Chapter 1 Gynecology and First Trimester Obstetrics
Adrian Dawkins and Nanditha George
1 Questions and Answers
Question 1.1: The Society of Radiologists in Ultrasound (SRU) Consensus Conference statement, published in Radiology in September 2010, addresses adnexal cysts in which group of women?
Symptomatic pregnant women.
Asymptomatic nonpregnant women.
Symptomatic premenopausal women.
Asymptomatic postmenopausal women.
Answer:
B. Correct. The SRU Consensus statement addressed lesions in asymptomatic nonpregnant women, both pre- and postmenopausal. While the recommendations may be useful in symptomatic women, the overall clinical picture should help steer management in these patients.
A, C, D—Incorrect. Asymptomatic nonpregnant women are addressed.
Question 1.2: What precise cyst measurement should be used to guide management of adnexal cysts according to the SRU Consensus statement (Radiology 2010)?
Maximum diameter in the sagittal plane.
Maximum diameter in the transverse plane.
Mean diameter.
Maximum diameter in any plane.
Answer:
D. Correct. The maximum diameter in any plane was chosen, since measurements in all three planes may be altered by pressure created by the endocavitary vaginal transducer.
A, B, C—Incorrect. The maximum diameter in any plane is used.
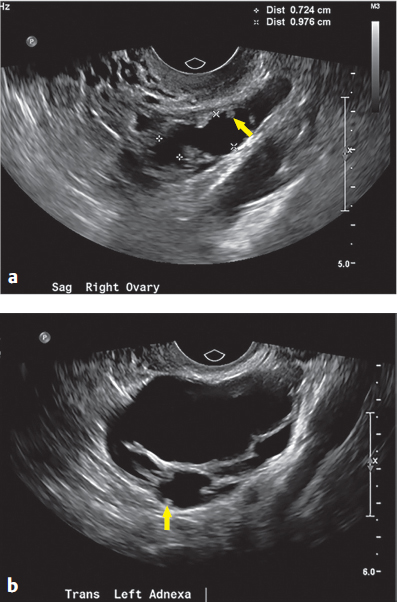
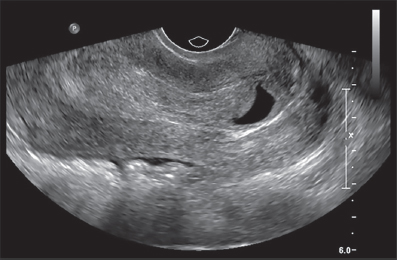
Question 1.3: These images were obtained in a 28-year-old female with abdominal pain. What is the likely cause for this appearance?
Endometriosis.
Ovarian hyperstimulation.
Molar pregnancy.
Ectopic pregnancy.
Answer:
A. Correct. The images demonstrate bilateral tubular fluid-filled structures within the adnexa. Also, tiny projections (arrows), due to longitudinal folds, can be seen protruding into the lumen. This has been described as the “cogwheel sign” and is typical of hydrosalpinx. Of the choices, endometriosis best explains the presence of bilateral hydrosalpinges.
B. Incorrect. Enlarged ovaries are seen in ovarian hyperstimulation.
C. Incorrect. Enlarged ovaries containing theca lutein cyst may be present in cases of molar pregnancy.
D. Incorrect. An ectopic pregnancy would not typically result in this appearance.
Question 1.4: A 54-year-old postmenopausal female undergoes a pelvic ultrasound due to an incidental left ovarian finding on computed tomography (CT). Which statement regarding management of this finding is correct?
No follow-up is required.
Follow-up in 1 year is recommended.
Pelvic magnetic resonance imaging (MRI) is recommended for better characterization.
None of the above.
Answer:
A. Correct. Recently published updated guidelines by the Society of Radiologists in Ultrasound (SRU) suggest that simple cysts in asymptomatic postmenopausal females require no follow-up if less than or equal to 3cm in size.
B. Incorrect. No follow-up is recommended.
C. Incorrect. Pelvic MRI may be of value for larger cysts if deemed to be not well-evaluated with ultrasound.
D. Incorrect. No follow-up is recommended.
Question 1.5: A 25-year-old woman presents with irregular menstrual bleeding and undergoes a pelvic ultrasound. A lesion is found within her right ovary. Which statement is correct?
The appearance is consistent with an endometrioma.
The appearance is consistent with a hemorrhagic cyst.
The appearance is consistent with a peritoneal inclusion cyst.
The appearance is consistent with a dermoid.
Answer:
D. Correct. The image demonstrates a complex cyst with an echogenic focus within the inferior aspect, toward the left of the image, consistent with fat. Short horizontal dash-like echogenic foci are also noted as well as tiny echogenic dots throughout the lesion. This had been described as the “dot-dash sign.” The findings are classic for an ovarian dermoid cyst.
A. Incorrect. An endometrioma is characterized by homogenous low-level echoes.
B. Incorrect. The typical hemorrhagic cyst demonstrates a mesh-like pattern.
C. Incorrect. A peritoneal inclusion cyst is fairly simple in morphology but conforms to the surrounding pelvic structures.
Question 1.6: Which statement best represents the appropriate management of the lesion seen in (Question 1.5)?
This lesion should be aspirated and sent for cytologic analysis.
A trial of danazol should be initiated.
No follow-up is required.
Repeat ultrasound in 6 months to 1 year.
Answer:
D. Correct. A dermoid should initially be re-evaluated with follow-up ultrasound in 6 months to 1 year to document stability. There is a very small risk (1%) of malignant transformation albeit in larger dermoids.
A. Incorrect. Aspiration of cystic ovarian lesions is generally avoided since the yield of useful diagnostic material is very low. There is also the risk of peritoneal seeding.
B. Incorrect. Danazol is a synthetic steroid, used to treat endometriosis.
C. Incorrect. A dermoid should initially be re-evaluated with follow-up ultrasound in 6 months to 1 year to document stability.
Question 1.7: Regarding early pregnancy, which statement is correct?
A nonviable pregnancy can be confirmed transabdominally if the crown–rump length measures at least 10 mm and no cardiac activity is detected.
A positive serum pregnancy test is defined as a beta human chorionic gonadotropin (HCG) value of 3 mIU/mL and above.
A pregnancy of unknown location is defined as one in which there is a positive serum or urine pregnancy test, with no discernible intrauterine gestational sac or sonographic evidence of an ectopic on a transvaginal scan.
A nonviable pregnancy is defined as one which has not yet reached 26 weeks gestation.
Answer:
C. Correct. A pregnancy of unknown location is defined as one in which there is a positive serum or urine pregnancy test, with no discernible intrauterine gestational sac or sonographic evidence of an ectopic on a transvaginal scan.
A. Incorrect. A nonviable pregnancy can be confirmed transabdominally if the crown–rump length measures at least 15 mm and no cardiac activity is detected.
B. Incorrect. A positive serum pregnancy test is defined as a beta HCG value of 5 mIU/mL and above.
D. Incorrect. A nonviable pregnancy is defined as one which has no chance of resulting in a liveborn child, for example, an ectopic pregnancy.
Question 1.8: A 32-year-old patient presents with sharp left-sided pelvic pain and a positive urine beta HCG. A pelvic ultrasound is performed. Given the sonographic findings and patient symptoms, what is the likelihood of an ectopic pregnancy?
1 in 30,000.
1 in 3,000.
1 in 300.
1 in 30.
Answer:
A. Correct. The image demonstrates the normal appearance of an early intrauterine pregnancy (IUP). The presence of an ectopic pregnancy in conjunction with an IUP, that is a heterotopic pregnancy, is very unlikely occurring in 1 in 30,000 pregnancies.
B, C, D—Incorrect. A heterotopic pregnancy occurs in 1 in 30,000 pregnancies.
Question 1.9: If the image in (Question 1.8) represents a normal early pregnancy, which structure should develop next?
Yolk sac.
Amnion.
Fetal pole.
Gestational sac.
Answer:
A. Correct. The yolk sac is the first structure to develop within the gestational sac in a normal pregnancy.
B. Incorrect. The yolk sac is visible before the amnion can be discerned.
C. Incorrect. The yolk sac is visible before the fetal pole can be discerned.
D. Incorrect. The gestational sac is the first sonographically detected structure to develop in a normal pregnancy.
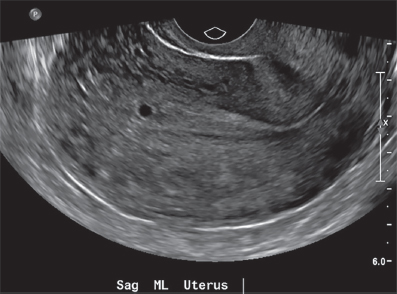
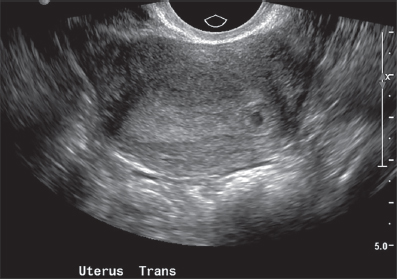
Question 1.10: Regarding this image, which statement is correct?
The pregnancy should be dated by the mean gestational sac diameter.
The pregnancy should be dated by the greatest gestational sac diameter.
The pregnancy should be dated by the mean yolk sac diameter.
The pregnancy should be dated by the greatest yolk sac diameter.
Answer:
A. Correct. At this point in the pregnancy, the mean diameter of the gestational sac is used to date the pregnancy.
B. Incorrect. The mean diameter of the gestational sac is used to date the pregnancy.
C, D—Incorrect. The size of the yolk sac is not used to date a pregnancy.
Question 1.11: Regarding the image in (Question 1.10), which statement is correct?
After 11 days, the absence of an embryo with cardiac activity is diagnostic of pregnancy failure.
If the mean sac diameter is 20 mm, the findings are diagnostic of pregnancy failure.
The yolk sac develops in the 7th week of pregnancy.
A yolk sac diameter of 7 mm is diagnostic of pregnancy failure.
Answer:
A. Correct. After 11 days, the absence of an embryo with cardiac activity is diagnostic of pregnancy failure.
B. Incorrect. A mean sac diameter of 25 mm, in the absence of an embryo is diagnostic of pregnancy failure.
C. Incorrect. The yolk sac develops at 5½ weeks.
D. Incorrect. A yolk sac diameter above 5 mm is highly suggestive of but not diagnostic of pregnancy failure.
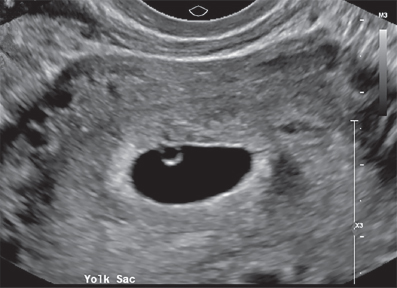
Question 1.12: Regarding this image, which statement is correct?

A multiple gestation pregnancy is not necessarily confirmed.
In general, a dichorionic diamniotic (DCDA) pregnancy is likely, however a monochorionic diamniotic (MCDA) pregnancy is excluded.
In general, a monochorionic monoamniotic (MCMA) pregnancy is excluded.
None of the above.
Answer:
C. Correct. The image demonstrates two yolk sacs within a gestational sac. This is consistent with a twin pregnancy. A twin pregnancy can be MCMA (2%), MCDA (30%), or DCDA (68%). In general, an MCMA twin pregnancy results from one fertilization event, typically leading to one yolk sac.
A. Incorrect. Two yolk sacs typically indicate a multiple gestation pregnancy, most commonly a twin pregnancy.
B. Incorrect. The image demonstrates two yolk sacs within a single gestational sac. The configuration is more typically seen in MCDA twins than DCDA twins. DCDA twins typically demonstrates two separate gestational sacs, each with its own yolk sac.
D. Incorrect. In general, a MCMA pregnancy is excluded since two yolk sacs are present.
Question 1.13: What structure is indicated by the arrow ?
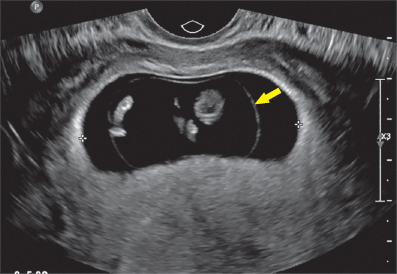
Amnion.
Chorion.
Yolk sac.
Gestational sac.
Answer:
A. Correct. Amnion. The arrow indicates the amniotic membrane.
B. Incorrect. The chorion is not indicated by the arrow.
C. Incorrect. The yolk sac is not indicated by the arrow.
D. Incorrect. The gestational sac is not indicated by the arrow.
Question 1.14: In a normal pregnancy, the amnion is usually no longer visible by the?
10th week of gestation.
14th week of gestation.
18th week of gestation.
22th week of gestation.
Answer:
B. Correct. The amnion usually fuses with the chorion by the 14th week after which it is no longer visible as a separate membrane. If seen as a separate membrane later than usual, chorioamniotic separation should be suspected, which could be a harbinger of complications.
A, C, D—Incorrect. The amnion is usually no longer visible by the 14th week.
Question 1.15: This 26-year-old female presents with a positive beta HCG and vaginal bleeding. Which statement is correct?
An inevitable abortion in underway.
Ectopic pregnancy is ruled out.
Molar pregnancy is reliably excluded.
Normal IUP is present.
Answer:
A. Correct. The image demonstrates a thickened endometrium with traces of fluid. Perhaps most importantly, the internal os is open and the endocervical canal is filled with soft-tissue material. This signifies a miscarriage in progress, the course of which cannot be altered.
B. Incorrect. An ectopic pregnancy should always be considered in the setting of a positive beta HCG and the absence of an IUP.
C. Incorrect. A molar pregnancy could present with a similar picture of endometrial thickening.
D. Incorrect. A normal IUP is not visualized.
Question 1.16: This patient presents with pelvic pain and a positive beta HCG. The location of the presumed gestational sac should prompt careful evaluation of which of the following?
The size of the ovaries.
The myometrial mantel.
The endometrial thickness.
The beta HCG.
Answer:
B. Correct. The gestational sac is located more eccentrically than usually encountered. This brings to bear the consideration of an interstitial ectopic. This describes an ectopic pregnancy that occurs in the interstitial portion of the fallopian tube. Careful evaluation of the surrounding myometrial mantle is recommended to aid in the diagnosis since a surrounding myometrial thickness of <5 mm is suggestive of the diagnosis.
A. Incorrect. The size of the ovaries will not aid in the sonographic diagnosis of an interstitial ectopic pregnancy.
C. Incorrect. This option will not aid in the sonographic diagnosis of an interstitial ectopic pregnancy.
D. Incorrect. Serial beta HCG levels may help to predict an abnormal early pregnancy, however it would not allow the specific diagnosis of an interstitial ectopic to be made.
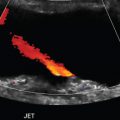
Question 1.17: A 27-year-old woman presents with a right adnexal pain. Regarding the presented image, which statement is correct?
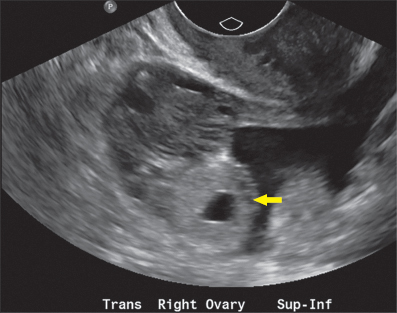
The arrow likely indicates a corpus luteal cyst.
If an ectopic is present, it is likely ovarian in location.
If the beta HCG is positive but doubles in value in 48 hours, an ectopic pregnancy is excluded.
None of the above.
Answer:
D. Correct. The arrow indicates an echogenic ring abutting, but separate from the ovary. These findings constitute the “tubal ring sign” and indicate a tubal ectopic pregnancy. Most tubal ectopic pregnancies occur within the ampullary portion of the tube.
A. Incorrect. A corpus luteal cyst is typically hypoechoic and is usually within the ovarian as opposed to abutting it.
B. Incorrect. Ectopic pregnancies very infrequently occur within the ovary. In particular, 3% of ectopic pregnancies are ovarian.
C. Incorrect. Approximately 20% of ectopic pregnancies may demonstrate doubling of beta HCG levels in 48 hours, mimicking an intrauterine pregnancy (IUP).
Question 1.18: A 41-year-old female presents with a positive pregnancy test and questionable spotting. A pelvic ultrasound is obtained. Based on the imaging below, which statement is correct?
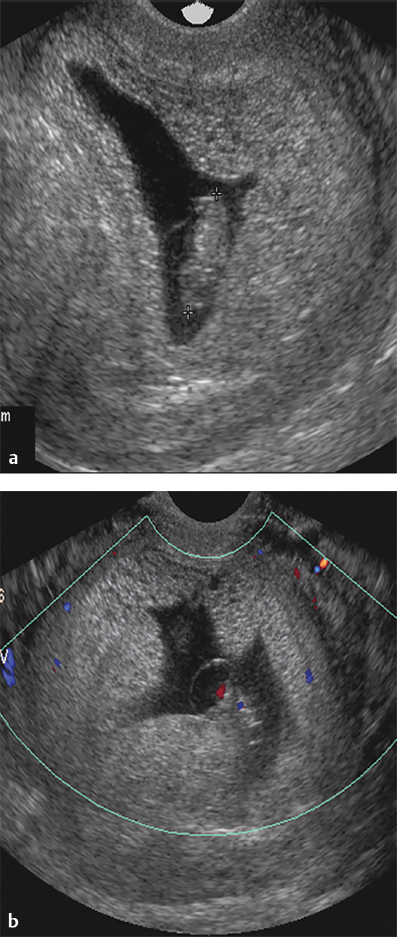
The appearance is within normal limits.
The patient probably suffers from hyperemesis.
A beta HCG level is likely lower than expected.
None of the above.
Answer:
B. Correct. The images demonstrate irregular thickening of the endometrium with numerous tiny cystic spaces. An irregular gestational sac is noted with a presumed fetal pole. The findings are suggestive of a molar pregnancy. Molar pregnancies occur in patients at extremes of age and are frequently associated with hyperemesis.
A. Incorrect. The appearance is very abnormal.
C. Incorrect. The beta HCG is often greater than expected for gestational age in molar pregnancies.
D. Incorrect. The findings are suggestive of a molar pregnancy. Molar pregnancies are frequently associated with hyperemesis.
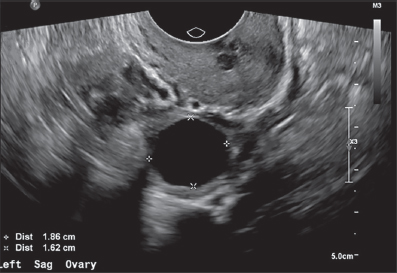
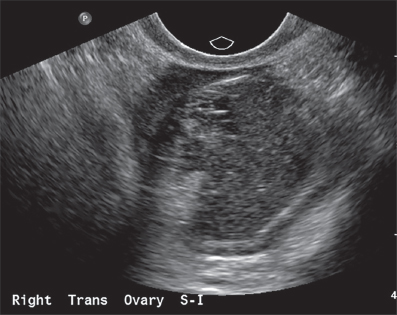
Question 1.19: The bilateral ovaries of the patient with a molar pregnancy are shown in the below images. Each measures roughly 8 cm in maximum length. What accounts for the appearance?
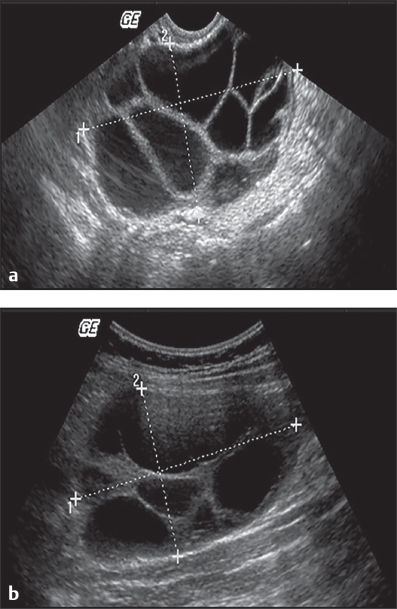
Bilateral ovarian neoplasms.
Theca lutein cysts.
Tubo-ovarian abscesses.
None of the above.
Answer:
B. Correct. Theca lutein cysts are usually noted in the enlarged ovaries of patients with molar pregnancy.
A. Incorrect. While synchronous bilateral ovarian neoplasms may occur, this option is not the most likely choice.
C. Incorrect. This option is not the most likely scenario. Tubo-ovarian abscesses usually present as complex cystic lesions with layering debris.
D. Incorrect. The findings are consistent with theca lutein cysts in the setting of a molar pregnancy.
Question 1.20: What karyotype is likely present? Refer to the images in question 1.18.
23x.
45xo.
46 xx.
69 xxy.
Answer:
D. Correct. The presence of a fetal pole within a molar pregnancy suggests a partial mole as opposed to a complete mole. A partial mole arises as a result of fertilization of one ovum by two spermatozoa. Consequently, this results in a triploid pregnancy. A complete mole is formed from the fertilization of an “empty ovum” by a haploid spermatozoon, followed by chromosomal duplication resulting in a diploid pregnancy.
A, B, C—Incorrect. A partial mole results in a triploid pregnancy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree