Cardiac magnetic resonance (CMR) imaging allows high-contrast, spatial, and temporal resolution imaging of the heart and related structures. The absence of ionizing radiation and the greater contrast and temporal resolution when compared with multidetector computed tomography are significant benefits of CMR. By combining different imaging sequences, cardiac abnormalities can be identified with high diagnostic accuracy. An understanding of the normal anatomic structures is of paramount importance to allow the reader to recognize such pathologic processes.
Using CMR, images may be acquired in any orientation, but typically the tomographic method of image display similar to that used in echocardiography is employed ( Fig. 13-1 ). This involves bisecting the heart with a single slice in a particular plane and then viewing adjacent parallel slices. The three most common imaging planes used are the short-axis view, the horizontal long-axis (or four-chamber) view, and the vertical long-axis (or two-chamber) view. In the short-axis view, the left ventricle is imaged perpendicular to a line from the apex to the center of the mitral valve apparatus. In the horizontal long axis-view, the lateral walls of both ventricles are sliced in such a way that both atria and ventricles are visible on the same image. In the vertical long-axis view, the plane bisects the left ventricular apex and the center of the mitral valve orifice.
Orientation of the Heart
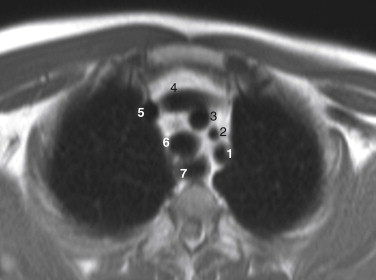
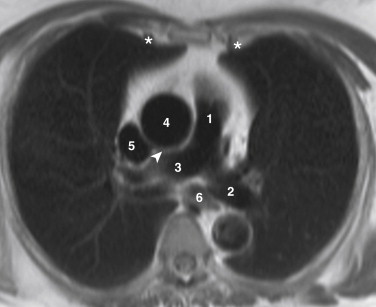
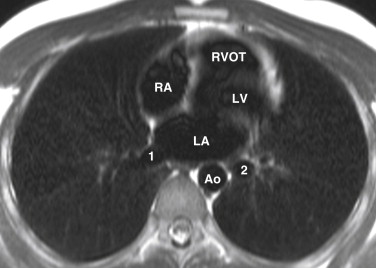
The heart is located within the middle mediastinum between the lungs. The heart lies obliquely within the chest cavity, with the interventricular septa angled approximately at 45 degrees to the transaxial plane. The atrioventricular valves (mitral and tricuspid) are at right angles to the interventricular septum. The right atrium is anterior and inferior to the left atrium, and the right ventricle forms the majority of the anterior border of the heart. The left atrium is the most posterior chamber.
Pericardium
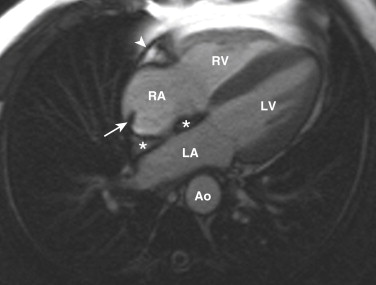
The pericardium envelops the heart within the middle mediastinum and consists of two components, the fibrous pericardium and the serosal pericardium. The fibrous pericardium, the outer component, is made of tough connective tissue and is not attached to the heart itself. Superiorly, the fibrous pericardium is continuous with the adventitia of the great vessels, and inferiorly, it is continuous with the central tendon of the diaphragm. Anteriorly, it is attached to the posterior surface of the sternum. The serosal pericardium has visceral and parietal layers. The visceral layer is attached to the myocardium and great vessels and forms the epicardium. A reflection of the visceral layer connects the epicardium with the parietal serous pericardium, which is adherent to the fibrous pericardium. These reflections also give rise to the transverse and oblique sinuses, which are potential spaces. The transverse sinus lies posterior to the aorta and pulmonary trunk and anterior to the atria. The oblique sinus is a cul de sac that lies posterior to the left atrium. Several pericardial recesses are also formed that may become visible on CMR if they contain fluid ( Fig. 13-2 ). The postcaval recess is located posterior to the junction of the right atrium and the superior vena cava (SVC) and lies between the right pulmonary artery and the right superior pulmonary vein ( Fig. 13-3 ). The right and left pulmonary venous recesses lie between the superior and inferior pulmonary veins on either side. The superior aortic recess (superior pericardial recess) extends from the transverse sinus to the right of and posterior to the ascending aorta and anterior to the proximal right pulmonary artery. The inferior aortic recess extends inferiorly from the transverse sinus between the ascending aorta and the right atrium.
Clinical Pearl
The fibrous pericardium cannot stretch. As a result, hemopericardium from a ruptured ascending aorta causes cardiac tamponade and can be rapidly fatal unless treated.
Right Atrium
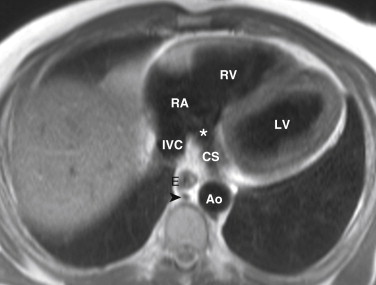
The right atrium has a posterior smooth-walled venous component, a muscular anterior component, and a right atrial appendage. The venous component receives the inferior vena cava (IVC), the SVC, and the coronary sinus. It is separated from the anterior component by a smooth internal muscular ridge called the crista terminalis that correlates with the embryonic location of the right venous valve ( Fig. 13-4 ). The IVC drains into the inferior aspect of the posterior right atrium. At the anterior and right lateral aspect of the IVC orifice is the eustachian valve or eustachian ridge. This valve is a fold of endocardium that is much larger in utero, at which time it serves to direct oxygenated blood returning from the placenta through the foramen ovale in the interatrial septum and into the left atrium. This anatomic configuration makes transeptal puncture easier using an IVC approach. The eustachian valve is continuous inferiorly with the valve of the coronary sinus (thebesian valve), which covers the lower part of the orifice of the coronary sinus. The thebesian valve may be complete, incomplete or fenestrated, or absent. The coronary sinus lies within the left atrioventricular groove and drains into the right atrium medial and superior to the IVC orifice ( Fig. 13-5 ). The pectinate muscles extend from the crista terminalis into the right atrial appendage, which is a broad-based triangular structure that extends around the anterior and right lateral aspect of the ascending aorta.
The interatrial septum separates the left atrium from the right atrium and usually bows into the right atrium because of slightly higher pressure in the left side of the heart. On the right side of the interatrial septum is the fossa ovalis. A peripheral muscular limbus with a central depression above and to the left of the orifice of the IVC represents the valve of the fossa ovalis. A small slit may be present at the superior aspect of the valve that allows communication with the left atrium. This is called a patent foramen ovale and is present in one third of people.
The normal area of the right atrium, viewed on the four-chamber view during ventricular systole and as measured on CMR, is 21 cm 2 . The upper limit of normal is 24 cm 2 .
Clinical Pearl
Patent foramen ovale may be complicated by paradoxical embolism.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree