Chapter 34 Cervical Zygapophysial Joint Nerve (Medial Branch) Radiofrequency Neurotomy and Nerve Injection, Posterior Approach
Note: Please see page ii for a list of anatomical terms/abbreviations used in this book.
Cervical radiofrequency denervation (i.e., neurotomy) is typically performed after significant pain relief is documented with either an intraarticular facet joint injection and/or a medial branch block injection. The approach to the cervical radiofrequency ablation is posterior, whereas the approach to intraarticular facet joint and medial branch block injections can be posterior or lateral. In addition, contrast dye is typically unnecessary for radiofrequency denervation. The probe tip is placed so that the ablation occurs parallel to the nerve, with the tip of the needle lying over the medial branch nerve for maximum therapeutic effect. Because there is anatomic variation with regard to the course of the medial branch nerve, many practitioners perform two to four denervations at each level (please see Chapter 33, Figure 33–10). The needle’s active tip is repositioned so that each denervation pass is parallel and within a needle’s-width apart from one another.1,2 In this chapter, we describe an oblique pass. The recommended technique includes both a sagittal and oblique pass at each level by varying the obliquity and tilt except for C7, which only requires a sagittal pass.
With the approach described in this chapter, the needle is placed with the use of a trajectory view and advanced using multiplanar imaging, with an emphasis on safely using the lateral and foraminal oblique (Chapter 3) views to confirm depth. Before denervation, a 0.5 to 1 cc of anesthetic is typically placed. The time and duration of the denervation varies with different practitioners (e.g., two to four 90-second cycles at 80° to 85° C).2
 Trajectory View (Figure 34–1)
Trajectory View (Figure 34–1)
Confirm the level (with the anteroposterior view).
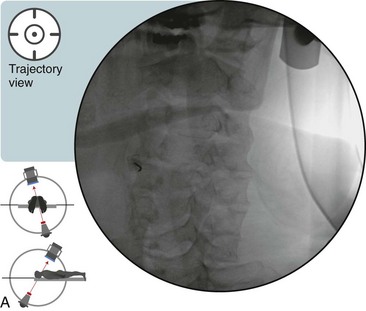
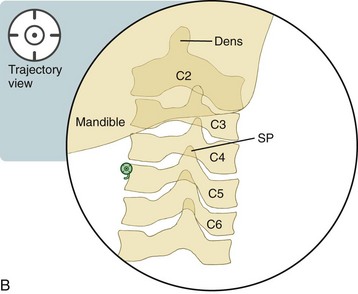
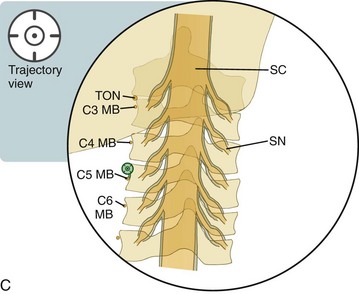
Figure 34–1 A, Fluoroscopic image of a trajectory view with the needle tip in position over the left C5 medial branch nerve. B, Radiopaque structures, trajectory view. C, Radiolucent structures, trajectory view. This figure illustrates a single location of the cervical medial branch nerve. See Figure 33–10 for the variable anatomical course of the cervical medial branch nerves.
 The needle-tip destination is the lateral groove or “waist” of the articular pillar (i.e., the lateral mass).
The needle-tip destination is the lateral groove or “waist” of the articular pillar (i.e., the lateral mass).
 There is variation with regard to the final needle position that is based on the level that is being treated.
There is variation with regard to the final needle position that is based on the level that is being treated.
 In this chapter, we describe an oblique pass. The recommended technique includes both a sagittal and oblique pass at each level by varying the obliquity and tilt except for C7, which only requires a sagittal pass.
In this chapter, we describe an oblique pass. The recommended technique includes both a sagittal and oblique pass at each level by varying the obliquity and tilt except for C7, which only requires a sagittal pass.
 The C5 medial branch lies within the middle segment of the lateral groove or “waist” of the articular pillar.
The C5 medial branch lies within the middle segment of the lateral groove or “waist” of the articular pillar.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





