Fig. 22.1
Transaortic celiac plexus block. Lateral view
Fluoroscopic imaging is one of the most commonly used methods of imaging for celiac plexus block [11]; however, there are many other imaging techniques that can be used, including computerized tomography-guided [12], injection by direct visualization [12], magnetic resonance imaging, and ultrasound-guided [13–15]. Ultrasound imaging can be used with a variety of techniques, including endoscopic [16, 17] and percutaneous [18].
In the literature, many approaches to celiac plexus blockade have been documented and include retrocrural, antecrural, transaortic, transcrural, transdiscal, and transabdominal. There are few studies on the different techniques used for celiac plexus neurolysis, and those that do exist demonstrate varying results. One study found no difference in pain scores with neurolysis between the retrocrural, transaortic, and bilateral chemical splanchnicectomy groups [10]. In a nonrandomized, prospective, case-controlled study of 59 patients [19], celiac plexus neurolysis was compared to videothorascopic splanchnicectomy. Stefaniak et al. [19] found that both techniques had similar efficacy in pain reduction and decreased daily opioid consumption. Celiac plexus neurolysis, however, was found to be associated with significantly improved physical, emotional, and social well-being with the added benefit of being less invasive [19]. As mentioned previously, in the meta-analysis by Eisenberg et al. [2], positive short-term outcomes from celiac plexus neurolysis, regardless of imaging modality used, were reported (Fig. 22.2).
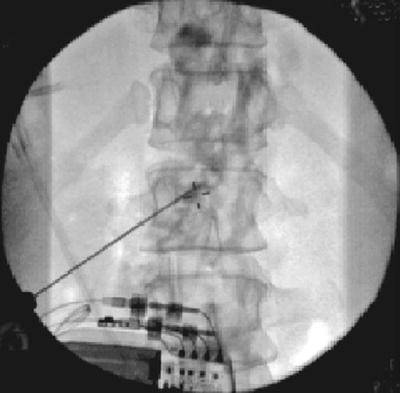
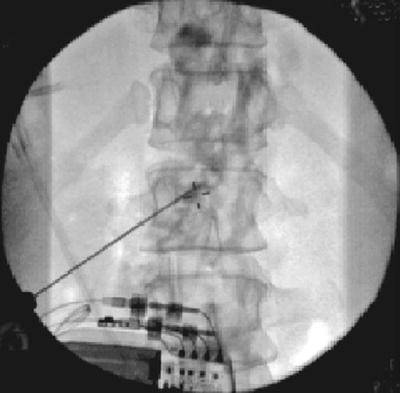
Fig. 22.2
Transaortic celiac plexus block. AP view
Splanchnic
The patient is placed in the prone position with a pillow placed under the abdomen to decrease lumbar lordosis. The inferior margins of the 12th rib are identified and marked back to the T12 vertebral body. The spinous process of the L1 vertebral body is then identified and marked. A point approximately 2 in. slightly inferior and lateral to the spinous process of L1 is marked. Typically, 20-gauge, 12-cm needles are inserted bilaterally. The needles are initially oriented 45° toward the midline and about 35° cephalad. Once bony contact with the T12 vertebra is made and the depth noted, the needles are withdrawn to the subcutaneous tissue and redirected so that the needles may walk off the lateral surface of the T12 vertebral body. The needle tips should be at the junction of the anterior and lower third of the vertebral body in a lateral view. Contrast should be confined to the midline and concentrated near the T12 vertebral body in the fluoroscopic anteroposterior view. A smooth posterior contour can be observed that corresponds to the psoas fascia on the lateral view. The contrast should be observed to be entirely retrocrural. If there is precrural spread, the needles are withdrawn slightly back through the crura of the diaphragm (Fig. 22.3) [9].


Fig. 22.3
Splanchnic nerve block. Lateral view
The use of pulsed radio-frequency ablation of the splanchnic nerves has been described as an alternative to splanchnic neurolysis for the treatment of pancreatic and upper abdominal pain [20–22]. Raj et al. [21] reported that up to 40% of patients had excellent pain relief after a thoracic splanchnic nerve block, with only 15% of patients reporting poor results in a series of 107 patients with abdominal pain [21]. One study consisting of eight patients with chronic pancreatitis and two patients with chronic abdominal pain of an unknown etiology found that splanchnic radio-frequency ablation resulted in decreased pain scores, opiate usage, and hospital admissions for pain control [20]. Garcea et al. [20] also found patients to have improvement in their level of anxiety, daily activity, mood, and overall perception of health. One advantage of radio-frequency lesioning of splanchnic nerves is that the tissue that is damaged can be more precisely controlled, allowing the technique to be safer and perhaps more reliable than with the use of a neurolytic agent [21]. Radio-frequency lesioning also has the advantage of an immediate effect unlike neurolytic agents which could take anywhere from 7 to 10 days to achieve neurolysis (Fig. 22.4) [21].


Fig. 22.4
Splanchnic nerve block. AP view
Neurolytic Agents
Neurolytic celiac plexus blocks are commonly performed with 50–100% alcohol and 6–12% phenol. The mechanisms of action of alcohol include dehydration; extraction of phospholipids, cholesterol, and cerebrosides; and precipitation of mucoproteins and lipoproteins. These actions result in sclerosis and separation of the myelin sheath, edematous Schwann cells, and axons. The basal lamina of the Schwann cell tube is often spared, and the axon can regenerate along the previous course; if the ganglion is injected, it may produce cell destruction with no subsequent regeneration [23]. The mechanism of action of phenol depends on its concentration, protein denaturation occurs at concentrations less than 5%, and concentrations higher than 5% produce protein coagulation, nonspecific segmental demyelination, and orthograde degeneration [24, 25]. Axons of all sizes are affected and appear edematous, except posterior root ganglia which are unaffected by phenol. Some have suggested that phenol has a greater affinity for vascular than neuronal tissue [23, 26].
There are advantages and disadvantages to both alcohol and phenol as neurolytic agents. Alcohol is an irritant for soft tissue and is associated with a burning dysesthesia that warrants prior or simultaneous injection of local anesthetic. Alcohol spreads quickly from the injection site due to high solubility in the body. The higher solubility of alcohol can make it challenging to reach the targeted nerve; this also makes a larger volume of injectate necessary to increase the chance of neurolysis of the targeted tissue while also increasing the likelihood of damage to surrounding nerves. An advantage of not using a local anesthetic is that pain along the target nerve will confirm correct needle placement [23]. Phenol used in a concentration of 5–10% causes neurolysis by causing protein coagulation and necrosis when applied to nerves [24, 25]. Phenol is suspended in glycerol, and its high viscosity limits its spread. Phenol also has an advantage of being painless on injection. Just like alcohol, phenol has also been associated with the development of neuritis. However, there are many more case reports of persistent paraplegia following neurolysis with alcohol than with phenol. A study published by Abdalla and Schell [13] reviewed all of the previously reported cases (1974–1998) of temporary or permanent paralysis following neurolysis with alcohol or phenol. In that study, 10/11 cases involved alcohol as the neurolytic agent versus 1/11 in which phenol was used.
Complications may be related to spread of neurolytics to nearby structures, resulting in deafferentation pain of somatic nerves and neuritis. The intravascular spread of the neurolytic solution to the spinal cord may occur with any paraspinal block using neurolytics [13, 27–33]. Even with direct intraoperative visualization, administration of a neurolytic has been reported to lead to permanent paraplegia [13]. Alcohol results in pain upon injection and has been associated with neuritis following neurolysis. With a retrocrural approach, the spread of the neurolytic agent is limited by the diaphragm. Higher quantities of neurolytic agents are often used for the retrocrural approach, and the spread of the agent may cause increased risk of neurolysis to the somatic nerve roots with resulting paraplegia and/or neuritis [13].
Efficacy
The first double-blinded, randomized, controlled trial that studied the benefits of chemical splanchnicectomy in pancreatic cancer patients was done by Lillemoe et al. [5]. Chemical splanchnicectomy was performed with alcohol versus saline placebo at time of exploratory laparotomy for biopsy, staging, and possible palliative gastrointestinal bypass. In follow-up, mean pain scores were found to be lower in the alcohol group at 2, 4, and 6 months (p < 0.05). In this study, patients who underwent splanchnicectomy had a longer duration of pain relief (7.2 vs. 3 months of placebo, p < 0.0001) and needed lesser amounts of opioids compared to patients who received the placebo (46 and 68%, respectively, p < 0.05). Patients in both groups received rescue neurolytic celiac blocks, but time to rescue was significantly longer in those who underwent chemical intervention. In patients who did not have preoperative pain, chemical splanchnicectomy significantly reduced later pain scores and delayed or prevented onset of pain (p < 0.05).
Another double-blinded, randomized, control trial more recently conducted by Wong et al. [34] randomized 100 patients into two groups that received either a neurolytic celiac plexus block or analgesic therapy alone with a sham injection. This resulted in a greater reduction in pain intensity (p = 0.01) and showed improvement in quality of life (p = 0.001) in the first week after randomization in the neurolytic block group. In the first 6 weeks, fewer patients reported moderate to severe pain (rated as ≥5/10 on pain scale) in the neurolytic block group versus those in the systemic analgesic group (14 and 40%, respectively, p = 0.005). Although fewer patients in the neurolysis group required rescue blocks versus systemic analgesic group (6 and 20%, respectively), this finding was not statistically significant (p = 0.07). Overall, there was no significant difference between the groups for opioid consumption, frequency of adverse opioid effects, quality of life, and survival. However, pain relief was improved in the neurolysis group. In a randomized, double-blind study by Polati et al. [35], the efficacy of neurolytic CPB was compared with pharmacological therapy in the treatment of pain from pancreatic cancer. Twenty-four patients were divided into two groups: 12 patients underwent neurolytic CPB (group 1), and 12 were treated with pharmacological therapy (group 2). Immediate and long-term efficacy, mean analgesic consumption, mortality, and morbidity were evaluated at follow-up. Patients in group 1 reported significant pain relief compared with those in group 2 immediately after the block (p < 0.05), but long-term results did not differ between the groups. Overall, the mean analgesic consumption was lower in group 1. They also found a decrease in drug-related adverse effects including constipation (5/12 in group 1 vs. 12/12 in group 2), nausea, and/or vomiting (4/12 in group 1 vs. 12/12 in group 2) (p < 0.05).
A prospective study of 50 consecutive pancreatic cancer patients [35] assessed the efficacy of neurolytic celiac plexus blocks depending on primary tumor location. Patients with pancreatic head cancer experienced more pain relief (92% relief) from neurolysis when compared to those with pancreatic body/tail cancer (29% relief). Study results are likely secondary to more advanced tumors in those with body and tail tumors; in which case, neurolysis was ineffective for pain control [36].
Eisenberg et al. [2] performed a meta-analysis of the efficacy and safety of neurolytic celiac plexus blocks from 24 papers including two or more patients with abdominal cancers (total of 1,145 patients included). Good to excellent pain relief was reported in 878/989 patients at 2 weeks. Ninety percent of patients had partial to complete pain relief at 3-month postneurolysis and 70–90% percent had relief until death, even if beyond 3 months after neurolysis.
Although literature has clearly shown that there is a significant reduction in pain scores for most patients following neurolytic celiac plexus blocks, there have also been studies to support that celiac plexus neurolysis may also alter opioid consumption, quality of life, and overall patient survival. Survival in patients with pre-procedure pain was significantly increased by up to 15 months in the celiac plexus neurolysis group versus the placebo group in one study (p = 0.0001) [5]. Data also suggested that there may be improved mood and lower levels of disability; however, this was not statistically significant [5].
A more recent study also supports a significant positive effect on duration of life and mood scores following neurolytic celiac block [37]. This study found a correlation between a reduction in pain and increase in longevity. Overall, neurolytic block, when compared to medical management alone, improved pain, elevated mood, reduced pain interference with activity, and was associated with an increase in life expectancy [37].
Despite the commonality of decreased pain scores throughout the literature, not all studies were able to reproduce the results found by Lillemoe et al. [5] and Staats et al. [37]. Multiple studies were unable to find statistically significant differences between medically managed patients and patients who underwent neurolysis, when evaluating quality of life [6, 34, 38]. However, the results from Kawamata et al. [38] indicate celiac plexus blockade does not directly improve quality of life in patients with pancreatic cancer pain, but it may prevent deterioration in quality of life by the long-lasting analgesic effect, limitation of side effects, and reduction of morphine consumption, compared to treatment only with NSAIDs and morphine.
Conflicting results regarding reduction in opioid consumption have been found throughout the literature. Kawamata et al. [38] found a delayed but significant reduction in opioid requirement 4–7 weeks after neurolysis and that consumption continued to decrease over time. Another study found that celiac plexus neurolysis caused a significant but not complete decrease in opioid consumption; patients experienced a mean reduction of 40–80 mg/day of oral morphine [4]. A multicenter, randomized, control trial of 65 patients [39] with pancreatic and upper abdominal cancer found no difference in pain relief or opioid consumption between patients who underwent medical management versus celiac plexus neurolysis or thoracic splanchnicectomy.
Mercadante et al. [40] published a randomized trial of 20 patients, two groups of 10 patients each who were followed until death; pain scores and side effects of their treatment were recorded. Both groups received 1 week of pharmacotherapy, after which group A continued with NSAID-opioid management that followed the World Health Organization stepwise approach and group B who received neurolytic plexus blocks. Although there was a reduction in visual analogue scale pain scores in both groups, there was no statistical significant difference between the two. However, there was a significant decrease in opioid consumption in the celiac plexus neurolysis group; some effects were seen up to 7 weeks after neurolysis or until death.
A recent meta-analysis published in 2011 by Arcidiacono et al. [41] identified six randomized control trials, published between 1993 and 2008, which compared the percutaneous posterior bilateral block (five studies) or the intraoperative block (one study) with standard analgesic therapy for pancreatic and upper abdominal cancer pain. The mean difference for the visual analogue scale pain score at 4 weeks was significant (p = 0.004) for the experimental group celiac plexus block. The improvement in pain control coincided with a reduction in opioid consumption; the mean difference in the use of analgesic therapy in the two groups was much greater in the celiac plexus block group (p < 0.00001) versus those managed with standard pharmacologic therapy. Decreased opioid usage persisted until the death of the patient, with significantly lower opioid requirements in the CPB group (p < 0.00001). Although opioids were never completely stopped, their reduction translated into fewer side effects such as constipation, which was significantly higher in the control group (p < 0.0001) [41].









