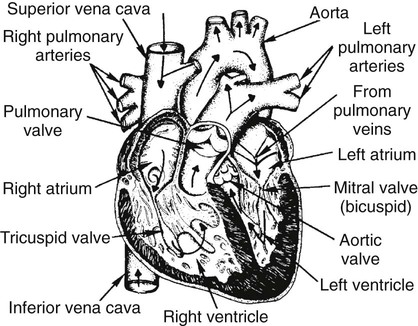
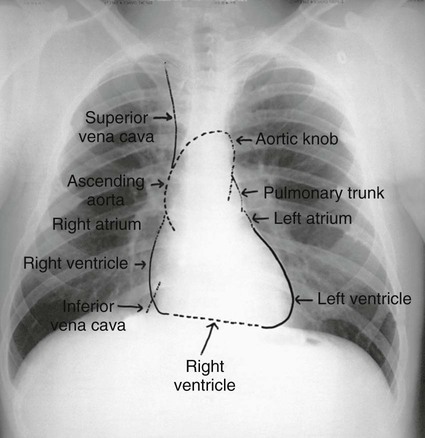
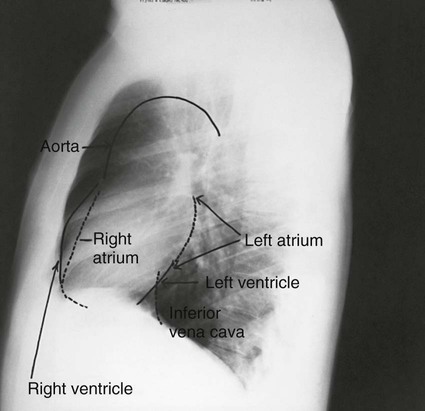
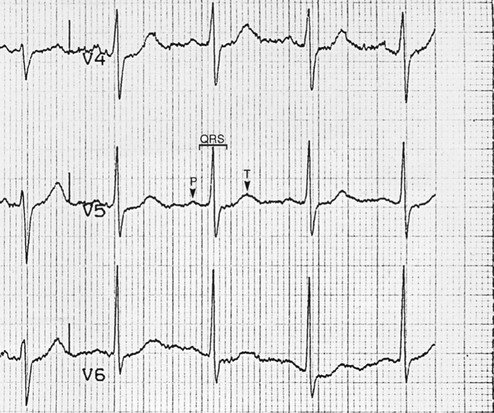
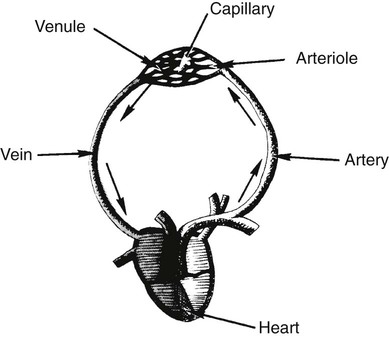
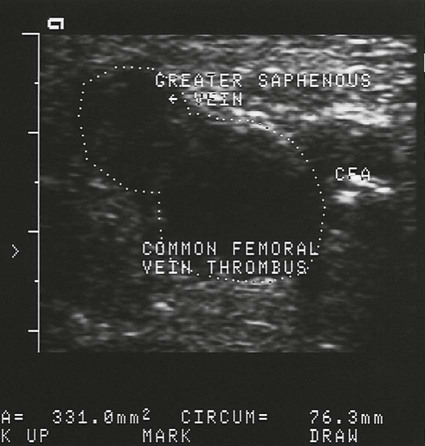
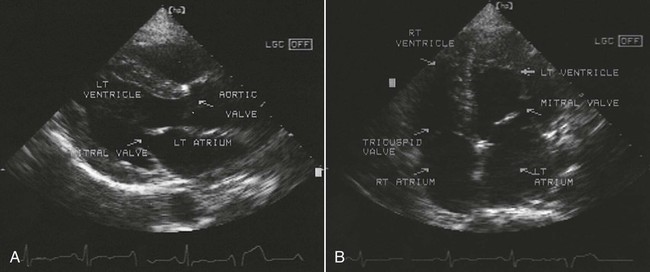
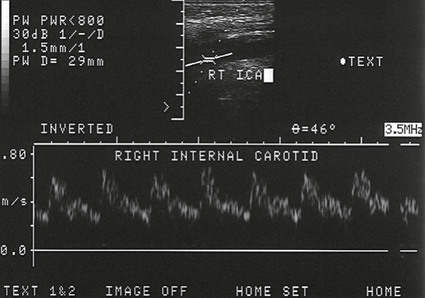
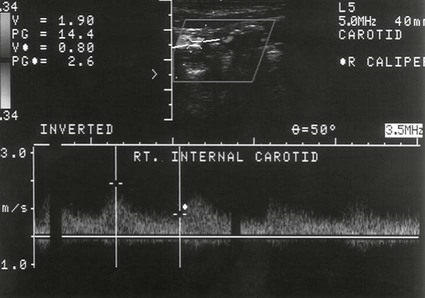
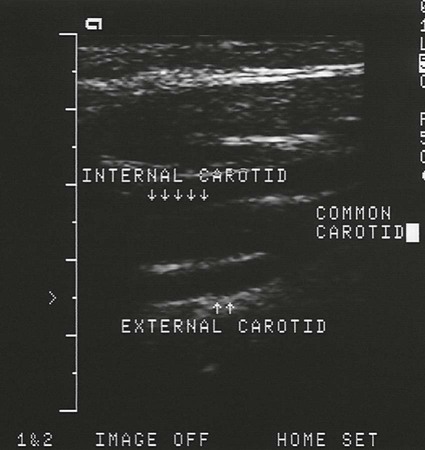
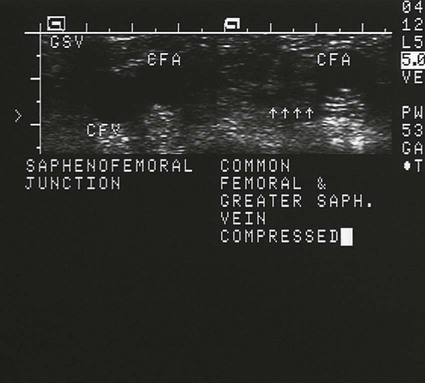
On completion of Chapter 4, the reader should be able to do the following: • Describe the anatomic components of the cardiovascular system. • Explain the appearance of the various portions of the heart on conventional chest radiographs. • Describe each segment of the cardiac cycle. • Discuss the role of other imaging modalities in the diagnosis, treatment, and management of cardiovascular disorders. • Differentiate among the major congenital anomalies of the cardiovascular system. • Identify the pathogenesis of the pathologies cited and typical treatments for them. • Describe, in general, the radiographic appearance of each of the given pathologies. The heart acts as a pump to propel the blood throughout the body via the circulatory vessels. It lies in the anterior chest within the mediastinum and is generally readily visible on a chest radiograph. The interior of the heart is divided into two upper chambers, termed the right and left atria, and two lower chambers, termed the right and left ventricles (Fig. 4-1). Note that the heart lies in an oblique plane within the mediastinum; therefore, a conventional posteroanterior (PA) chest radiograph does not clearly demonstrate all chambers of the heart. A frontal projection of the chest shows a cardiac silhouette, with two thirds of the heart lying to the left of midline; the right side is composed mainly of the right atrium, and the left side is composed mainly of the left ventricle. The right ventricle lays midline within the cardiac shadow and is located anterior to the right atrium and left ventricle. The left atrium is located midline and is the most posterior aspect of the heart (Fig. 4-2). Therefore, it is necessary to obtain a lateral projection of the chest to best demonstrate the right ventricle and the left atrium. On a lateral projection of the chest, the right ventricle constitutes the anterior portion of the cardiac silhouette, and the left atrium and the left ventricle constitute the posterior portion of the cardiac shadow (Fig. 4-3). Electrocardiography graphically demonstrates this electrical activity. The elements of an electrocardiogram (ECG) include the P wave, PR interval, QRS complex, T wave, and QT duration (Fig. 4-4). The P wave is the graphic display of the spread of the electrical impulse from the atria. The PR interval shows the amount of time required for the electrical impulse to travel from the SA node to the ventricular muscle fibers. The spread of the electrical impulse through the ventricles is displayed by the QRS complex, and the period in which the ventricles recover from the spent electrical impulse is graphically displayed by the T wave. The QT duration represents the total time from ventricular depolarization (QRS) to ventricular repolarization (T). Arteries are blood vessels that carry blood away from the heart and are generally named for their location or the organ they supply (e.g., splenic artery). They are composed of three layers. The outermost layer is termed the adventitia, the middle layer is the media, and the innermost layer is the intima. The internal, tubular structure of the vessel is termed the lumen. Veins are blood vessels that carry blood to the heart. They are composed of the same three layers; however, venous walls are thinner than arterial walls, and veins contain valves at set intervals to help with blood return to the heart. Capillaries are microscopic vessels that connect arteries and veins (Fig. 4-5). They are responsible for the exchange of substances necessary for nutrient and waste transport. Chest radiographs obtained without a good inspiration also distort heart shape and size (Figs. 4-6 and 4-7). Keep in mind that at least 10 posterior ribs should be visible within the lung fields on a chest radiograph taken with a good inspiration. The sternoclavicular joints should be an equal distance from the spine, and the scapulae should be rolled forward out of the lung fields on a well-positioned PA chest radiograph. To position a patient for a lateral chest radiograph, the arms and shoulders should be placed above the patient’s head to ensure that they are above the apices. In most institutions, chest radiography is the most commonly performed procedure, and radiographers all too often underestimate the importance of these basic radiographic principles. Well-positioned diagnostic chest radiographs are crucial in the diagnosis and treatment of cardiovascular disorders. In a normal adult, the transverse diameter of the cardiac shadow should be less than half the transverse diameter of the thorax on a PA erect chest radiograph. An enlarged heart is termed cardiomegaly (Fig. 4-8), which is indicative of many cardiovascular disorders and is a nonspecific finding. Factors affecting cardiac shape and size that are not under the technologist’s control include patient body habitus, bony thorax abnormalities, and pathologic conditions such as pneumothorax or pulmonary emphysema. Bone abnormalities of special concern include scoliosis and pectus excavatum. Individuals with pectus excavatum present a funnel-shaped depression of the sternum. The abnormal placement of the xiphoid causes displacement of the heart to the left and distortion of the cardiac shadow. Vascular lines and tubes are discussed in Chapter 3 of this text. Echocardiography encompasses a group of noninvasive sonographic (ultrasound) procedures that can provide detailed information about heart anatomy, function, and vessel patency (Fig. 4-9). Sonographic imaging may be performed using M-mode, two-dimensional (2-D) imaging, spectral Doppler, color Doppler, or stress echocardiography. Doppler sonography is an adjunct, noninvasive procedure used to study the peripheral vasculature. It has been a mainstay of vascular imaging since the 1970s and is used to determine the direction and velocity, as well as the presence or absence, of blood flow in both arteries and veins. The Doppler Effect is the principle that the sound coming toward you has a higher pitch than the sound going away from you. The return of pulsed ultrasound allows calculation of the shift in the direction of blood flow and creates a spectral display from which velocity is calculated (Fig. 4-10). The spectral signal is displayed on a strip chart or videotape. With Doppler sonography the flow of blood is not affected until any obstruction present is at least 60% complete. The percentage of stenosis present dictates the treatment of vascular disease, and usually this consists of surgery (e.g., endarterectomy). Such vascular imaging is said to be duplex in that it helps reveal physiologic characteristics, and the imaging component defines anatomy (e.g., plaque morphology). The most common conditions imaged by 2-D Doppler sonography are carotid stenosis (significantly reducing carotid angiography) (Figs. 4-11 and 4-12), lower extremity arterial stenosis, and deep venous thrombosis (Figs. 4-13 and 4-14), largely supplanting traditional venography. Blood flow may be encoded with color to differentiate blood flowing toward the transducer (red) from blood flowing away from the transducer (blue); this is termed color Doppler echocardiography. A myocardial perfusion scan is the most widely used procedure in nuclear cardiology. It may be performed on patients with chest pain of an unknown origin, to evaluate coronary artery stenosis, and as a follow-up to bypass surgery, angioplasty, or thrombolysis. It is especially useful in detecting regions of myocardial ischemia and scarring (Figs. 4-15 and 4-16). In this study, a radionuclide, usually radioactive technetium sestamibi or thallium, is injected through a vein. It concentrates in the areas of the heart that have the best blood flow. Those areas lacking blood flow demonstrate filling defects, visualized between images taken at rest and under stress. Stress may be induced by exercise on a treadmill or by the use of pharmaceuticals such as regadenoson. Myocardial perfusion scanning is performed using single photon emission computed tomography (SPECT), allowing the camera to rotate around the patient to obtain tomographic images of the heart parallel to the short and long axes of the left ventricle. SPECT myocardial perfusion scans can detect significant CAD in 90% of patients presenting with CAD. PET may also be used for imaging myocardial perfusion employing a variety of positron perfusion and metabolic agents. A PET unit is more sensitive than conventional nuclear medicine cameras, and spatial resolution is superior to that of conventional cameras. It is highly accurate for detecting CAD that interferes with blood flow to the heart muscle and can identify injured but viable heart muscle. PET can also provide quantitative data about the distribution of the radionuclide within the body.
Cardiovascular System
Anatomy and Physiology
Heart
Cardiac Cycle
Circulatory Vessels
Imaging Considerations
Radiography


Echocardiography
Nuclear Cardiology
Cardiovascular System