Chapter 7 Breast
Paul J. Spicer
7 Questions and Answers
Refer to the following case for questions 7.1 to 7.3.
Case 1 A 45-year-old female has a palpable mass in her right breast. Radial and antiradial ultrasound images are provided.
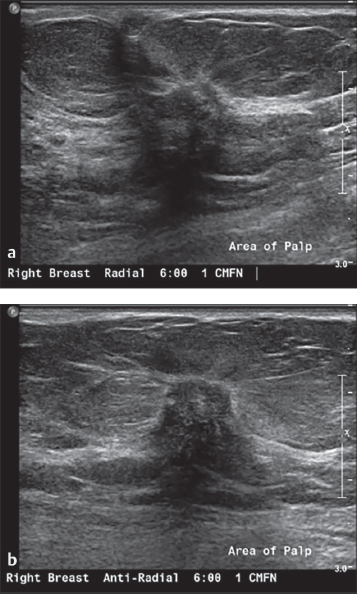
Question 7.1 Which of the following best describes the margin of the mass?
Irregular.
Indistinct.
Microlobulated.
Angular.
Spiculated.
Question 7.2: Which of the following best describes the shape of the mass?
Oval.
Round.
Irregular.
Microlobulated.
Angular.
Question 7.3: Which of the following features of a mass is most important for determining malignancy?
Shape.
Orientation.
Margin.
Echo pattern.
Posterior features.
Answer 7.1:
E. Correct. The margin of a mass is described as either circumscribed or not circumscribed. Circumscribed masses usually have an oval or round shape. Masses with margins which are not circumscribed have at least a portion of the margin which is not well-defined or sharply defined. These masses are further characterized as either indistinct, angular, microlobulated, or spiculated. The provided images depict a spiculated mass. Spiculated masses are those which have a margin with sharp lines radiating from the mass. This feature is often associated with malignancy. The spiculations are noted on both images as thin lines radiating from the mass.
A. Incorrect. Irregular is not an appropriate margin descriptor, instead it is a type of mass shape.
B. Incorrect. An indistinct margin is without a clear demarcation of at least a portion of the margin from the surrounding tissue. In the provided case, the margin is visible around the entirety of the mass.
C. Incorrect. An angular margin has sharp corners which often form acute angles. This is not present in the provided case.
D. Incorrect. A microlobulated margin has short cycle undulations, which is not present in the provided case.
Answer 7.2:
C. Correct. An irregular mass is a mass with a shape that cannot be described as either oval or round. This is typically a more worrisome finding for mass shape. The mass in the provided case is neither oval nor round.
A. Incorrect. Oval masses have a shape that is elliptical or egg-shaped. These masses may have two or three undulations. The mass in the provided case is not oval in shape.
B. Incorrect. Round masses have a spherical or circular shape where the anterior-posterior diameter equals the transverse diameter. This is an uncommon mass shape and does not reflect the mass in the provided case.
D. Incorrect. Microlobulated is a description of a mass margin, it is not a descriptor for a mass shape.
E. Incorrect. Angular is a description of a mass margin, it is not a descriptor for a mass shape.
Answer 7.3:
C. Correct. The margin of a mass is the most important feature for determining malignancy.
A. Incorrect. The shape of a mass is not the most important feature for determining malignancy.
B. Incorrect. Determining the benignity or malignancy of a mass based on orientation alone is discouraged.
D. Incorrect. The echo pattern of a mass alone has little predictive value for determining malignancy.
E. Incorrect. The posterior feature of a mass has more secondary value than primary predictive value for determining malignancy.
Refer to the following case for questions 7.4 to 7.6.
Case 2 A 50-year-old female has the following ultrasound images of a palpable mass in her left breast. She states the mass has not changed in size since she first noticed it several years prior.

Question 7.4: What is the most likely diagnosis?
Complicated cyst.
Complex cystic and solid mass.
Skin mass.
Silicone granuloma.
Invasive ductal carcinoma.
Question 7.5: What is the most appropriate Breast Imaging Reporting and Database System (BI-RADS) assessment?
2.
3.
4.
5.
6.
Question 7.6: What sonographic technique is applied in image (b) but not in (a)?
Spatial compounding.
Proper focal zone positioning.
Proper gray-scale gain.
Proper probe frequency.
Elastography.
Answer 7.4:
C. Correct. The mass is immediately below the skin surface and involves portions of the subcutaneous tissues, best noted by observing the edges of the mass. The mass is solid, without cystic components, and is oval in shape, parallel, with circumscribed margins. This is the appearance of a benign mass consistent with a large sebaceous cyst. A tract to the skin surface from the mass can be helpful for diagnosis as well, though not seen in this case.
A. Incorrect. The mass is solid, without any cystic components. A complicated cyst is a cyst that contains debris but does not have a solid component.
B. Incorrect. The mass is solid, without any cystic components. A complex cystic and solid mass has both cystic and solid components.
D. Incorrect. A silicone granuloma typically has the classic snowstorm shadowing created by the silicone. No shadowing is noted deep to this mass. Instead it has enhancement, meaning the area deep to the mass is more echogenic than the other tissue in the image at a comparable depth.
E. Incorrect. No suspicious features are noted with this mass to suggest malignancy.
Answer 7.5:
A. Correct. Skin masses are benign, therefore a BI-RADS 2 assessment is appropriate.
B. Incorrect. BI-RADS 3 assessments are for findings that have a less than or equal to 2% chance of malignancy. Since skin lesions are benign, this would be an inappropriate BI-RADS designation for this mass.
C. Incorrect. BI-RADS 4 assessments are for findings with a greater than 2% but less than 95% chance of malignancy. No suspicious features are noted and biopsy is not warranted. This is an inappropriate BI-RADS designation for this mass.
D. Incorrect. BI-RADS 5 assessments are for findings with a 95% or greater chance of malignancy. The mass in this case is benign, therefore this would be an incorrect designation.
E. Incorrect. BI-RADS 6 assessments are for biopsy-proven malignancies. This mass is benign in appearance and has not been biopsied, therefore this would be an incorrect designation.
Answer 7.6:
A. Correct. Spatial compounding is a technique used to improve resolution in the center of the image. This allows the margins of lesions to be visualized more clearly but the posterior features are less apparent. This is created by summing several overlapping ultrasound images obtained at different angles of insonation into a single image.
B. Incorrect. The focal zones are appropriately positioned in each image.
C. Incorrect. The gray-scale gain is appropriately set in both images. The gray-scale gain is set so that the normal breast parenchyma utilizes much of the gray-scale range.
D. Incorrect. The same probe frequency is utilized in both images.
E. Incorrect. Elastography was not utilized in either image. If strain elastography was utilized a color box would encompass the relevant finding, documenting the stiffness of the finding relative to normal tissue, and a corresponding scale would be noted in the upper-right-hand corner of the image.
Refer to the following case for questions 7.7 to 7.9.
Case 3 A 14-year-old female has a palpable abnormality in her right breast. Radial and antiradial ultrasound images are provided.

Question 7.7: What is the most likely diagnosis?
Simple cyst.
Clustered microcysts.
Complicated cyst.
Complex cystic and solid mass.
Lymph node.
Question 7.8: What is the posterior feature of this mass?
No posterior feature.
Twinkling.
Enhancement.
Shadowing.
Combined pattern.
Question 7.9: What type of probe does the American College of Radiology recommend for breast imaging?
Linear array, at least 10 MHz.
Curvilinear array, at least 10 MHz.
Linear array, at least 5 MHz.
Curvilinear array, at least 5 MHz.
Hockey stick probe.
Answer 7.7:
C. Correct. Complicated cysts are cysts which contain internal debris, as in this case. They do not have a solid component and have an imperceptible wall.
A. Incorrect. A simple cyst is a cyst that is circumscribed, round or oval, anechoic, and has posterior enhancement.
B. Incorrect. Clustered microcysts are a cluster of anechoic masses, each of which is less than 2 or 3 mm. They have intervening septations which are less than 0.5 mm in thickness. They do not have a solid component.
D. Incorrect. Complex cystic and solid masses have both anechoic cysts, or fluid, and echogenic solid components.
E. Incorrect. Lymph nodes typically have an echogenic fatty hilum and an outer cortex. They are reniform in shape.
Answer 7.8:
C. Correct. Enhancement occurs when the sound transmission is unimpeded as it passes through the mass, causing the area deep to the mass to be more echogenic than the adjacent tissue at the same depth. This is the posterior feature noted in this case. This is often seen with cysts, but some cancers also demonstrate this same pattern of posterior enhancement.
A. Incorrect. Masses with no posterior features are those in which the area deep to the mass is the same as the adjacent tissue at the same depth.
B. Incorrect. Twinkling is not a descriptive term used in breast imaging as defined by the BI-RADS atlas. This term is usually applied to renal calcifications.
D. Incorrect. Shadowing is noted when the area deep to the mass is attenuated relative to the adjacent tissue at the same depth. This can be seen in benign entities such as fibrosis, scar, fibrous mastopathy, and calcifications but it can also be seen in some cancers.
E. Incorrect. A combined pattern means the mass has more than one posterior feature.
Answer 7.9:
A. Correct. The American College of Radiology recommends the use of a broad bandwidth linear array transducer with a center frequency of at least 10 MHz.
B. Incorrect. Curvilinear probes are not typically used in breast imaging.
C. Incorrect. Frequencies of at least 10 MHz probes are preferred in breast imaging.
D. Incorrect. Curvilinear probes are not typically used in breast imaging.
E. Incorrect. Hockey stick probes are not typically used in breast imaging. These are more commonly used in areas where a smaller probe footprint is necessary such as in certain musculoskeletal situations.
Refer to the following case for questions 7.10 to 7.12.
Case 4 A 20-year-old female has a palpable mass in her right breast. Radial and antiradial ultrasound images are provided.

Question 7.10: What is the most likely diagnosis?
Simple cyst.
Complex cystic and solid mass.
Lymph node.
Fibroadenoma.
Epidermal inclusion cyst.
Question 7.11: What is the most appropriate BI-RADS assessment?
2.
3.
4.
5.
6.
Question 7.12: How can it be determined if the depth of the provided image is appropriate?
The entirety of the target should be visualized.
The pectoralis muscle should be visualized.
The ribs should be visualized.
The pleura should be visualized.
The lung should be visualized.
Answer 7.10:
D. Correct. The images depict a solid mass with circumscribed margins, oval shape, hypoechoic to fat, minimal posterior enhancement, and parallel orientation. This is consistent with a fibroadenoma.
A. Incorrect. A simple cyst is a cyst that is circumscribed, round or oval, anechoic, and has posterior enhancement. The mass in this case is solid instead of cystic.
B. Incorrect. Complex cystic and solid masses have both anechoic cysts, or fluid, and echogenic solid components. No cystic components are noted in this case.
C. Incorrect. Lymph nodes typically have an echogenic fatty hilum and an outer cortex. They are reniform in shape. The mass in this case is not reniform in shape and an echogenic hilum is not visualized.
E. Incorrect. An epidermal inclusion cyst is a skin lesion. The mass in this case is within the breast parenchyma, not within the skin.
Answer 7.11:
B. Correct. In patients under 40 years of age, fibro-adenomas with typical imaging features are given a BI-RADS 3 assessment.
A. Incorrect. A fibroadenoma can be given a BI-RADS 2 assessment if there are at least three total similar masses between both breasts, at least two in one breast, and at least one in the contralateral breast, or if the fibroadenoma has previously gone through a 2-year follow-up BI-RADS 3 cycle. Neither of these scenarios were noted in this case.
C, D—Incorrect. Masses in women under 40 years of age with typical imaging features of a fibroadenoma do not require biopsy.
E. Incorrect. This mass has not previously been biopsied, therefore it is not a biopsy-proven malignancy.
Answer 7.12:
B. Correct. The appropriate depth of an image is defined as including the breast tissue and the pectoralis muscle deep to it. By using this technique, it ensures that the entirety of the depth of the breast tissue is included in the image so that no breast lesions will be missed.
A. Incorrect. It is true that the entirety of the lesion should be visualized; however tissue deep to the lesion should also be visualized as well.
C. Incorrect. The ribs are deeper than what is required and therefore should not be included in the image.
D. Incorrect. The pleura is deeper than what is required and therefore should not be included in the image.
E. Incorrect. The lung is deeper than what is required and therefore should not be included in the image.
Refer to the following case for questions 7.13 to 7.15.
Case 5 A 54-year-old female has a palpable abnormality in her right breast. Radial and antiradial ultrasound images are provided.

Question 7.13: What is the most likely diagnosis?
Complicated cyst.
Fibroadenoma.
Intramammary node.
Abscess.
Invasive ductal carcinoma.
Question 7.14: Which of the following additional findings is present in the ultrasound images?
Skin thickening.
Skin retraction.
Intraductal extension.
Ductal debris.
Vascularity.
Question 7.15: What skin thickness is characterized as skin thickening?
>1 mm.
>2 mm.
>3 mm.
>4 mm.
>5 mm.
Answer 7.13:
E. Correct. The mass is irregular in shape with microlobulated margins and adjacent architectural distortion of the Cooper ligaments. The features of the mass are worrisome for malignancy and biopsy is warranted. The biopsy results yielded an invasive ductal carcinoma.
A. Incorrect. The mass is solid, not cystic. Therefore, this is not a complicated cyst.
B. Incorrect. The mass has worrisome features and is inconsistent with a fibroadenoma.
C. Incorrect. The mass does not have the typical reniform shape as present in intramammary lymph nodes. Also, no fatty hilum is noted.
D. Incorrect. The mass is solid without cystic or fluid-filled areas, therefore this is not an abscess.
Answer 7.14:
A. Correct. Skin thickening is noted in the images. Skin thickening is defined as skin >2 mm in thickness. This is a case of inflammatory breast cancer resulting from an invasive ductal carcinoma with overlying skin thickening.
B. Incorrect. Skin retraction is noted when the surface of the skin is concave or ill-defined and is pulled in. Skin retraction is not present in this case.
C. Incorrect. Masses may have intraductal extension, where the mass extends into an adjacent duct. This often dilates the duct. Ductal extension is not present on the provided images.
D. Incorrect. Debris within a duct is typically a benign finding. Ducts are not visualized in the provided images, therefore ductal debris is not present in this case.
E. Incorrect. Vascularity is not detected in the provided images as color images were not included.
Answer 7.15
B. Correct. Skin thickening is defined as skin >2 mm in thickness. This may be diffuse or focal. The exception is in the inframammary fold or the periareolar region, where it may normally be up to 4 mm in thickness. Skin thickening may be seen in cellulitis, mastitis, or inflammatory breast cancer.
A. Incorrect. More than 1 mm is within the normal limits for skin thickness. Skin thickening is defined as skin >2 mm in thickness.
C, D, E—Incorrect. Skin thickening is defined as skin >2 mm in thickness.
Refer to the following case for questions 7.16 to 7.18.
Case 6 A patient with inflammatory breast cancer undergoes an ipsilateral axillary ultrasound. A single ultrasound image of one of the axillary lymph nodes is provided.

Question 7.16 Based on the ultrasound image, what is the next most appropriate step?
Nothing, the lymph node is normal.
Compare with the contralateral side with ultrasound to determine if the node is normal.
Compare with the mammogram to determine if the node is normal.
Recommend magnetic resonance imaging (MRI) to determine if the node is normal.
Recommend sampling of the node under ultrasound guidance.
Question 7.17 What cortical thickness is considered abnormal?
>1 mm.
>2 mm.
>3 mm.
>4 mm.
>5 mm.
Question 7.18: Which feature of an abnormal node has the highest positive predictive value for metastatic disease within an axillary lymph node?
Hilar blood flow.
Nonhilar blood flow.
Cortical thickening.
Calcifications in the node.
Loss of the fatty hilum.
Answer 7.16:
E. Correct. This lymph node is markedly abnormal. It has cortical thickening >3 mm with complete loss of the fatty hilum. This node should, therefore, be sampled under ultrasound guidance. This can be performed with fine needle aspiration (FNA) if cytopathology is available on site to analyze the specimen in real time to determine its adequacy. Otherwise, ultrasound-guided core biopsy could be performed.
A. Incorrect. The node is markedly abnormal in this case.
B. Incorrect. Comparing with the contralateral side is not necessary in this case as the node in question is markedly abnormal. Side-to-side comparison is sometimes helpful if there is suspicion of an inflammatory node resulting from a systemic disease.
C. Incorrect. Ultrasound is more sensitive and specific than mammography for evaluation of axillary lymph nodes.
D. Incorrect. Ultrasound is more sensitive and specific than MRI for evaluation of axillary lymph nodes. This node is obviously abnormal as per the ultrasound, therefore MRI would not add any value for evaluation of this node.
Answer 7.17:
C. Correct. A cortical thickness >3 mm is considered abnormal.
A, B, D, E—Incorrect. A cortical thickness >3 mm is considered abnormal.
Answer 7.18:
E. Correct. Loss of the fatty hilum has been reported to have a 100% positive predictive value for metastatic involvement of the lymph node.
A. Incorrect. Hilar blood flow describes the normal flow of blood to the lymph node through the hilum.
B. Incorrect. Nonhilar blood flow refers to flow of blood directly into the cortex of the node resulting from neovascularity, thus bypassing the normal flow through the hilum. This has a high positive predictive value for metastatic involvement, but it is less than 100%.
C. Incorrect. Cortical thickening is a suspicious finding, but it has a positive predictive value of less than 100%. It has a sensitivity of 88% and a specificity of 75%.
D. Incorrect. Calcifications in the lymph node may be a suspicious finding, particularly if the shape of the calcifications is suspicious. However, calcifications can also occur within lymph nodes from benign causes, such as the presence of tattoos in an area which drain to the axillary nodes.
Refer to the following case for 7.19 to 7.21.
Case 7 A 32-year-old female has spontaneous right bloody nipple discharge. Split screen image, including power Doppler, is provided.

Question 7.19: The mass does not move with changing the positioning of the patient. What is the most likely diagnosis?
Debris.
Fibroadenoma.
Papilloma.
Invasive ductal carcinoma.
Invasive lobular carcinoma.
Question 7.20: What BI-RADS assessment is appropriate based on the ultrasound image and history?
3.
4A.
4B.
4C.
5.
Question 7.21: Which feature of discharge is most worrisome?
Bilateral, milky color.
Unilateral, green color.
Unilateral, milky color.
Bilateral, green color.
Unilateral, bloody color.
Answer 7.19:
C. Correct. The image depicts a solid mass with internal flow inside the duct. As per the history, this does not move with movement of the patient, therefore debris is unlikely. Debris also does not have an internal flow. The most common solid intraductal mass is a papilloma.
A. Incorrect. The finding is a solid mass with internal flow; therefore it is not likely to be debris. Debris does not have internal flow and it may move with changes in patient positioning, similar to sludge in the gallbladder. A technique called ballottement can also be used to differentiate debris from a solid mass. When pressure from the probe is applied to the area of concern, debris will disperse away from the pressure with ballottement while a solid mass will not.
B. Incorrect. The image does not have the typical features of a fibroadenoma.
D. Incorrect. The most common solid intraductal mass is a papilloma, not invasive ductal carcinoma.
E. Incorrect. The most common solid intraductal mass is a papilloma, not invasive lobular carcinoma.
Answer 7.20:
B. Correct. The correct BI-RADS assessment for the history and ultrasound image is 4A. Spontaneous bloody nipple discharge with an intraductal mass noted by ultrasound has a positive predictive value of malignancy of 8%. 4A findings have >2% but <10% chance of malignancy.
A. Incorrect. BI-RADS 3 findings have a less than 2% chance of malignancy. This finding, however, has an 8% chance of malignancy and is, therefore, a 4A finding.
C. Incorrect. BI-RADS 4B findings have a ≥10% but <50% chance of malignancy. This finding, however, only has an 8% chance of malignancy and is, therefore, a 4A finding.
D. Incorrect. BI-RADS 4C findings have a ≥50% but <95% chance of malignancy. This finding, however, only has an 8% chance of malignancy and is, therefore, a 4A finding.
E. Incorrect. BI-RADS 5 findings have a ≥95% chance of malignancy. This finding, however, only has an 8% chance of malignancy and is, therefore, a 4A finding.
Answer 7.21:
E. Correct. Worrisome features of malignancy include a discharge that is clear or bloody in color, unilateral, spontaneous, and via a single duct. Features that are less concerning include a discharge that is milky or yellow in color, bilateral, nonspontaneous, and via multiple ducts. The worrisome features collectively point to concern for a mass within a single ductal system within a breast which may be bleeding or generating clear fluid.
A. Incorrect. Both bilaterality and milky color are not typically worrisome findings.
B. Incorrect. Green color is not typically a worrisome finding.
C. Incorrect. Milky color is not typically a worrisome finding.
D. Incorrect. Both bilaterality and green color are not typically worrisome findings.
Refer to the following case for 7.22 to 7.24.
Case 8 A 55-year-old male has left breast tenderness and a palpable abnormality. Transverse and long axis ultrasound images are provided.

Question 7.22: What is the most likely diagnosis?
Gynecomastia.
Papilloma.
Fibroadenoma.
Ductal carcinoma in situ.
Invasive lobular carcinoma.
Question 7.23: What is the most appropriate BI-RADS assessment?
2.
3.
4.
5.
6.
Question 7.24: A 40-year-old female has a mammogram and ultrasound depicting an abnormal axillary node which has previously been proven to represent lymphoma by biopsy. No other suspicious findings are noted. With this information, what is the appropriate BI-RADS assessment for the imaging findings in this case?
2.
3.
4.
5.
6.
Answer 7.22:
A. Correct. The images depict gynecomastia in a male patient. No focal mass or suspicious abnormality is noted. Gynecomastia has the typical appearance of female breast tissue with ducts and stroma; however, no lobules are typically present. The ultrasound in this case has the usual depiction of stroma and ducts in the subareolar region of the breast.
B. Incorrect. No intraductal mass is noted.
C. Incorrect. No solid mass is noted. Males do not typically have lobules therefore they do not have masses that start in the lobule, such as a fibroadenoma.
D. Incorrect. No solid mass or intraductal mass is noted.
E. Incorrect. No solid mass is noted. Males do not typically have lobules therefore they do not have masses that start in the lobule, such as invasive lobular carcinoma.
Answer 7.23:
A. Correct. Gynecomastia is benign, therefore a BI-RADS 2 assessment is appropriate.
B. Incorrect. Gynecomastia is benign, therefore a BI-RADS 2 assessment is appropriate. BI-RADS 3 is for a finding which is probably benign but still has <2% chance of malignancy.
C. Incorrect. Gynecomastia is benign, therefore a BI-RADS 2 assessment is appropriate. BI-RADS 4 is for a finding which is suspicious.
D. Incorrect. Gynecomastia is benign, therefore a BI-RADS 2 assessment is appropriate. BI-RADS 5 is for a finding which is highly suggestive of malignancy.
E. Incorrect. Gynecomastia is benign, therefore a BI-RADS 2 assessment is appropriate. BI-RADS 6 is for a biopsy-proven malignancy.
Answer 7.24:
A. Correct. Though the patient has a malignancy, the malignancy is not breast related. The BI-RADS assessment only applies to breast cancer, therefore the patient in this case is given a BI-RADS 2 assessment for the breast findings instead of a BI-RADS 6 for biopsy-proven lymphoma.
B. Incorrect. The findings are benign, therefore follow-up as a BI-RADS 3 assessment if inappropriate.
C. Incorrect. The findings are benign, no breast finding is noted which requires biopsy under a BI-RADS 4 assessment.
D. Incorrect. The findings are benign, no breast findings are noted which requires a biopsy under a BI-RADS 5 assessment.
E. Incorrect. The patient does have lymphoma; however, it is not breast related therefore it is not considered in the BI-RADS assessment. The breast findings are benign, therefore a BI-RADS 2 assessment is given. It would be appropriate to add a sentence in the recommendations noting the presence of the abnormal node and that it is consistent with the known history of lymphoma.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree