frequently associated with microcalcifications and therefore are more easily found on mammography. Of the 10 breast cancers detected in this study, 3 cancers were detected on mammography alone. The continued use of mammographic screening in this population is important and MR imaging should be used only in addition to mammography. Freitas and colleagues similarly reported a 4.1% added cancer detection rate using MR imaging to screen patients with a history of chest irradiation. In this study, the median latency from completion of radiation to breast cancer detection was 18 years. Of the 4 cancers detected on MR imaging alone, 3 were invasive cancers with a median size of 1.6 cm, and there was 1 case of ductal carcinoma in situ (DCIS), suggesting a benefit for early detection with this screening protocol.
The increased incidence of breast cancer in this population underscores the importance of breast cancer screening in this population, although the incorporation of breast cancer screening into the medical care of these women is not widely recognized. A recent study surveying women treated with chest radiation between the ages of 25 and 50 years in the United States and Canada found that almost 50% of women between the ages of 25 and 39 years had never had a mammogram, and less than 2% had undergone breast screening with MR imaging.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree