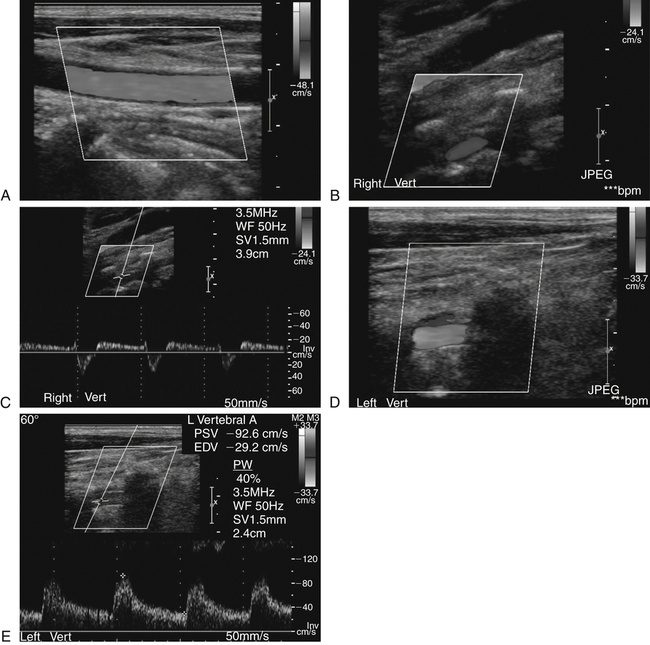
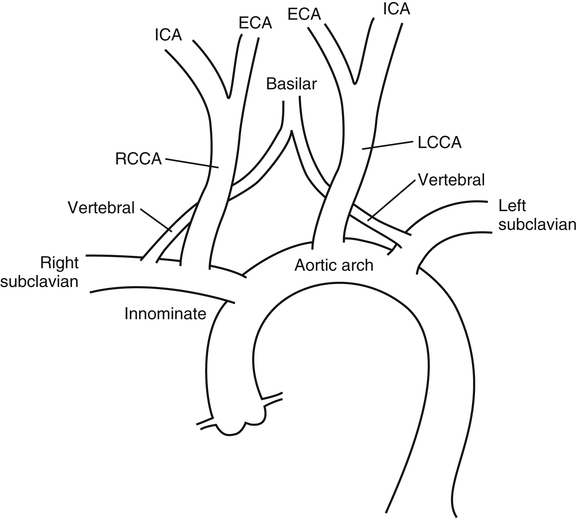
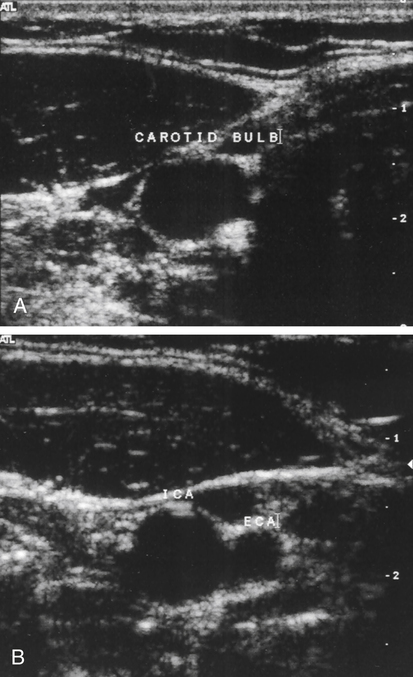
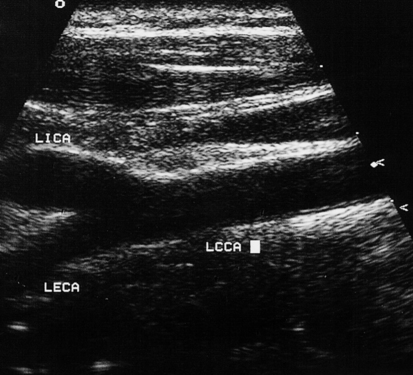
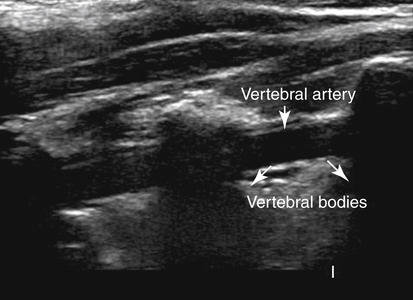
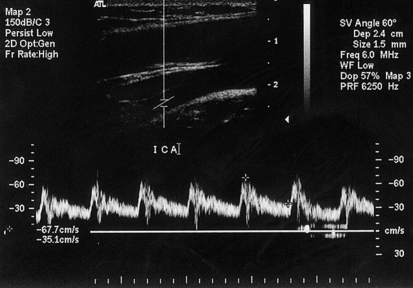
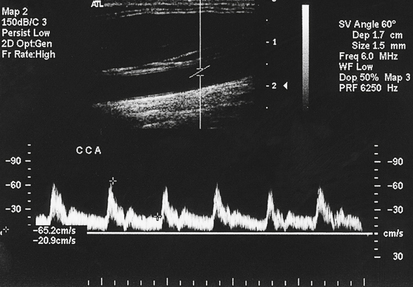
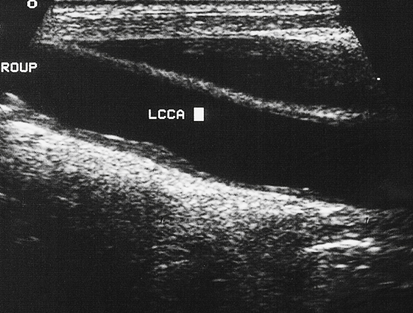
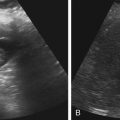
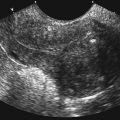
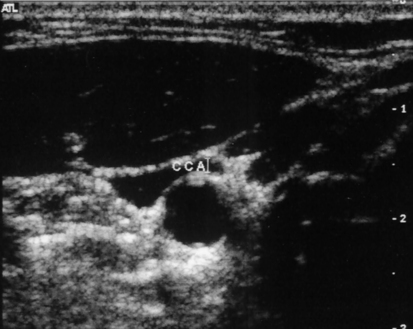
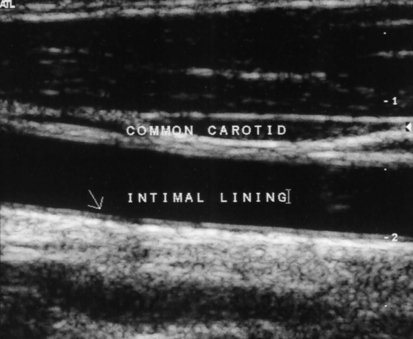
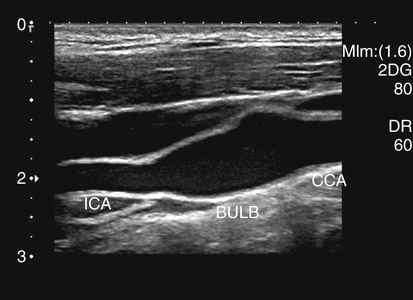
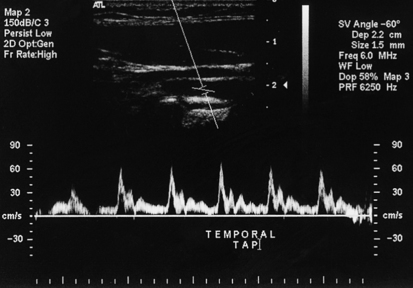
Jenni Taylor and Kelly Mumbert • Identify risk factors associated with disease of the carotid or vertebral arteries. • Identify signs and symptoms associated with abnormalities of the carotid or vertebral arteries. • Recognize the sonographic appearances of normal and abnormal carotid arteries. • Differentiate Doppler findings from normal to hemodynamically significant lesions. • Distinguish rare forms of cerebrovascular disease and cerebrovascular accidents. Stroke, also known as cerebrovascular accident, is the fourth leading cause of death in the United States, preceded by heart disease, cancer, and chronic lower respiratory diseases. Each year, approximately 795,000 people have a first stroke and an additional 185,000 have a recurrent stroke. On average, someone in the United States has a stroke every 40 seconds, which accounts for approximately 1 of every 18 deaths. Approximately three-fourths of all strokes are the result of ischemia, and one-fourth are hemorrhagic.1,2 The aortic root leaves the left ventricle with the left and right coronary arteries immediately branching off near the aortic cusp. The innominate, or brachiocephalic, is the first major branch off the aortic arch. The innominate splits into the right subclavian and right common carotid artery (CCA). The right CCA bifurcates into the right internal carotid artery (ICA) and external carotid artery (ECA). The right vertebral artery branches off the right subclavian and travels cephalad until it joins the left vertebral artery to form the basilar artery. The left CCA is the next branch directly off the aortic arch. It also bifurcates into the ICA and ECA. The third branch off the arch is the left subclavian artery, which supplies blood to the left arm. The left vertebral artery branches off the left subclavian artery and combines with the right vertebral artery to form the basilar artery, which provides blood for the posterior circulation of the brain (Fig. 34-2). The examination begins with gray-scale interrogation from a transverse plane. The transducer is usually placed in an anterolateral position near the supraclavicular notch and moved cephalad to the angle of the mandible (Fig. 34-3). During scanning in the transverse plane, notation of the orientation of the ICA and ECA as they split just past the bulb (Fig. 34-4) is helpful. The location and amount of plaque also should be noted when present. Area measurements for determination of the percent of stenosis are taken from this plane. Longitudinal views are obtained, starting again at the proximal CCA near the clavicle (Fig. 34-5). The widening of the artery at the bifurcation is identified as the carotid bulb (Fig. 34-6), seen at the more cephalad portion of the vessel. The artery splits into the ICA and ECA (Fig. 34-7). Plaque characterization should take place. Diameter measurements of a stenotic lesion should also be taken in this view. The ICA is typically the larger vessel compared with the ECA. In most patients, the ICA is posterior and lateral to the ECA and very rarely has branches off the vessel seen in the neck. The ECA may be identified by the superior thyroid artery branching off in the cervical area. The vertebral arteries originate from the subclavian artery and are imaged posterolaterally directing the sound beam until the vertebral bodies are identified. The vertebral artery is seen running between the vertebral processes (Fig. 34-8). Color and spectral Doppler are instrumental in visualization of the vertebral artery. The ICA receives approximately 80% of the blood supplied by the CCA and is needed to supply an adequate amount of blood to the brain. The Doppler spectral waveform has a low-resistance appearance, demonstrating antegrade flow in diastole (Fig. 34-9). The ECA supplies blood to the facial musculature and demonstrates a high-resistance Doppler waveform. The ECA waveform shows a sharp systolic rise and a sharp diastolic fall with a brief diastolic flow reversal. The ECA can be distinguished from the ICA with a temporal tap, which can be accomplished by locating the superficial temporal artery near the ipsilateral ear and providing quick sequential taps; this can be seen on the ECA spectral waveform during diastole (Fig. 34-10). The CCA has flow characteristics of both the ICA and the ECA. Similar to the ICA, it has antegrade flow during diastole (Fig. 34-11). A carotid sonogram examination consists of gray-scale imaging, Doppler, and color flow analysis, with each one providing support in determination of the percent of stenosis. Direct imaging of the vessel allows evaluation and characterization of plaque. A homogeneous layer along the intimal lining with smooth borders may indicate a minimal stenosis, sometimes referred to as a “fatty streak” (Fig. 34-12). A more complex plaque may show echogenic areas composed of calcium mixed with soft echoes, reflective of collagen and fibrous tissue. Sonolucent areas seen within a complex plaque would indicate areas of intraplaque hemorrhage (Fig. 34-13). Calcific plaque can be identified easily with distal acoustic shadowing (Fig. 33-14, A). Shadowing from a calcific plaque can make determination of vessel patency difficult with sonographic imaging techniques. Angiography may be used to define the degree of stenosis further (Fig. 33-14, B).
Carotid Artery Disease
Normal Anatomy
Sonographic Imaging Techniques
Doppler Imaging: Spectral Analysis
Carotid Artery Stenosis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine