Chapter 14 Cerebral Venous Thrombosis
Cerebral venous thrombosis (CVT) was first described by Ribes in the early 19th century on the basis of postmortem examination.1 For a long time, CVT was seen as a rare and severe illness resulting in seizures, focal deficits, and often death. Its association with sinus infections was well described,2 but other predisposing conditions were not yet recognized. However, advances in vascular neuroimaging have led to a renewed appreciation of this disorder, which is more common, more variable, and less uniformly severe than previously assumed.3–6
Cerebral sinus venous thrombosis is estimated to account for 0.5% of all strokes in adults,3 but its true incidence is unknown, and frequent underrecognition is suspected.7 Initially asymptomatic venous sinus thrombosis has been implicated in the etiology of idiopathic intracranial hypertension.8,9 Indeed, studies have demonstrated that the most common symptom of CVT is headache (80%–90%) and the most common sign papilledema (50%–60%).10 Other clinical signs include focal deficits and partial seizures, and alteration of consciousness. Headache may be the only clinical symptom of CVT.11,12 Approximately one quarter of all patients have completely normal examination.3
Multiple causes and risk factors for CVT have been identified.5 The list comprises genetic and acquired prothrombotic conditions (the latter most prominently including pregnancy, puerperium, and combination of hormonal contraceptives and smoking), infections (particularly sinusitis, otitis, mastoiditis, and meningitis), systemic inflammatory illnesses (such as systemic lupus erythematosus, sarcoidosis, and inflammatory bowel disease), hematological disorders (e.g., polycythemia, leukemia, thrombocythemia, paroxysmal nocturnal hemoglobinuria), systemic cancer, severe dehydration, and head trauma. The threshold for obtaining brain imaging to exclude CVT should be lower in the presence of these conditions.
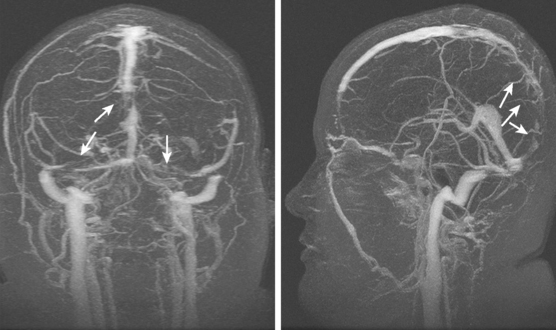
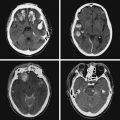
Current neuroimaging techniques have greatly enhanced our ability to diagnose CVT.3,13 Magnetic resonance imaging (MRI), particularly in combination with MR venography (MRV), provides excellent diagnostic yield in cases of thrombosis of dural sinus or deep cerebral veins (Figure 14-1).13,14 It is worth reemphasizing that noninvasive imaging modalities are allowing us to learn the broad spectrum of CVT. Although once the diagnosis was only suspected after severe intracranial hypertension or venous infarctions had occurred, today the possibility of CVT must be considered in the differential diagnosis of patients with new headaches and benign intracranial hypertension. Often CVT can be timely diagnosed only by keeping a low threshold for its clinical suspicion. A delayed or missed diagnosis of CVT, unfortunately still a common occurrence in practice, cannot be justified now that we have reliable and extremely safe means to reach the diagnosis.
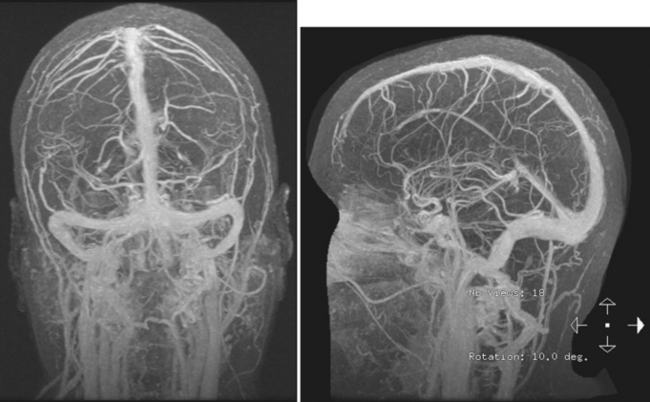
Figure 14-1 Example of normal gadolinium-enhanced magnetic resonance venography. Refer to Figure 14-3 for anatomical details.
Although MRI/MRV is the most proved and widely used set of tests for the identification of CVT, computed tomography (CT)/CT venogram (CTV) represent a valuable alternative when MRI is contraindicated or unavailable. The main disadvantage of CTV is the requirement for administration of iodinated contrast material.
On examination at the hospital, the patient was drowsy, had bilateral papilledema, right VI nerve palsy, and peripheral right facial nerve palsy. Otherwise the examination was unremarkable. She underwent MRI and MRV of the brain that demonstrated extensive thrombosis of the posterior two thirds of the superior sagittal sinus and the proximal transverse sinuses (Figure 14-2). Thrombophilia workup was negative.
ANATOMY OF THE VENOUS SYSTEM
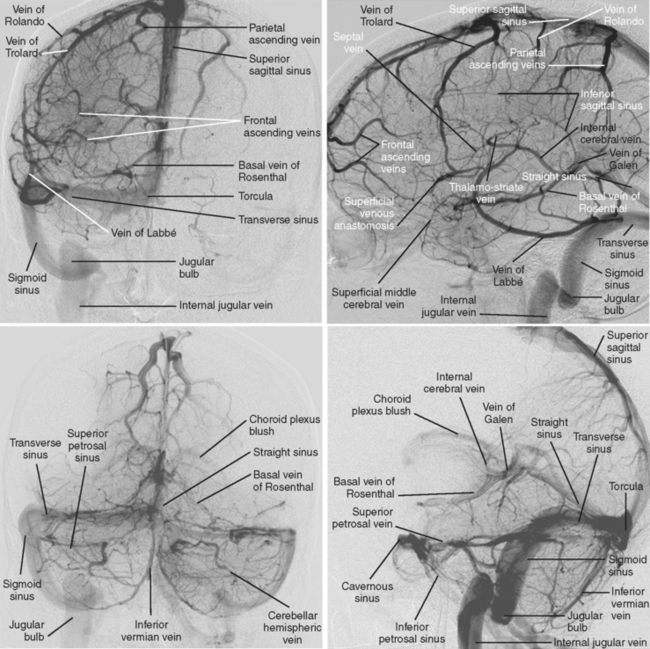
The cerebral venous system consists of dural venous sinuses, superficial veins, and deep veins. The dural venous sinuses are venous channels devoid of valves situated between the two layers of the dura, and thus they are not collapsible. They constitute the major draining pathways of the cerebral venous circulation. Cerebral veins are also devoid of valvular structures and have a very thin wall with no muscular tissue. They empty into the dural sinuses but may reverse their flow in cases of dural sinus occlusion. Venous anatomy is illustrated on angiographic pictures shown in Figure 14-3.
Dural Sinuses
The straight sinus is situated at the line of the junction of the falx cerebri with the tentorium cerebelli. After a descending course, it terminates at the internal occipital protuberance, usually emptying into the left transverse sinus. It receives venous blood flow from the great vein of Galen and superior cerebellar veins, thus participating in the deep venous drainage. Occlusion of this sinus usually produces venous infarcts in the deep basal ganglia.
The transverse sinuses are contained within the attachment of the tentorial leaves to the calvarium. At the posterior border of the petrous temporal bone, the transverse sinuses receive the superior petrosal sinus to become the sigmoid sinuses. Transverse sinuses receive blood from the superior sagittal sinus and straight sinus, as well as bridging veins from cerebellum, inferolateral surfaces of the temporal and occipital lobes, and tentorium. It also receives blood from the cortical vein of Labbé. In more than half of cases, the right transverse sinus is larger than the left.15,16 In up to 20% of the cases, a narrowed or atretic segment can be identified in at least one of the transverse sinuses.16
Deep Cerebral Veins
IMAGING CHARACTERISTICS OF CVT
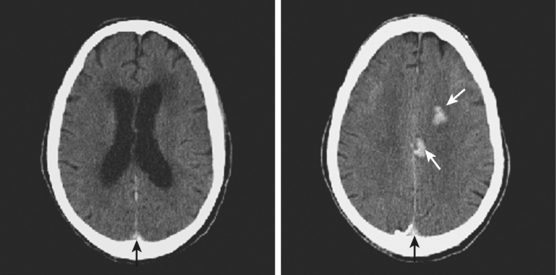
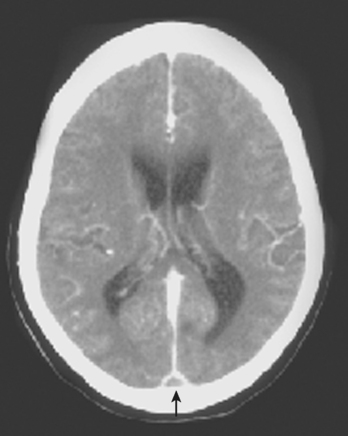
Computed Tomography
Signs of Parenchymal Involvement
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree