2The London Independent Hospital, London, UK
- Hands and wrist fractures account for 20% of acute fractures
- Age alone can accurately predict most injuries
- Plain radiographs remain the mainstay of imaging
- MRI (and CT) are developing increasing roles
- Aim is to restore function and avoid chronic disability
Injuries to the hand and wrist are very common, accounting for 20% of acute fractures presenting to emergency departments. The hand is the most active part of the body, is the least well protected and thus is often injured.
Most injuries to the wrist occur following a fall onto an outstretched hand (FOOSH). Mechanism of injury in these patients can accurately predict injury pattern. Age alone also can accurately predict likely fracture pattern (Table 2.1).
Clinical exam is usually accurate in this scenario and strong clinical suspicion for fracture can often direct close radiologic evaluation for subtle abnormalities.
The goal of treatment is rapid restoration of function with attention given to the prevention of chronic disability. Plain radiographs are the mainstay of imaging. Computed tomography (CT) and magnetic resonance imaging (MRI) are developing increasing roles, particularly as their availability increases.
Anatomy
Hand
Each ray, apart from the thumb, consists of a metacarpal and proximal, middle and distal phalanges. The thumb has a metacarpal and proximal and distal phalanges. At each metacarpophalangeal (MCP) joint and interphalangeal (IP) joint, lateral stability is provided by the collateral ligaments. The joint capsule at the MCP and IP joints also demonstrate on the volar aspect areas of dense fibrous thickening, known as the volar plate, which provide further strength. Each finger has two flexor tendons on the volar (palmar) surface and an extensor tendon complex on the dorsal surface.
Table 2.1 Age as a predictor of distal radial fractures following FOOSH.
| Age | Fracture pattern |
| <10 | Transverse metaphyseal (often incomplete) |
| 10–16 | Epiphyseal plate (Salter–Harris type injury) |
| 17–40 | Scaphoid and triquetral fractures |
| >40 | Transverse distal radial fractures |
Wrist
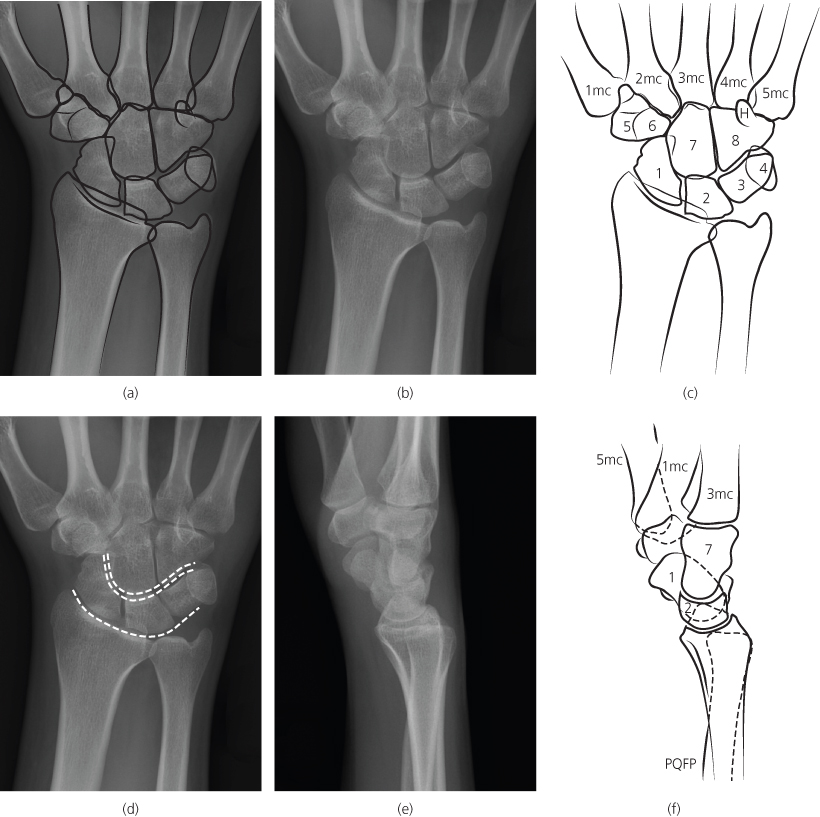
The wrist (Figure 2.1a–c, e and f) consists of eight carpal bones arranged in two rows. The proximal row (scaphoid, lunate, triquetrum and pisiform) articulates wth the radius and ulna and the distal row (trapezium, trapezoid, capitate and hamate) articulates with the bases of the metacarpals. The distal row is more rigid and stable than the proximal. These bones are held together by a complex arrangement of strong ligaments. The radiocarpal joint has a 4–15° volar tilt and the hand is usually held in slight flexion and ulnar deviation. The radial styloid is distal to the ulnar styloid. Radial inclination to the ulna is assessed on the PA view and should be 20–25°.
Figure 2.1 (a) Normal AP view with line drawing; (b) normal AP view; (c) AP view of right wrist: scaphoid (1), lunate (2), triquetrum (3), pisiform (4), trapezium (5), trapezoid (6), capitate (7), hamate (8), hook of hamate (H), metacarpal (mc); (d) Gilula’s three carpal arcs; (e) normal lateral view; (f) line drawing lateral view.
In children the carpal bones first appear at the age of 3 months and all of the carpal bones are visible by 12 years. The age of a child can be estimated by counting the number of epiphyses minus one (see Chapter 16).
ABCs systematic assessment
- Adequacy—check correct views have been obtained
- Alignment—check the relationship of the individual bones to each other
- Bone—trace the contours of all the bones
- Cartilage and joints—joint spaces should be uniform in width
- Soft tissues—change windows to look for soft tissue swelling and foreign bodies (FBs)
- Hands—anteroposterior (AP), lateral or oblique
- Fingers—AP, lateral or oblique
- Wrist—AP, lateral ± oblique
- Scaphoid—coned scaphoid series (× 4)
Adequacy
The clinical findings should guide the radiologic views to be obtained. At least two views are mandatory and additional views may be necessary for specific injuries, such as scaphoid injuries, where coned views with an AP, lateral, oblique and a dedicated scaphoid view are indicated. MRI and CT are becoming increasingly available and are being used even in the acute setting.
Hand
AP, lateral and oblique views are recommended for finger and hand injuries.
On the lateral views the fingers should be flexed to varying degrees to avoid overlap and confusing composite shadows.
Wrist
In general a minimum of posteroanterior (PA) and lateral views are recommended, but in addition some centres advocate external oblique views whereby the radial side of the wrist is elevated. If a scaphoid fracture is suspected, a PA view with ulnar deviation and also a dedicated scaphoid view with 20–30° of tube angulation are recommended in addition to a lateral and an oblique view (Figure 2.2).
Figure 2.2 Scaphoid coned PA view in ulnar deviation allows for visualisation of the full length of the scaphoid.

On a true lateral wrist view, the palmar surface of the pisiform bone should overly between the palmar surfaces of the distal scaphoid pole and the capitate head.
CT is typically reserved for suspected fractures with negative initial and follow-up radiographs or for preoperative planning in cases with significant comminution and intra-articular extension. MRI is rarely indicated acutely, although some centres are doing MRIs on patient’s with anatomical snuff box tenderness who have normal plain X rays (XRs) to exclude scaphoid fractures.
Alignment
In alignment we look at bones and their relationship to each other.
Hand
Bony surfaces should be congruent along each ray from the metacarpals to distal phalanges. Alignment should always be assessed on at least two views. On AP views, overlap of joint margins may be the only indication of subluxation/dislocation. The carpometacarpal articulations in particular, where some degree of overlap is unavoidable, should be carefully scrutinised. Dislocations here may be overlooked.
Wrist—AP view (see Figure 2.1a )Wrist—AP view (see Figure 2.1a )
The intercarpal joint spaces should be uniform and <2 mm wide. Widening following injury, seen most commonly at the scapholunate articulation resulting in the Terry Thomas or Madonna sign, may be indicative of joint dissociation and ligamentous injury. The proximal and distal carpal rows form three arcs (Gilula’s three carpal arcs). Arc 1 outlines the proximal surface of the scaphoid, lunate and triquetrium. Arc 2 outlines the distal surface of these same bones. Arc 3 outlines the proximal surface of the capitate and hamate bones. Disruption of one of these arcs suggests pathology at that site (Figure 2.1c).
The lunate should have a square (quadrilangular) shape. A ‘pie-shaped’ (triangular) lunate indicates a perilunate or lunate dislocation.
Wrist—lateral view (Figure 2.3)Wrist—lateral view (Figure 2.3)
This can be daunting as there is significant overlap of many of the carpal bones! It is crucial to assess the alignment of the distal radius, lunate, capitate and 3rd metacarpal. The lunate is moon shaped (lunar = moon) and lies on its back on the distal radius (saucer on table). The proximal pole of the capitate sits into the concave distal surface of the lunate (cup in the saucer) and the third metacarpal should line up with the distal pole of the capitate. Interruption of this alignment is usually secondary to a perilunate or lunate dislocation (and should result in careful assessment for associated carpal and distal radial fractures).
Figure 2.3 Normal lateral view of the wrist outlining the normal relationship of the lunate and capitate bones and normal anatomy.

Bone
Trace the cortical contour of each bone on each projection. Fractures typically consist of a cortical step deformity, which may be visible on only one view. In more subtle cases there may be a subtle intramedullary lucency without significant visible cortical breach at initial presentation. Impacted or healing fractures may be manifested as an ill-defined sclerotic or dense band. As with all fractures, the location, direction, displacement, angulation and comminution of the fracture as well as the involvement of the articular surfaces should be assessed.
On the AP view, the normal fused distal radial epiphysis may present a slight irregularity on the radial aspect and may mimic a fracture. The dorsal surface of the distal radius typically shows a small area of irregularity representing Lister’s tubercle, a normal anatomic landmark. Similarly vascular grooves in the mid shaft of the phalanges may mimic a fracture. Remember to use the digital ‘windows’ to look for soft tissue swelling associated with subtle fractures and to help with tricky calls.
Cartilage
Joint spaces should be uniform in width. Narrowing may be due to technical factors (rotation, flexion, tilting) or disease (arthritis).
Soft tissues
Careful attention should be paid to the cortical margins in regions of soft tissue swelling. Digital windowing of a radiograph may be required to adequately assess for soft tissue swelling particularly if the radiograph is overexposed. There is a fat plane volar to the distal radial metaphysis, along the volar aspect of the pronator quadratus muscle. This may be displaced (convex anterior surface) or obliterated in distal radial fractures. In the hand and wrist, soft tissue swelling often also spreads distal to the point of injury.
Figure 2.4 Crush fracture distal phalanx, AP view.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree