Chapter 6 Intracranial Atherosclerotic Disease
Narrowing of the large intracranial arteries is a surprisingly common cause of stroke in non-Caucasian populations, and one often overlooked in the evaluation of cerebrovascular patients. Various imaging modalities can effectively interrogate the intracranial vascular tree, at least the large intracranial vessels, to determine the extent of this condition. Although various pathologies can affect intracranial large arteries, including moyamoya disease, sickle cell disease, spasm, and arteritis, the most common cause is atherosclerosis. This chapter reviews the frequency of intracranial atherosclerotic disease, available diagnostic modalities, and treatment options.
EPIDEMIOLOGY AND NATURAL HISTORY
In the United States, between 8% and 10% of all strokes are deemed to be due to intracranial atherosclerotic disease.1,2 However, the burden of this condition has clear ethnic differences, affecting Asians, African Americans, and Latinos more than Caucasians. Some reports have cited that as many as 25% of all strokes in Asians are due to intracranial stenosis.3 In addition, intracranial disease may coexist with extracranial disease; 6% of patients with symptomatic extracranial carotid disease have tandem intracranial disease.4
The progression of severity of intracranial stenosis has not been carefully evaluated. Small studies have reported that between one third and one half of vessels develop worsening stenosis during a mean follow-up of 27 months.5,6 More important, progression of arterial narrowing strongly correlates with development of ischemic symptomatology.6 Therefore,
MECHANISMS OF CEREBRAL ISCHEMIA
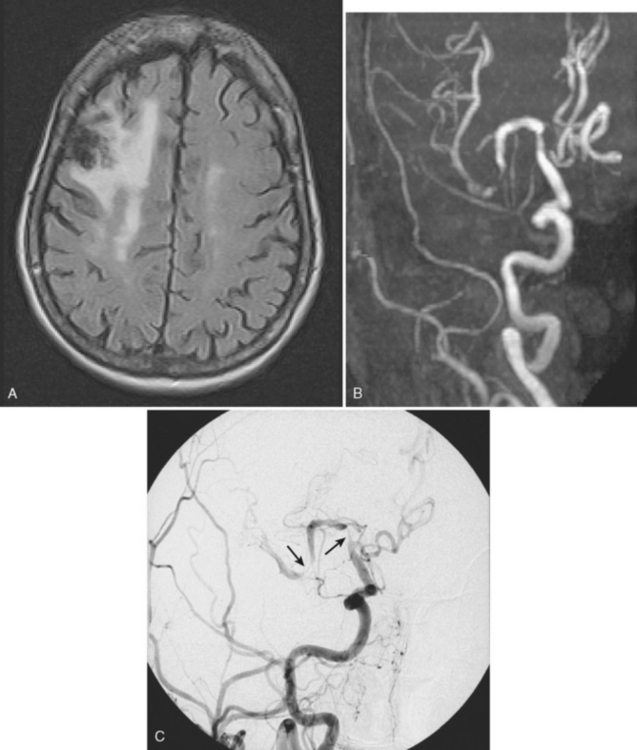
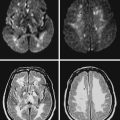
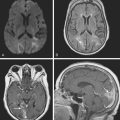
The mechanisms by which intracranial arterial disease causes cerebral ischemia are varied and include occlusion of the ostium of a penetrating artery producing a small subcortical (lacunar) stroke, occlusion of multiple penetrators resulting in a large subcortical infarct (such as a striatocapsular stroke), hemodynamic reduction in blood flow with a subsequent watershed stroke, and finally generation of a thrombus on the surface of the plaque with artery-to-artery embolism causing a cortical infarct. Figure 6-1 shows a cortical infarct in a patient with a middle cerebral artery stenosis. Indeed, in the extracranial-intracranial artery bypass surgery trial, 61% of those with middle cerebral artery stenosis had a cortical infarct.7 The role of artery-to-artery embolism in the production of strokes related to intracranial arterial disease has been confirmed by the finding of microembolic signals during transcranial Doppler (TCD) monitoring of the affected artery. Vessels with microembolic signals tend to be more stenotic and have an increased risk of becoming symptomatic.8
The mechanisms of infarction intracranial atherosclerosis are:
DIAGNOSIS OF INTRACRANIAL ATHEROSCLEROTIC DISEASE
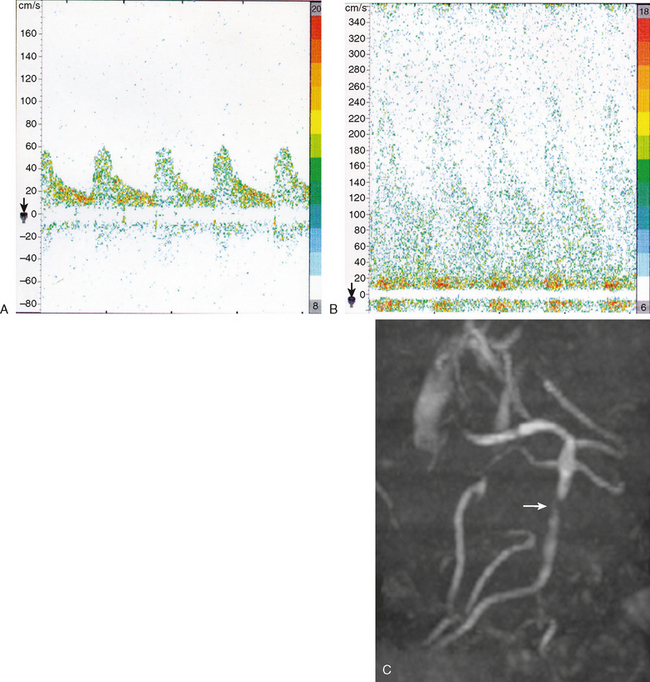
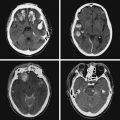
The gold standard method to detect intracranial arterial disease remains conventional catheter angiography. Nonetheless, this procedure is invasive, expensive, and has associated risks.9 Therefore, there is interest in determining the accuracy of available noninvasive tests. The recent Stroke Outcomes and Neuroimaging of Intracranial Atherosclerosis (SONIA) study evaluated the role of TCD and magnetic resonance angiography (MRA) in detecting 50% to 99% stenosis of the large intracranial arteries.10 Both TCD and MRA had strong negative predictive values of 86% and 91%, respectively, but the positive predictive values were lower at 36% and 59%. The TCD and MRA criteria for diagnosing 50% to 99% stenosis are outlined in Table 6-1. Data for sensitivity and specificity of computed tomography angiography (CTA) were unavailable from SONIA because of small numbers, but there is information indicating that it has good correlation with angiography, with one report showing a positive predictive value of 93%.11 Therefore, a normal TCD or MRA is a relatively trustworthy indication that there is no significant stenosis, but an abnormal result has a suboptimal predictive value. The relatively low positive predictive value for TCD may be understandable because it is a blind procedure in which the skill of the operator comes into play. The Doppler shift is greatest if the insonation is parallel to the plane of flow; perpendicular insonation will not detect this Doppler shift and therefore will be unable to detect flow velocity reliably. Figure 6-2 shows an intracranial carotid (cavernous segment) detected by MRA and confirmed by catheter angiography; TCD performed through the orbital window could not detect the increase in flow velocity in this case. However, straight arterial segments may be easier to interrogate by TCD, such as the vertebral, basilar, and M1 segments of the middle cerebral arteries. Figure 6-3 shows a significant basilar stenosis detected by a focal increase in flow velocity on TCD also noted on MRA.
TABLE 6-1 TCD and MRA cutoff parameters to detect ≥50% stenosis of large intracranial arteries.
| TCD (mean flow velocity) | |
|---|---|
| MCA | 100 cm/sec |
| ICA | 90 cm/sec |
| Vertebral | 80 cm/sec |
| Basilar | 80 cm/sec |
| MRA | |
|---|---|
| 50% stenosis or flow gap | |
MRA, magnetic resonance angiography; TCD, transcranial Doppler.
(Adapted from Feldmann E, Wilterdink JL, Kosinski A, Lynn M, Chimowitz MI, Sarafin J, et al., Neurology 2007; 68:2099–2106.)
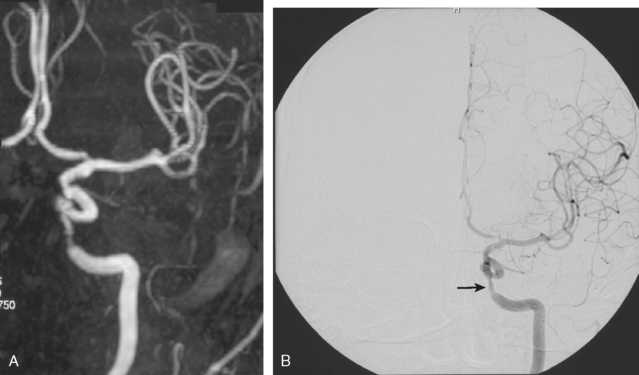
Figure 6-2 (A) A cavernous segment intracranial carotid stenosis confirmed by catheter angiography (B).
If a risky or invasive procedure is planned, then confirmatory conventional angiography is required. However, if medical treatment will not be significantly altered by the test results, it is reasonable to rely on noninvasive diagnostic modalities. As reviewed subsequently, current medical interventions are not optimal, and further research on the valve of revascularization will determine whether it is an effective and safe option; therefore, the relevance of the choice of diagnostic test will be amplified as more therapeutic choices become available.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree