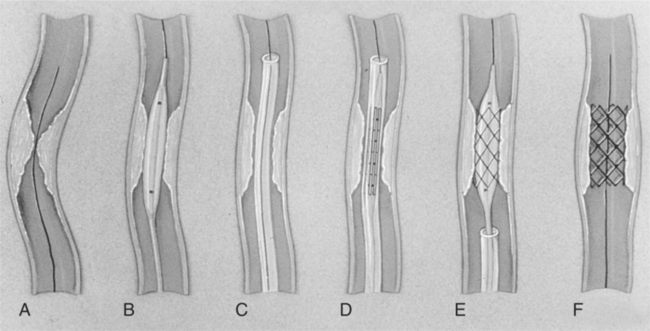
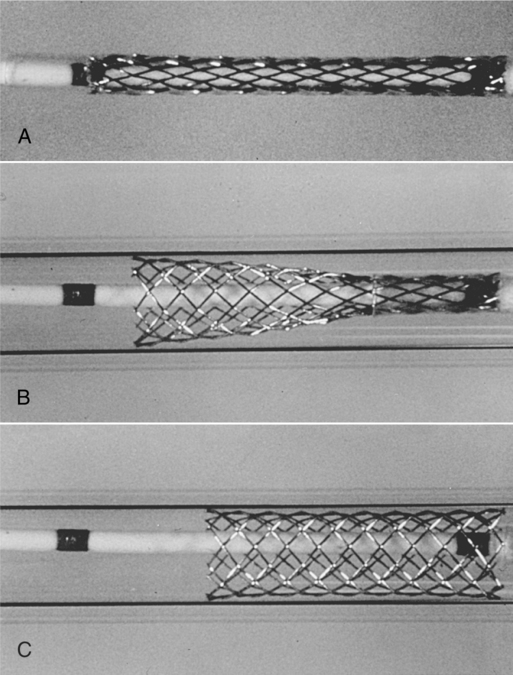
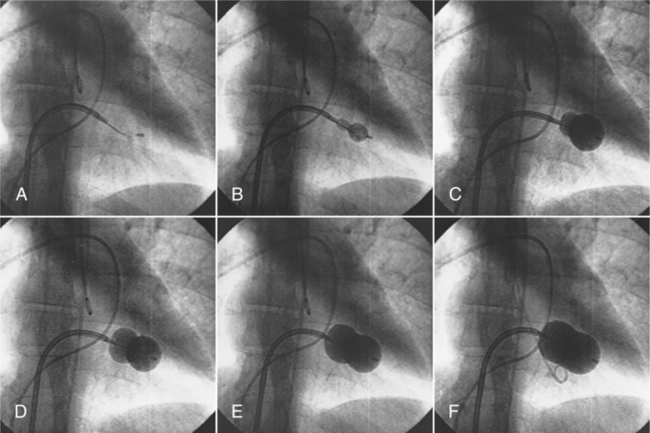
CHAPTER 18 After completing this chapter, the reader will be able to perform the following: The conventional diagnostic angiographic techniques used to demonstrate the anatomy of the heart have already been discussed in Chapter 12. In this chapter we will discuss some of the interventional techniques that are in use today. Interventional cardiology primarily focuses on several major areas: hemodynamic studies, techniques to improve the flow of blood to the myocardium, techniques to improve valve performance, extraction techniques (biopsies, foreign body removal), and electrophysiologic procedures. The techniques for transseptal left-sided heart catheterization as well as hemodynamic measurements have also been discussed in Chapter 12. These techniques can be considered as diagnostic rather than therapeutic (interventional). The balloon-stent, as its name implies, has the balloon encased in a metallic stent. The process is slightly different from the balloon catheter alone. The initial expansion of the plaque is usually accomplished by means of a separate balloon catheter, which is subsequently removed once the amount of compression has been achieved and replaced by a “stent over balloon” catheter. When this catheter is placed in the expanded lumen and the balloon is inflated, the stent is compressed into the plaque, providing a firmer support for the compressed plaque. The stent remains in place and the deflated balloon catheter can be removed, leaving a patent vessel (Fig. 18-1). Another type of stent is the self-expanding stent. This type of stent is mounted over the catheter and held in a compressed state by a sheath or membrane. When placed in the area of stenosis the covering sheath or membrane can be removed, allowing the stent to expand to its full diameter. This type of stent is held in place by means of its own expansion force against the vessel wall. Figure 18-2 illustrates the placement of a typical self-expanding stent. Restenosis of the vessel is possible with either system; however, stents have the added advantage of supporting the vessel wall in cases in which the expanding balloon may have caused it to be weakened. The newer “drug eluting” stent systems show promise in reducing the incidence of restenosis of the vessel. As discussed in Chapter 17, these stents are coated with certain drugs that reduce the incidence of restenosis. Transluminal atherectomy has already been discussed in Chapter 17. Atherectomy, also referred to as “debulking,” has the advantage over simple transluminal angioplasty of accomplishing the physical removal of the plaque from the artery. This would decrease the probability of rapid restenosis of the vessel. The procedure has some drawbacks. Among these is the relative size of the catheter system compared to angioplasty. Atherectomy systems are much larger and therefore require a larger access sheath. This fact can increase the potential for severe complications in certain at risk patients. This procedure is best utilized in cases in which the vessel lumen is larger or the stenosis is confined to the vessel orifice. Atherectomy is generally not the method of choice and is rarely applied today in the recanalization of stenotic vessels. A specially designed “Inoue balloon catheter” is usually used for the procedure. The catheter is made from polyvinyl chloride with a balloon at its distal end. The balloon has a latex band around its center so that it restricts the inflation of the center of the balloon. When it is fully inflated it will resemble an hourglass shape (Fig. 18-3). Once the opening into the left atrium has been accomplished and dilated, the deflated Inoue catheter is placed in the atrial chamber. The distal end is expanded, and the catheter is allowed to float across the valve opening. Additional inflation is applied, the proximal end begins to expand, and the balloon engages the valve. When the balloon resembles an hourglass the catheter is in place across the valve and ready for the valvuloplasty. The balloon is expanded further against the valve to complete the procedure (Fig. 18-4). Ablation is a general term referring to the process of destroying and removing tissue. This procedure is commonly accomplished using radiofrequency waves. There are several different energy sources that can be used for catheter ablation besides radiofrequency energy. These include direct electrical stimulation, microwave, laser, cryoablation, ultrasound (US), and chemical. Box 18-1 summarizes the type of energy used and its effect on tissue.
Cardiac Interventions
 List the percutaneous coronary interventional techniques
List the percutaneous coronary interventional techniques
 List and describe the various cardiac intervention procedures that can be performed
List and describe the various cardiac intervention procedures that can be performed
 Identify the indications and contraindications for the various procedures
Identify the indications and contraindications for the various procedures
 Identify the complications associated with each procedure
Identify the complications associated with each procedure
 Describe stent placement in the coronary vasculature
Describe stent placement in the coronary vasculature
 Define the debulking techniques
Define the debulking techniques
PERCUTANEOUS CORONARY INTERVENTIONS
Percutaneous Transluminal Angioplasty
Percutaneous Balloon Valvuloplasty
Percutaneous Balloon Mitral Valvuloplasty
Catheter Ablation
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Cardiac Interventions