Chapter 5 Extracranial Large Artery Atherothrombosis
Extracranial atherothrombotic disease is an important cause of stroke, and the management of asymptomatic occlusive disease poses additional challenges and opportunities for stroke prevention. Depending on the population studied, approximately 20% of strokes are attributed to large vessel extracranial disease.1 The prevalence of asymptomatic carotid stenosis greater than 50% stenosis is approximately 3% in the general population.2–4 There is a higher prevalence of extracranial atherosclerotic disease in whites compared with African Americans and other ethnic groups.5,6
ULTRASONOGRAPHY
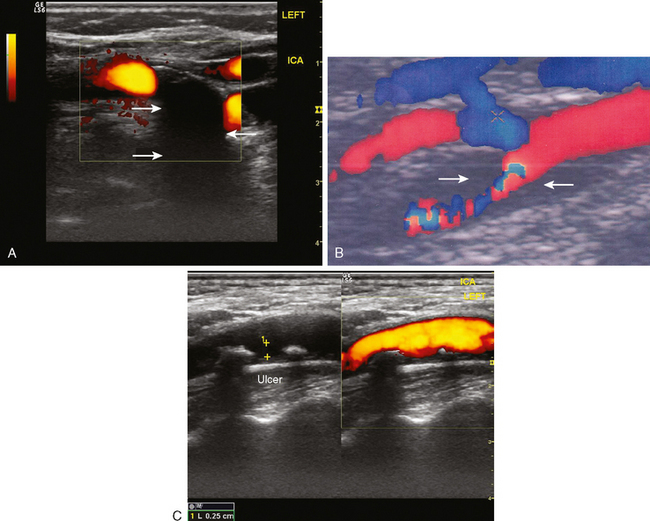
Determining the exact degree of stenosis remains the single most important goal of extracranial ultrasonography. However, plaque composition is an additional determinant of future stroke risk, particularly in the setting of symptomatic stenosis. Carotid plaques that are hypoechoic (i.e., have a dark intraplaque area), or ulcerated are of particular concern.7–11 These hypoechoic areas are likely to represent intraplaque hemorrhage, and these plaques should be considered unstable, thus having an increased thromboembolic potential. The presence of calcifications, in contrast, imparts relative plaque stability, and such plaques are less likely to be symptomatic12 (Figure 5-1).
Ultrasonography is technician-dependent and requires considerable skill and expertise. It is typically used as an initial screening tool, and thereby sensitivity is optimized at the expense of specificity-that is, it will tend to overestimate the degree of stenosis resulting in some false-positive results. Therefore a confirmatory test is necessary to improve the overall accuracy of the diagnostic approach.13 Ultrasound is less reliable in identifying carotid stenosis in moderate ranges (between 50% and 69%)14,15 and carotid occlusion.13
Because ultrasonography uses an increase in flow velocities as the main diagnostic criterion, the findings of ultrasonography in the setting of abnormal collateral flow patterns must be carefully interpreted. This situation often arises during insonation of a moderately stenotic plaque in patients with contralateral occlusion or high-grade stenosis. In these cases, ultrasound may overestimate the degree of stenosis of the moderately stenotic plaque,16,17 and the findings on ultrasonography must be cautiously reviewed and confirmed with other imaging modalities.
It is also important to realize that ultrasonography only visualizes the proximal portion of the carotid artery, and pathology involving the distal cervical segment may be unrecognized.
MR AND CT ANGIOGRAPHY
In general clinical practice, the findings on ultrasonography are often confirmed with an alternate imaging technique. MR and CT angiography have essentially replaced catheter angiography as the confirmatory test. The advantages MR and CT angiography are that they are noninvasive and readily available. The sensitivity and specificity for both techniques exceeds 80% to 90%.13,15,18,19 For the majority of patients, this approach (i.e., ultrasonography and CT/MR angiography combined) will correctly identify the true degree of stenosis. However, it continues to be controversial if noninvasive techniques are reliable enough to make decisions about surgical intervention, particularly if the degree of stenosis is in the moderate (50%–69%) range.15
CT angiography has recently experienced a revival with the advent of multislice detectors and development of sophisticated postimaging software. Advantages of CT over MR angiography lie in its acquisition speed. Even though few data are available with these newer techniques, they are likely to improve further the diagnostic accuracy of CT angiography.19
MR angiography is widely used at present but has some inherent limitations. There is a tendency for overestimation of the degree of stenosis because of sampling error. Therefore MR angiography may be more valuable as a screening tool rather than to confirm that stenosis is actually present.20 The specificity and sensitivity can be improved with gadolinium administration.20,21
Diagnostic accuracy of noninvasive imaging is generally improved if results of ultrasonography and MR or CT angiography are concordant.13
CATHETER CEREBRAL ANGIOGRAPHY
Catheter cerebral angiography remains the gold standard in determining the degree of stenosis and identifying surgical candidates. However, even in recent clinical trials, there has been a trend in favor of noninvasive testing, particularly in asymptomatic patients, given the risks of catheter angiography.22 The risk of stroke may be as high as 1.2% in asymptomatic patients; however, other reports have shown a reduced risk of serious complications in general practice.23,24
Less well recognized are subclinical infarcts detected by diffusion-weighted MR imaging after diagnostic cerebral angiography. Such lesions are present in up to 20% of patients and are the result of silent microembolism,25 but might produce subtle neuropsychiatric manifestations that go undetected.
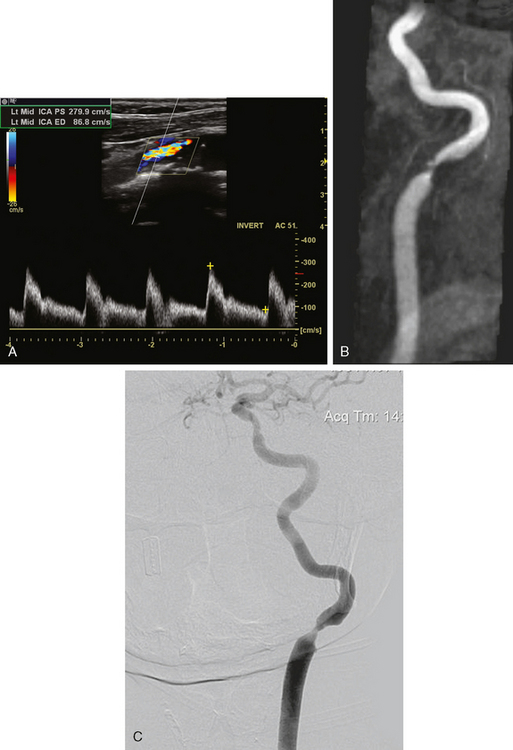
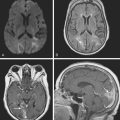
A 75-year-old hypertensive diabetic woman developed right-sided weakness. Extracranial ultrasonography showed a right ICA occlusion and left ICA high-grade stenosis meeting diagnostic criteria for stenosis exceeding 70% of the luminal diameter. MR angiography of the neck showed a high-grade left internal stenosis and confirmed the right internal carotid occlusion. On cerebral angiography, the left carotid stenosis was carefully measured to be 60% (Figure 5-2). The external carotid artery was occluded.
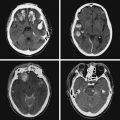
CLINICAL FEATURES OF CAROTID ATHEROTHROMBOSIS
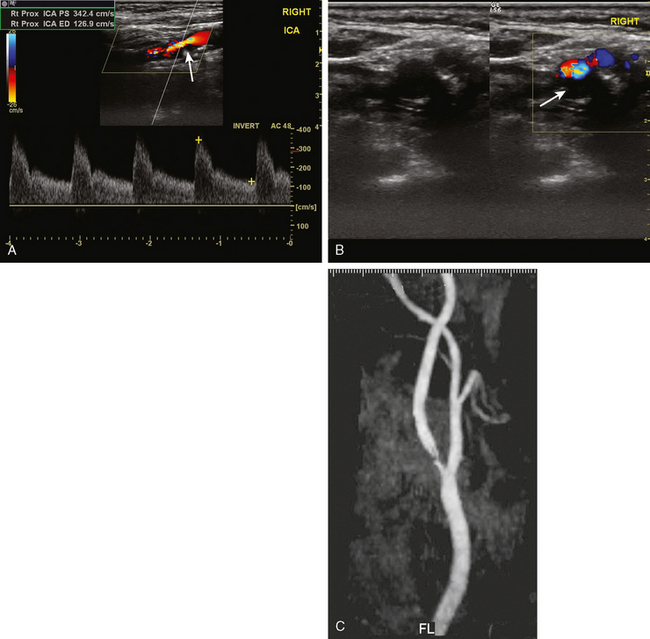
A 76-year-old man with a prior history of hypertension developed three episodes of sudden transient left hand and forearm numbness lasting 10 to 15 minutes over the previous week. His neurological examination showed no abnormalities. A harsh right carotid bruit was heard on neck auscultation. He underwent an emergent carotid ultrasound, which revealed a hypoechoic plaque at the right internal carotid origin causing high-grade stenosis of the lumen. MR angiography of the neck performed later confirmed these findings (Figure 5-3). He was admitted to a local hospital and placed on antithrombotic therapy. The following morning, he developed left-sided facial droop, dysarthria, and left-arm paralysis. He underwent an emergent endarterectomy and recovered without residual deficits.
This case illustrates the clinical hallmarks of large arterial atherothrombosis:
A 55-year-old smoker underwent a routine ocular examination and was found to have a Hollenhorst plaque in her right eye. She denied any visual symptoms. Carotid ultrasound revealed an ulcerated plaque at the origin of the right ICA causing no more than 30% to 40% stenosis (Figure 5-4). She was placed on aspirin, and her vascular risk factors were treated intensively.
MECHANISMS OF INFARCTION
Atherothrombotic Embolism
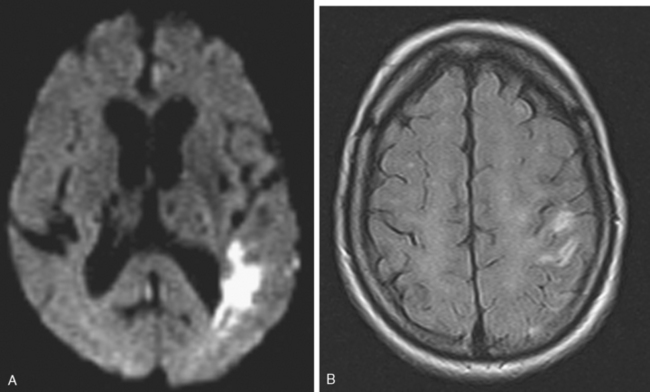
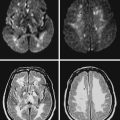
A 68 year-old man with history of hypertension, dyslipidemia, and diabetes developed sudden onset of left arm and leg numbness. On examination, he had diminished left-arm sensation and sensory extinction. Brain MRI showed an acute infarct in the right parietal lobe on diffusion-weighted imaging sequence. Fluid-attenuated inversion recovery (FLAIR) showed a prior infarct in right middle cerebral territory (Figure 5-5). Carotid ultrasound and MR angiography revealed high-grade stenosis of the right ICA artery at its origin.
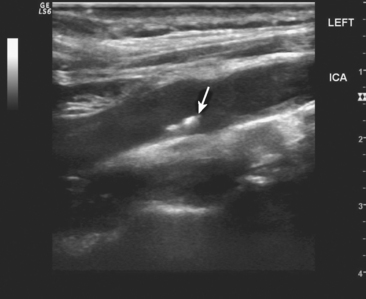
A carotid ultrasound showed plaque formation in the left carotid bulb, which produced no alteration of Doppler flow pattern and was estimated to cause no more than 50% stenosis of the luminal diameter (Figure 5-6). Subsequently, he underwent a catheter cerebral angiogram, which confirmed the presence of an ulcerated left carotid bulb plaque, causing no significant stenosis. Given the repetitive nature of his symptoms restricted to a single vascular distribution, it was felt that his symptoms were most likely explained by repeated thromboembolism from the proximal ICA plaque. Consequently, he was treated with left carotid endarterectomy. A hemorrhagic ulcerated plaque was found at the time of the operation. He recovered well from surgery and has been symptom-free for the following 2 years.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree