2St George’s, University of London, London, UK
- Plain radiographs remain the mainstay of imaging
- It is important to understand the basic technical concepts underpinning CXRs and thoracic CT to appreciate their benefits and limitations
- A systematic approach is crucial to evaluating the imaging appearances of various traumatic and non-traumatic conditions of the chest
The chest radiograph (CXR) remains the initial method of assessing the thorax in most patients presenting to the emergency department. At the same time, limitations of the CXR may mean that further imaging with other modalities, usually computed tomography (CT) is needed. This chapter provides a basis for understanding the normal appearances of the thorax on imaging, a structured evaluation approach, and descriptions of the common traumatic and non-traumatic conditions relevant to the emergency department.
Imaging techniques
Chest radiograph (CXR)
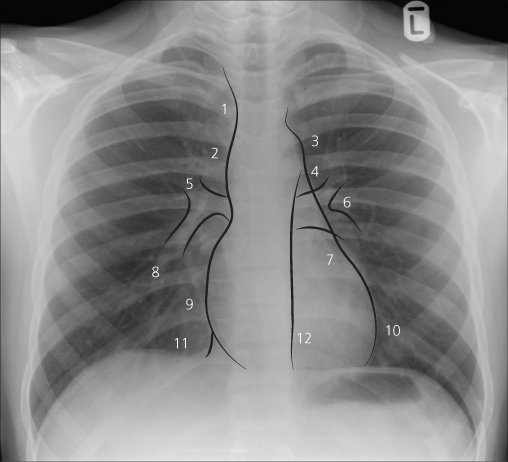
The posteroanterior (PA) view is the best CXR technique, taken with the patient in an erect position, facing the film, and with the X-ray tube behind the patient. The lungs are clearly viewed due to the full inspiration and the projection of scapulae outside the lungs (Figure 12.1).
Figure 12.1 Normal PA CXR, with some of the mediastinal and hilar structures outlined. Note the position of the scapulae, which do not overlap the lungs. 1, right brachiocephalic vein; 2, superior vena cava; 3, aortic arch; 4, main pulmonary artery; 5, right upper lobe pulmonary artery; 6, left pulmonary artery; 7, Left atrial appendage; 8, right lower lobe pulmonary artery; 9, right atrium; 10, left ventricle; 11, inferior vena cava; 12, descending thoracic aorta.
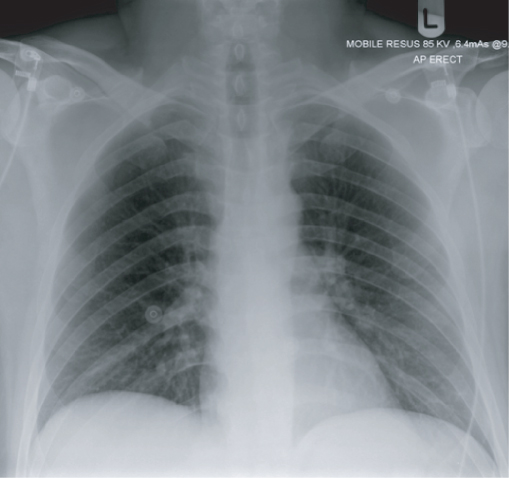
However, the anteroposterior (AP) view is the most commonly performed view in the emergency department, as patients often cannot be positioned erect or require a portable film (Figure 12.2).
Figure 12.2 Normal AP CXR. The scapulae partially overlap the lungs.
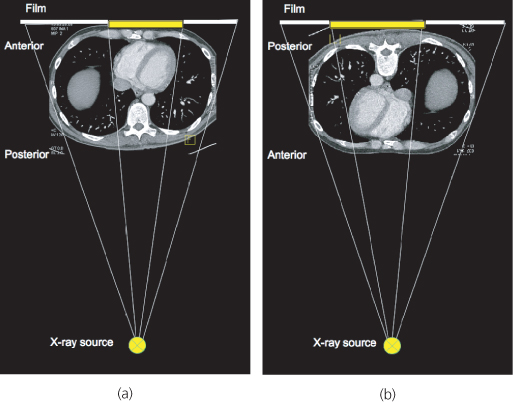
Both views have advantages and limitations (Table 12.1) (Figure 12.3).
Table 12.1 Advantages and limitations of PA and AP CXRs.
| Posteroanterior (PA) | Anteroposterior (AP) |
| Excellent visualisation of lungs and mediastinum | Reasonable for lungs, poor for mediastinum |
| Poor for evaluating the skeleton | Good for evaluating the skeleton |
| Cannot be performed supine or portable | Can be erect or supine, and portable if necessary |
| Patient can be well-centred | Patient may be rotated |
| Can ensure better inspiration | May have a poor inspiration |
Figure 12.3 Differences in magnification of the cardiac contour on PA and AP projections, illustrated using an axial CT. The cardiac contour is represented by the yellow region on the film. (a) On the PA image, the heart is closest to the film, and so the magnification is kept to a minimum, compared to (b) the AP image.
The lateral view is not normally performed in the emergency setting but can be useful in evaluating suspected sternal fractures or manubriosternal dislocation.
Computed tomography (CT)
CT scans can provide more cross-sectional detail of the thorax compared to standard CXR (Box 12.1). This is especially because CT scans do not suffer from the superimposition of structures (e.g. the mediastinal structures over one another and over the vertebrae; or the ribs, clavicle and scapula over the upper lungs).
- To further characterise abnormalities detected on CXR
- To exclude pathology when clinical suspicion is high, but the CXR is normal (e.g. vascular injury, acute aortic syndromes and pulmonary embolism)
- In major trauma
The patient is placed on a table that is moved along its axis through a rotating gantry with an X-ray source and detectors positioned at opposite ends. Images reconstructed from the signals transmitted by the detectors provide detail regarding location (anatomy) as well as the density.
Scans are often performed with intravenous iodinated contrast, unless there are contraindications such as severe asthma, allergy or renal impairment. The timing of scanning with respect to contrast injection can be optimised to visualise the structures of most interest, such as the aorta during a CT aortogram.
Modern multidetector CT (MDCT) scanners allow quick scanning in a single breath-hold, with little distortion, and also allow synchronisation of scanning with the cardiac cycle (cardiac gating), as long as there is no limiting arrhythmia or tachycardia. This can provide good visualisation of the heart if required. MDCT scanners can provide 2D reconstructions in multiple planes, and 3D reconstructions to highlight specific structures.
On axial (transverse) CT images, the body is viewed from a ‘bottom looking up’ perspective, such that the patient’s right will be located on the left of the image, and vice versa. The images can be viewed to show different structures, such as the lung, soft tissue or skeleton (greyscale windows) and in different planes (multiplanar reconstructions—MPR) or in 3D.
Figure 12.4 Ultrasound demonstrating a loculated right empyema (E), above the right hemidiaphragm (D). RLL, right lobe of liver.
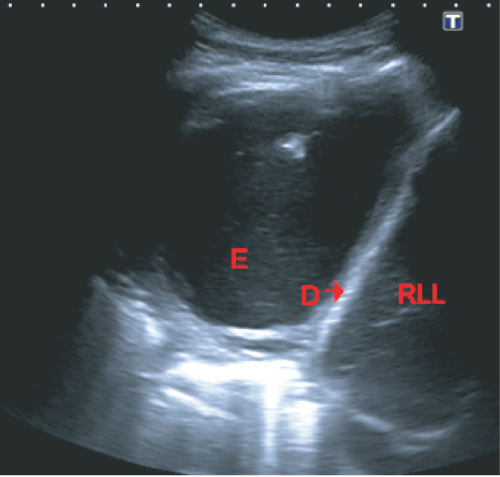
Ultrasound (US)
US assessment of the thorax is usually helpful in confirming or excluding pleural fluid, and in guiding thoracocentesis (Figure 12.4). Thoracic US is usually performed with the patient sitting upright if possible.
CXR anatomy
The lungs above the diaphragm are conventionally divided into upper, mid and lower ‘zones’ to facilitate description, but these do not bear any correlation to normal anatomical landmarks. Each of these zones occupies arbitrarily one-third of the height of the lungs.
Only the horizontal fissure (which divides the right upper lobe from the middle lobe) is usually seen on a normal PA CXR.
A significant volume of lung parenchyma lies posterior to the heart and below the level of the diaphragm. The diaphragm is attached onto the 12th rib inferiorly. The posterior ribs lie horizontally and arise from the spine. The anterior ribs tend to slope inferiorly and anteriorly, and they fade medially (due to the orientation of the anterior aspects of the ribs as they join the sternum).
The right side of the mediastinum (superior to inferior) consists of the right brachiocephalic vein, superior vena cava and right atrium. The left mediastinal border (superior to inferior) comprises the left subclavian artery, aortic arch, main pulmonary artery, left atrial appendage and left ventricle.
The hila are usually smooth and taper laterally. The right hilum is usually lower than the left, but may be at the same level in about 3% of cases. The right hilum should never be higher than the left (Figure 12.1).
ABCs structured assessment
An ABCs system of assessment can be applied to CXRs and adapted to thoracic CT scans. An ABC method specifically for reviewing the lungs may also be used. Once such approaches have been completed, however, one should always ask if the specific clinical question has been satisfactorily answered.
- Adequacy, airways, all lines
- Breathing
- Circulation
- Diaphragm
- Edges
- Skeleton, soft tissues
- Adequacy, airways, all lines
- Breathing
- Circulation, central structures
- Diaphragm
- Edges
- Skeleton, soft tissues
- Apical zone
- Basal zone
- Central (middle) zone
- Density
- Extra signs
Adequacy
Check:
- Demographic details
- Side markers
- Type of film
- Coverage: entire lung should be covered, from apices to costophrenic angles
- Inspiration: at least five anterior ribs should be seen above the midpoint of the hemidiaphragms
- Rotation: medial ends of the clavicles should be equidistant from the spinous process of the vertebra at that level. Some degree of rotation may be acceptable, as long as the film is still interpretable
- Exposure: on a correctly exposed film, the lower thoracic vertebrae (T8/T9 disc) and the left lower lobe pulmonary vessels should be visible through the cardiac silhouette
Airways
The trachea should be central above the manubrium but deviates slightly to the right below this. The right mainstem bronchus should have a more vertical alignment than the left main bronchus. Check the position of the endotracheal tube, and exclude foreign bodies while assessing the airways.
Any deviation towards a particular side that is not accounted for by rotation suggests either:
- Ipsilateral volume loss: collapse (Figure 12.5), scarring, fibrosis, or surgery; or
- Contralateral mass effect: tension pneumothorax, haemothorax, or large effusion.
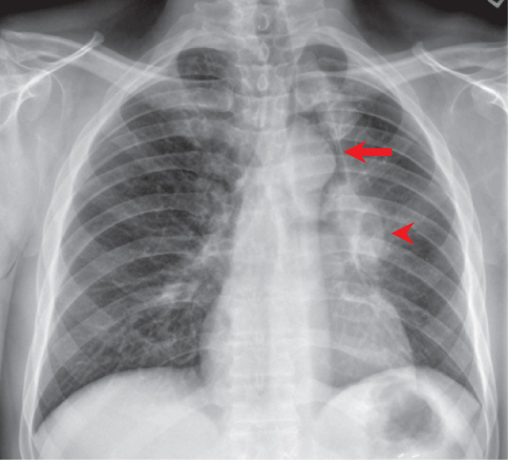
Figure 12.5 Left upper lobe collapse with tracheal deviation to the left. The left upper lobe collapses anteriorly, resulting in a decreased size of the left lung, with a veil-like opacity. A lucency is noted adjacent to the aortic knuckle (arrow), due to the compensatory expansion of the apical segment of the left lower lobe between the collapsed left upper lobe and the aortic arch. This is known as the ‘Luftsichel’ sign. The collapse is due to a left hilar mass (arrowhead).
All lines
Endotracheal tube
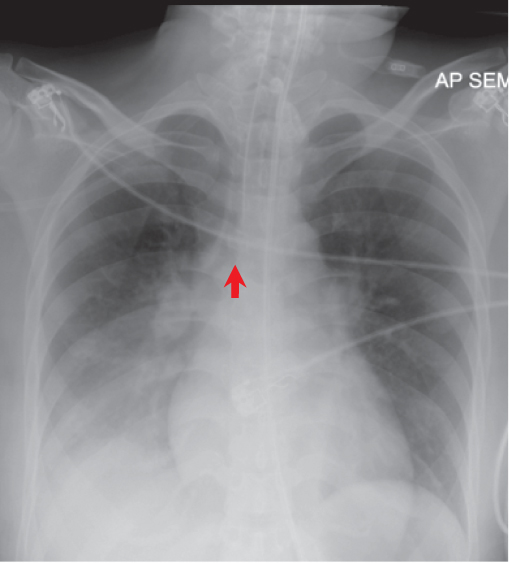
The tip of the endotracheal tube should be at the level of the aortic arch or at least 3.5–5.5 cm above the carina, if the neck is in extension (Figures 12.6 and 12.7). Having the tip of the endotracheal tube at least 3.5 cm above the carina ensures that the tube does not extend past the carina if the neck is flexed, and so is less likely to obstruct a main bronchus.
Figure 12.6 Intubated patient on general intensive care unit. Satisfactory position of the endotracheal tube (arrow), right subclavian vein central venous catheter (block arrow), and nasogastric tube passing below the diaphragm (arrowhead).
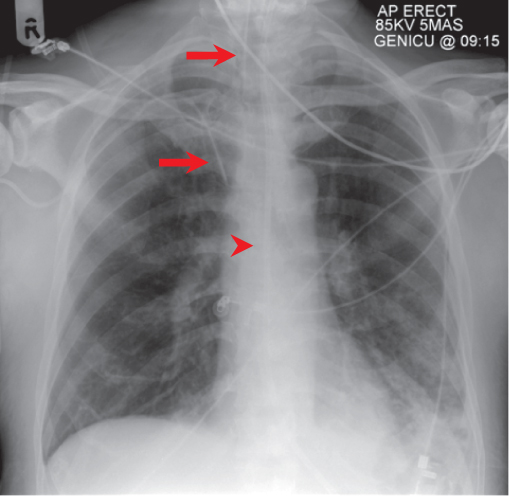
Figure 12.7 Suboptimal endotracheal tube position, approximately 1.5cm proximal to the carina (arrow). Note the right lower lobe consolidation- this had developed secondary to collapse of the right lower lobe due to previous positioning of the endotracheal tube in the right lower lobe bronchus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree