1. What are the findings?
2. What is the next most appropriate study?
3. What is the proposed mechanism of injury, using the Lauge Hansen classification?
4. What is the best method of assessing the stability of this injury?
5. What is the treatment?
Maisonneuve fracture 1362
Case ranking/difficulty: ![]() Category: Trauma
Category: Trauma

Transverse displaced medial malleolus fracture.

Postsplinting image better demonstrates the posterior malleolus fracture.

High fibula fracture is seen.
Answers
1. There is a displaced medial malleolus fracture, and a minimally displaced posterior malleolus fracture. The syndesmotic space does not appear widened.
2. A tibia-fibula film is needed to exclude a Maisonneuve fracture. Stress views may also be useful, but examination under anesthesia to assess stability is usually indicated.
3. Pronation-external rotation is the usual mechanism of injury.
4. Examination under anesthesia is the best way to assess for stability.
5. A long leg cast is suitable for stable Maisonneuve injuries, and open reduction and internal fixation (ORIF) with syndesmotic screws for unstable injuries. The proximal fibula fracture is not usually fixed.
Suggested Readings
Hanson JA, Fotoohi M, Wilson AJ. Maisonneuve fracture of the fibula: implications for imaging ankle injury. AJR Am J Roentgenol. 1999;173(3):702.
Wilson FC. Fractures of the ankle: pathogenesis and treatment. J South Orthop Assoc. 2000;9(2):105-115.
Pain and clicking in the shoulder after recurrent dislocation
1. What are the characteristic MRI features of this entity?
2. What structures should be evaluated on MRI if this diagnosis is suspected?
3. What percentage of cases of this entity occurs in the direction that this injury was sustained?
4. What is a SLAP lesion?
5. What structures are at risk of damage in the acute presentation?
Hill-sachs defect (anterior dislocation of the shoulder) 526
Case ranking/difficulty: ![]() Category: Trauma
Category: Trauma
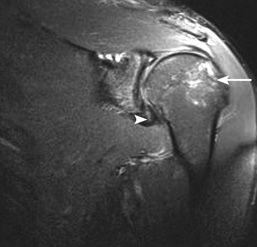
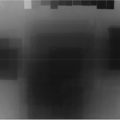
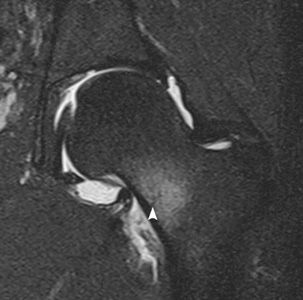
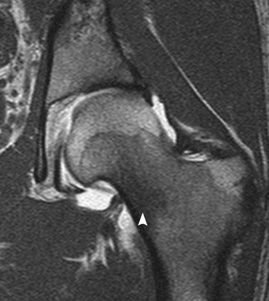
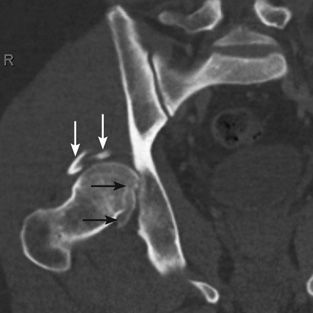
Hill-Sachs defect in posterolateral humeral head (arrow). Cleft in inferior labrum is seen consistent with a Bankart lesion (arrowhead).
Contour abnormality of humeral head is best appreciated on axial images (arrow). This must be high (at or above the level of the coracoid—arrowhead). There is extensive tearing of the anterior labrum, from the level of the inferior Bankart lesion, extending more superiorly as shown here (asterisk).

Sagittal images confirm integrity of rotator cuff muscle bulk with no denervation edema or fatty atrophy.
The coracoacromial arch, AC joint, and axillary neurovascular bundle are not damaged. The latter, in particular, is at risk of injury acutely with anterior dislocations.
Answers
1. Bankart lesions are highly specific and sensitive findings for previous anterior dislocation. A Hill-Sachs lesion is an impaction fracture of the posterolateral humeral head. A reverse Hill-Sachs lesion is a feature of posterior dislocation. Greater tuberosity fractures are also associated with anterior dislocation.
2. Careful inspection of the glenoid labrum is important to assess for Bankart lesions, in addition to bony Bankart fractures. The axillary nerve is particularly vulnerable from anterior inferior dislocation, and rotator cuff atrophy may be seen in late (missed) presentations as a result of nerve damage.
3. The vast majority of shoulder dislocations are anteroinferior (95%).
Only 5% are posterior.
4. A SLAP lesion is a superior labral tear (anterior to posterior), which often is related to overhead throwing movements, for example, in athletics/baseball. It can also be seen in the context of a large anteroinferior tear (Bankart), which extends superiorly to the level of the biceps anchor.
5. The axillary neurovascular bundle is at direct risk from anterior dislocation, and its integrity must be confirmed clinically prior to reduction.
Suggested Readings
Farin PU, Kaukanen E, Jaroma H, Harju A, Väätäinen U. Hill-Sachs lesion: sonographic detection. Skeletal Radiol. 1996;25(6):559–562.
Hendey GW, Kinlaw K. Clinically significant abnormalities in postreduction radiographs after anterior shoulder dislocation. Ann Emerg Med. 1996;28(4):399–402.
Imhoff AB, Hodler J. Correlation of MR imaging, CT arthrography, and arthroscopy of the shoulder. Bull Hosp Jt Dis. 1996;54(3):146–152.
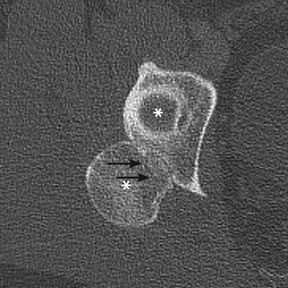
Fall from a bridge

1. What type of calcaneal fracture is demonstrated?
2. What is the mechanism of injury?
3. How often are these fractures bilateral?
4. What is the change in Böhler angle in depressed calcaneal fractures?
5. What are the associated findings in this injury?
Calcaneus fracture: tongue type 2328
Case ranking/difficulty: ![]() Category: Trauma
Category: Trauma

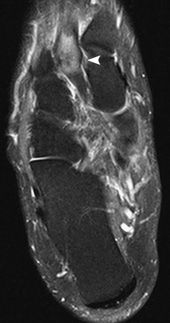
Intra-articular “tongue”-type calcaneus fracture. The secondary fracture line (arrowhead) is well depicted here, but the primary fracture line was only seen on CT.

Different patient. Other tarsal fractures are common; in this case, a fifth metatarsal avulsion (pseudo-Jones fracture) and fourth metatarsal shaft fracture.

Different patient. Comminuted joint depression intra-articular calcaneus fracture, with flattening of the Böhler angle, which now measures 13 degrees. Arrowhead points to the primary fracture line extending to the angle of Gissane (asterisk), and the arrow points to the secondary fracture line.

Joint depression type of fracture. Arrowhead points to the primary fracture line extending to the angle of Gissane, and the arrow points to the secondary fracture line.
Answers
1. There is a markedly displaced horizontal fracture of the calcaneus, known as a “tongue” fracture.
These fractures, and the more common joint depression type, are intra-articular fractures.
2. Intra-articular calcaneal fractures, both the tongue and joint depression types, are a result of high-velocity axial loading, including from parachuting and falls from a height (usually greater than 6 feet).
3. Intra-articular calcaneal fractures are bilateral in 5% to 10% of injuries.
4. The Böhler angle is measured from the anterior calcaneal process to the peak of the articular facet, and from there to the peak of the posterior tuberosity. The normal angle is 20 to 40 degrees; in depressed calcaneal fractures, that angle is less than 20 degrees.
5. The high axial loading forces can result in thoracic or lumbar compression fractures, and bilateral fractures in 10% of injuries. Pilon fractures and other tarsal fractures may occur. Soft-tissue injuries include peroneal tendon dislocation, neurovascular injuries, and flexor hallucis tendon entrapment. A compartment syndrome may occur in up to 10% of injuries.
Suggested Readings
Badillo K, Pacheco JA, Padua SO, Gomez AA, Colon E, Vidal JA. Multidetector CT evaluation of calcaneal fractures. Radiographics. 2011;31(1):81–92.
Daftary A, Haims AH, Baumgaertner MR. Fractures of the calcaneus: a review with emphasis on CT. Radiographics. 2005;25(5):1215–1226.
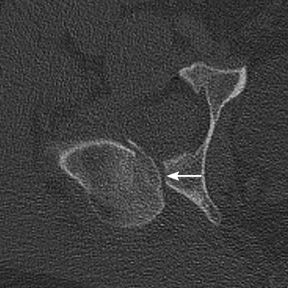
25-year-old runner presenting with severe left hip pain
1. What are the radiographic findings?
2. What is the next most appropriate study?
3. What is the differential, and the most likely diagnosis?
4. What are the types of this condition, and which has the best prognosis?
5. What is the management for this condition?
Femoral neck stress fracture 1384
Case ranking/difficulty: ![]() Category: Trauma
Category: Trauma
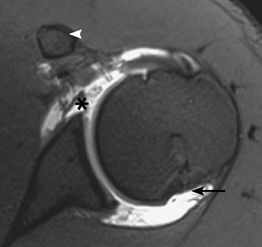
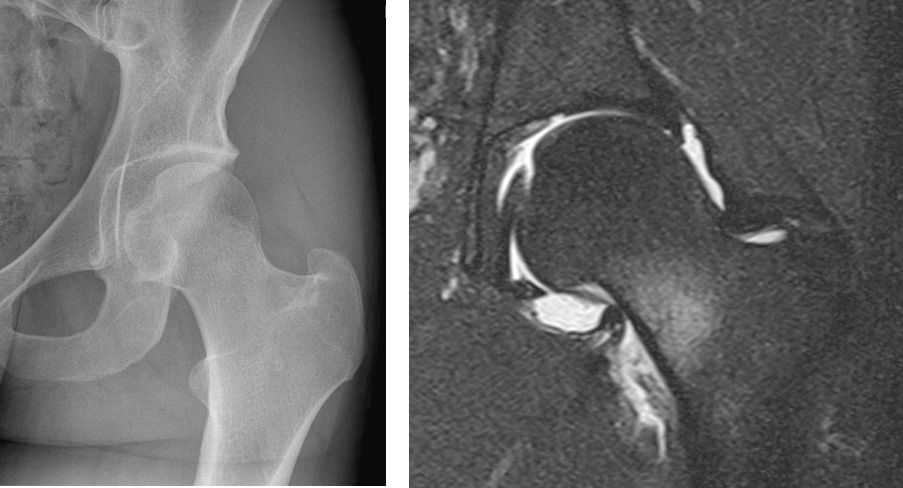
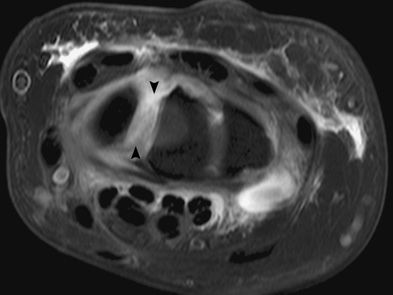
Intense bone marrow edema in the medial femoral neck with an incomplete T2 hypointense fracture line abutting the medial cortex (arrowhead).
T1-weighted image with intra-articular contrast shows T1 hypointensity in the medial femoral neck (arrowhead). An MR arthrogram was performed because a labral tear was initially suspected.

The fracture line is well appreciated.
Answers
1. The radiograph is normal.
2. An MRI would be the most sensitive and specific test to exclude a stress fracture.
3. Early septic arthritis, osteomyelitis, avascular necrosis, and stress fracture can have normal radiographs. The MRI shows centering in the medial femoral neck suggesting either stress fracture or osteoid osteoma. The absence of a nidus, and a clear fracture line, confirms a femoral neck stress fracture as the diagnosis.
4. There are 2 types of femoral neck stress fractures: the medial compressive type and the lateral tensile type.
5. Rest with gradual mobilization is the management for compressive femoral neck stress fracture. Tensile types may have to be percutaneously pinned, to avoid progression to a complete fracture.
Suggested Readings
Dorne HL, Lander PH. Spontaneous stress fractures of the femoral neck. AJR Am J Roentgenol. 1985;144(2): 343-347.
Meaney JE, Carty H. Femoral stress fractures in children. Skeletal Radiol. 1992;21(3):173–176.
Lower back pain with radicular symptoms in the legs

1. What are the radiographic findings?
2. What are the 2 main types of stress fractures?
3. What are the expected bone scan findings?
4. What are risk factors for this abnormality?
5. Which zone is most commonly involved?
Sacral insufficiency fracture 1537
Case ranking/difficulty: ![]() Category: Trauma
Category: Trauma

Bilateral sacral insufficiency fractures with compressed trabeculae.
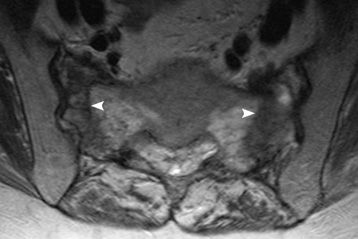
Bilateral sacral insufficiency fractures with low T1 signal fracture lines.
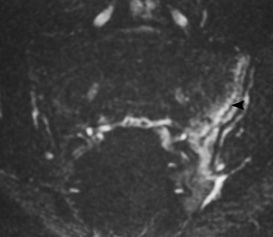
Another patient with a vertical T2 hyperintense sacral stress fracture.
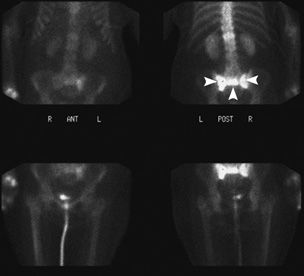
Bone scan in another patient showing the classic “H” or “Honda” sign of bilateral sacral insufficiency fractures.
Answers
1. Bilateral compressed trabeculae consistent with sacral insufficiency fractures.
2. Fatigue fractures are a result of abnormal stresses on normal bone, such as March fractures.
Insufficiency fractures are a result of normal stresses on abnormal bone.
3. Although the bone scan is nonspecific, it may show a Honda or butterfly sign, with a horizontal and 2 vertical areas of increased uptake. Depending on the acuity, the bone scan may be positive on all 3 phases.
4. Osteoporosis is a major cause of sacral insufficiency fractures. Other causes include Paget disease, steroid use, sequelae of hip arthroplasties, and pregnancy/breastfeeding (the latter can induce a temporary osteoporotic state).
5. Denis classified sacral insufficiency fractures into 3 zones:
• Zone I: Fractures in the sacral ala which are lateral to the neural foramina.
• Zone II: Fracture through the neural foramina.
• Zone III: Fracture through the body of the sacrum.
Zone I fractures are the most common.
Suggested Readings
Blake SP, Connors AM. Sacral insufficiency fracture. Br J Radiol. 2004;77(922):891–896.
Brahme SK, Cervilla V, Vint V, Cooper K, Kortman K, Resnick D. Magnetic resonance appearance of sacral insufficiency fractures. Skeletal Radiol. 1990;19(7): 489-493.
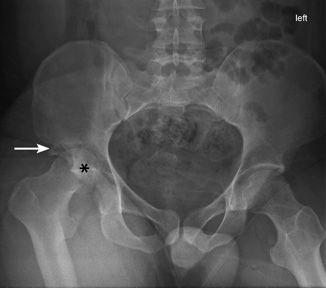
Hip pain for a few months, now progressing to limping

1. What are the radiographic findings?
2. How often is the disease bilateral?
3. What are the risk factors?
4. What are the treatment options?
5. What are the complications of this entity?
Slipped capital femoral epiphysis (SCFE) 1445
Case ranking/difficulty: ![]() Category: Trauma
Category: Trauma

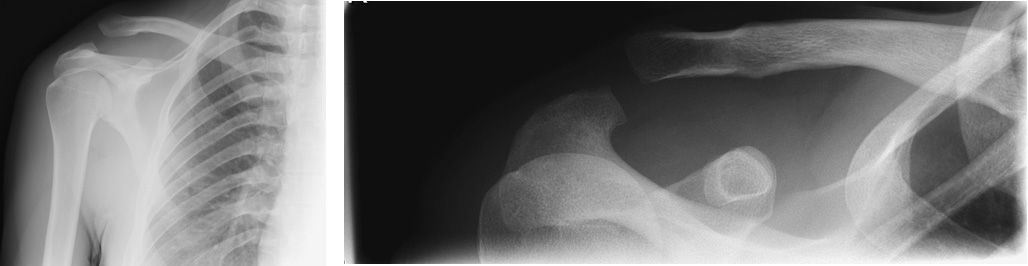
Frog lateral view of the left hip showing irregularity and widening of the growth plate, with metaphyseal sclerosis (arrowheads).

Frog lateral view with long arrows demonstrating widened and irregular epiphyseal growth plate of the left femur, and metaphyseal sclerosis (short arrows).

Widening of the left epiphyseal plate with irregularity of the growth plate suggesting a chronic stage of slip (arrow). Line of Klein is abnormal on the left, with no intersection of the epiphysis.
Answers
1. There is a blurring and irregularity of the physeal plate, posteromedial slip of the epiphysis, metaphyseal sclerosis, and abnormality of the line of Klein, which does not intersect the epiphysis. Slippage of the epiphysis gives the appearance of a reduction in height of the epiphysis because of foreshortening.
2. SCFE is bilateral in 20% of patients.
3. Obesity, rapid growth spurt, rickets, growth hormone therapy, and trauma are all predisposing factors, along with Afro-Caribbean origin.
4. Conservative treatment with analgesics and crutches in mild cases.
Surgical pinning, corrective osteotomies, hip replacement, and contralateral prophylactic pinning are the main treatment options. Pinning should be performed without correction of the slippage, as there is an increased risk of avascular necrosis if correction is attempted.
5. Avascular necrosis, chondrolysis, limb length discrepancy, pistol grip deformity, and degenerative changes are recognized complications.
Suggested Readings
Boles CA, El-Khoury GY. Slipped capital femoral epiphysis. Radiographics. 1997;17(4):809–823.
Dawes B, Jaremko JL, Balakumar J. Radiographic assessment of bone remodelling in slipped upper femoral epiphyses using Klein’s line and the α angle of femoral-acetabular impingement: a retrospective review. J Pediatr Orthop. 2011;31(2):153–158.
Fall on outstretched hand with wrist pain

1. What are the radiographic findings?
2. What is a finding on the radiographs that may be helpful?
3. What scaphoid fractures are most common in children?
4. What scaphoid fractures are most prone to avascular necrosis?
5. What parameters are used to assess whether the fracture is considered displaced?
Occult scaphoid fracture 1387
Case ranking/difficulty: ![]() Category: Trauma
Category: Trauma

The scaphoid appears normal. The scaphoid fat pad (arrow) appears preserved.

Nondisplaced fractures of the proximal scaphoid pole (arrowhead), and tubercle (arrow) are seen, with bone marrow edema. Lunate contusion is noted.
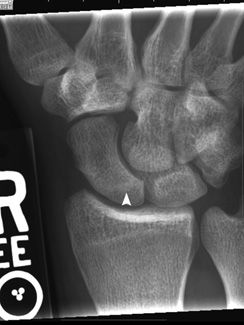
Repeat film 3 months later shows healed proximal pole fracture (arrowhead), with no evidence of avascular necrosis.
A normal scaphoid fat pad.
Answers
1. The radiographic appearances are normal. The scaphoid fat pad is preserved.
2. If a scaphoid fracture is suspected, elevation or displacement of the scaphoid fat pad may be seen. It is however not sensitive or specific. Pronator fat pad elevation occurs in distal radius fractures.
3. Tubercle fractures are most common in children. Waist fractures are most common in adults.
4. The scaphoid blood supply is from the dorsal branch of the radial artery and branches of the volar interosseous artery, and enters the scaphoid mainly through the dorsal ridge. Therefore, proximal pole fractures are the most prone to avascular necrosis because of the relatively poor perfusion.
5. Scaphoid fractures are considered to be displaced when there is a separation of 1 mm or angulation of 15 degrees.
Suggested Readings
Pierre-Jerome C, Moncayo V, Albastaki U, Terk MR. Multiple occult wrist bone injuries and joint effusions: prevalence and distribution on MRI. Emerg Radiol. 2010;17(3):179–184.
Stevenson JD, Morley D, Srivastava S, Willard C, Bhoora IG. Early CT for suspected occult scaphoid fractures. J Hand Surg Eur Vol. 2012;37(5):447–451.
Fall on the outstretched hand

1. What is the main abnormality on the radiographs of the wrist?
2. What is the normal scapholunate distance on a PA radiograph?
3. What are the most useful tests to confirm scapholunate ligament injury?
4. What are the associated complications of this injury?
5. How can scapholunate dissociation be treated?
Scapholunate dissociation 1538
Case ranking/difficulty: ![]() Category: Trauma
Category: Trauma

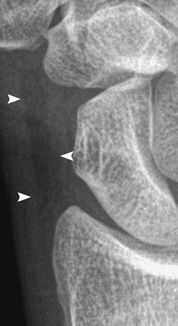
Increased scapholunate (SL) distance, with torn SL ligament.

MR arthrogram. Contrast migrates from the radioscaphoid joint to the midcarpal joint (arrow) through a torn scapholunate ligament (arrowhead).
Disrupted SL ligament.
Answers
1. There is an increased gap between scaphoid and lunate, which suggests scapholunate dissociation. The scaphoid adopts a “signet-ring” appearance, and both the scapholunate and capitolunate angles are increased.
2. Normal is 1 to 3 mm. Abnormal scapholunate (SL) distance is more than 3 mm.
3. Although CT and MR arthrograms are both very useful, CT arthrography has higher accuracy, especially for partial nonsurgical tears of the scapholunate and lunotriquetral ligaments. In many cases, nonarthrographic CT or MRI is adequate.
4. SLAC (scapholunate advanced collapse), radioscaphoid osteoarthritis, and DISI (dorsal intercalated segmental instability) are recognized complications of scapholunate dissociation.
5. Depending upon the presentation, an acute SL tear is repaired with SL ligament repair or dorsal capsulodesis. The subacute and chronic tears without arthritis are treated with SL ligament or bone-ligament-bone repair, or tenodesis. Triscaphoid arthrodesis is performed in advanced cases.
Suggested Readings
Rominger MB, Bernreuter WK, Kenney PJ, Lee DH. MR imaging of anatomy and tears of wrist ligaments. Radiographics. 1993;13(6):1233–1246.
Timins ME, Jahnke JP, Krah SF, Erickson SJ, Carrera GF. MR imaging of the major carpal stabilizing ligaments: normal anatomy and clinical examples. Radiographics. 1995;15(3):575–587.
Fell down the stairs

1. What are the radiographic findings?
2. What is the mechanism of injury?
3. What is the most severe injury in the spectrum of traumatic carpal instability?
4. What is the Terry Thomas sign?
5. What is the space of Poirier?
Perilunate dislocation 1394
Case ranking/difficulty: ![]() Category: Trauma
Category: Trauma

Marked disruption of the carpal arcs, with a displaced radial styloid fracture (arrowhead) and ulnar styloid process fracture. Numerous glass foreign bodies are also seen.

Perilunate dislocation. Lunate remains articulating with the radius, and the capitate dislocates posteriorly (arrowhead).

Postreduction radiographs show improved alignment. Some disruption of the carpal arcs persists.

Post second reduction, radial and ulnar styloid fractures are seen, with mild widening of the scapholunate space.
Answers
1. There is a radial styloid fracture with interrupted carpal arcs, perilunate dislocation, and multiple foreign bodies.
2. The mechanism is a fall on the outstretched hand held in hyperextension and ulnar deviation.
3. The spectrum is rotary subluxation of the scaphoid, perilunate dislocation, midcarpal dislocation, and finally lunate dislocation. The most severe injury is lunate dislocation.
4. This is a widened scapholunate space from scapholunate ligament tear.
5. The space between the radioscaphocapitate and palmar radiolunate ligament is known as the space of Poirier, and is a weak spot through which the lunate can dislocate into the carpal tunnel.
Suggested Readings
Linscheid RL, Dobyns JH, Beabout JW, Bryan RS. Traumatic instability of the wrist: diagnosis, classification, and pathomechanics. J Bone Joint Surg Am. 2002; 84-A(1):142.
Schreibman KL, Freeland A, Gilula LA, Yin Y. Imaging of the hand and wrist. Orthop Clin North Am. 1997;28(4): 537-582.
Motor vehicle accident
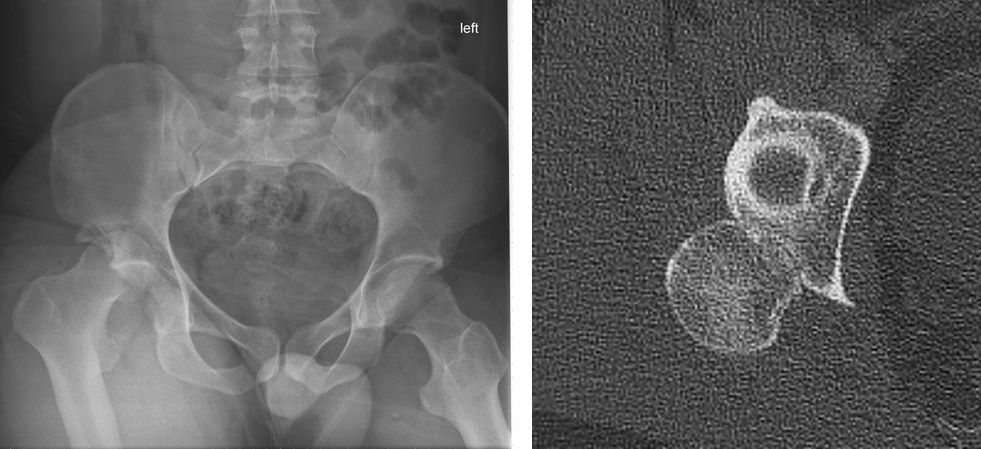
1. What is the most common direction of hip dislocation?
2. What are complications of hip fracture–dislocation?
3. What is the Pipkin classification?
4. Hip dislocations are usually isolated injuries. True or False?
5. What is the most common etiology for posterior hip dislocations?
Posterior hip dislocation 1471
Case ranking/difficulty: ![]() Category: Trauma
Category: Trauma
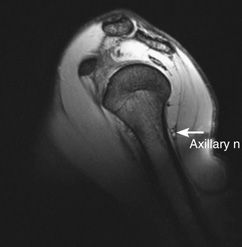
Dislocation of the right femoral head (asterisk) is demonstrated. A fracture fragment (arrow) is visible adjacent to the femoral head. The left femoral head is anatomically located.
The femoral head (inferior asterisk) is dislocated posteriorly from the acetabulum (superior asterisk). A fracture line (arrows) is visible in the femoral head.
Fracture of the posterior wall of the acetabulum (arrow) is also demonstrated.
Fracture fragments arising from the posterior wall of the acetabulum are demonstrated (white arrows). Fracture of the femoral head is demonstrated (black arrows).
Answers
1. Of traumatic hip dislocations, 90% are posterior and 10% are anterior.
2. Complications of hip fracture–dislocation include osteonecrosis of the femoral head, post-traumatic osteoarthritis, hip instability, and heterotopic ossification.
3. The Pipkin classification is a classification system of hip dislocations with associated femoral head fractures.
4. Associated injuries are common, and 95% of patients with hip dislocations also sustain injury elsewhere in the body.
5. Motor vehicle accidents account for the majority of posterior hip dislocations. Other common causes of hip dislocations include athletic injuries and falls from a height.
Suggested Readings
Lang-Stevenson A, Getty CJ. The Pipkin fracture–dislocation of the hip. Injury. 1987;18(4):264–269.
Sahin V, Karaş ES, Aksu S, Atlihan D, Turk CY, Halici M. Traumatic dislocation and fracture–dislocation of the hip: a long-term follow-up study. J Trauma. 2003;54(3):520–529.
Pain and inability to move shoulder after injury
1. What ligaments are at risk of rupture with injuries to this joint?
2. What is the recommended treatment for grade 2 injuries of this structure?
3. What activities are risk factors for this injury?
4. What imaging modalities are appropriate for imaging this structure?
5. What is the treatment of choice for grade 3 injuries of this structure?
Acromioclavicular joint subluxation 480
Case ranking/difficulty: ![]() Category: Trauma
Category: Trauma

AC and CC ligament rupture consistent with a grade 3 injury.

A further stepoff between the acromioclavicular articular margins and a posteriorly driven clavicle is a feature of grade 4 injuries.
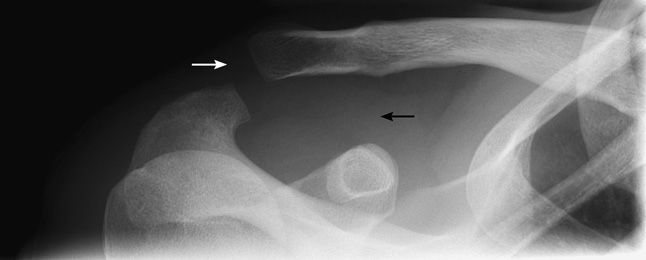
AC and CC ligament rupture on dedicated coned view of AC joint.

A posteriorly positioned clavicle is a hallmark of grade 4 injuries.
Answers
1. The acromioclavicular and coracoclavicular ligaments are at risk of rupture and may need surgical stabilization.
2. Grades 1 to 2 AC joint injuries generally have an excellent prognosis when managed conservatively. Grades 3 to 6 may require surgical repair.
3. High-energy direct trauma can lead to AC joint injury. Sports such as rugby and hockey are, therefore, high-risk activities for AC joint injury.
4. Plain film and CT are useful for demonstrating the bony injuries around the AC joint best. Ultrasound is useful for assessing the integrity of the acromioclavicular joint and coracoclavicular ligament. MRI can provide the same information, although does not allow dynamic assessment.
5. AC joint dislocations with disruption of the coracoclavicular ligament (grade 3 and above) are likely to lead to permanent disability and pain unless surgically repaired. An operation that is currently favored is the Nottingham repair, which involves passing synthetic ligament substitute material from the clavicle to the coracoid by looping it under tension around the coracoid to bring the bones closer together.
Suggested Readings
Melenevsky Y, Yablon CM, Ramappa A, Hochman MG. Clavicle and acromioclavicular joint injuries: a review of imaging, treatment, and complications. Skeletal Radiol. 2011;40(7):831–842.
Reuter RM, Hiller WD, Ainge GR, et al. Ironman triathletes: MRI assessment of the shoulder. Skeletal Radiol. 2008;37(8):737–741.
History of MVA and left-sided chest pain
1. What is the finding on the chest X-ray?
2. What is the next most appropriate study?
3. What is the most common form of this injury?
4. What is the main risk of this injury?
5. What is the most appropriate management?
Posterior sternoclavicular joint dislocation 1364
Case ranking/difficulty: ![]() Category: Trauma
Category: Trauma

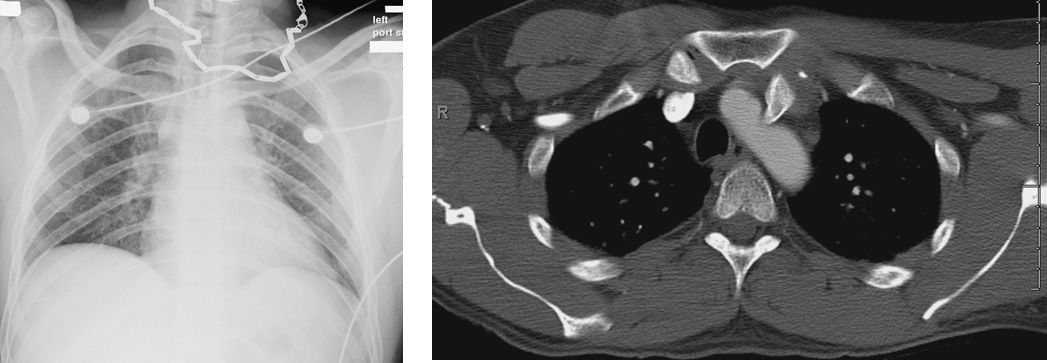
Posterior dislocation of the medial left clavicle with impingement on the aorta.

The medial left clavicle impinges on the aorta.

The medial left clavicle impinges on the aorta.
Answers
1. There is no abnormality on the chest X-ray.
2. If a sternoclavicular separation is suspected, then a CT scan is the next most appropriate study. A “serendipity” view is an AP film with 40-degree cranial angulation, used to evaluate the sternoclavicular joints.
3. This is a sternoclavicular dislocation, and the anterior form is nine times more common than the posterior form.
4. The main risk of a posterior sternoclavicular dislocation is mediastinal injury, including tracheal rupture and vascular injury.
5. Posterior sternoclavicular dislocations require closed reduction under anesthesia, or if this fails or the injury is life threatening, then open reduction.
Suggested Readings
McCulloch P, Henley BM, Linnau KF. Radiographic clues for high-energy trauma: three cases of sternoclavicular dislocation. AJR Am J Roentgenol. 2001;176(6):1534.
Patten RM, Dobbins J, Gunberg SR. Gas in the sternoclavicular joints of patients with blunt chest trauma: significance and frequency of CT findings. AJR Am J Roentgenol. 1999;172(6):1633–1635.
Tsai DW, Swiontkowski MF, Kottra CL. A case of sternoclavicular dislocation with scapulothoracic dissociation. AJR Am J Roentgenol. 1996;167(2):332.
Road traffic accident

1. What are the imaging findings?
2. What are the different types of this entity?
3. What is the usual mechanism of injury?
4. What are the components of the Lisfranc ligament?
5. What imaging modality is best for evaluation of the major ligamentous structure involved in this entity?
Lisfranc fracture dislocation 1539
Case ranking/difficulty: ![]() Category: Trauma
Category: Trauma

Fracture of the third (arrowhead) and fourth (arrow) metatarsal bases, with malalignment. Lateral cuboid fracture is also seen (asterisk).
Another patient with a sprain of the Lisfranc ligament (arrowhead) and edema in the second metatarsal base.
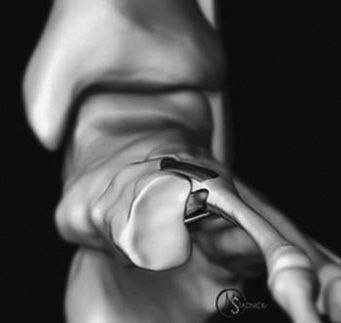
Illustration demonstrating the major components of the Lisfranc ligamentous complex. Black band is the weak dorsal band, thick grey the interosseous band, and thin white the plantar band. (Reproduced with permission from Radsource and Dr. Michael Stadnick.)
Answers
1. The plain radiograph demonstrates a homolateral Lisfranc fracture dislocation and fracture of the base of the second metatarsal with malalignment of the intercuneiform articulations.
2. Homolateral, divergent, isolated, and first ray separation are the described types of Lisfranc injury.
3. Road traffic accident, fall from height, Charcot joint, and forced plantar flexion are typical mechanisms.
4. The Lisfranc ligament connects the first cuneiform with the base of the second metatarsal. It has 3 main components: the plantar, central interosseous and dorsal bands. The ligament fails sequentially from dorsal to plantar. The dorsal capsule of the Lisfranc joint lacks sufficient reinforcement and is weak, hence dorsal subluxation is a primary feature.
5. Although the diagnosis of a Lisfranc fracture is usually made on CT, MRI best evaluates Lisfranc ligament, especially in partial tears and sprains. Of particular importance is the plantar component of the ligament: if there is a high-grade sprain or it is torn, it implies an unstable midfoot. CT and MRI also detects additional injuries not detectable on plain film.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree