Case presentation
A 17-year-old male presents to the Emergency Department after being shot in the back. He reports chest pain and dyspnea. His vital signs are a heart rate of 110 beats per minute, a blood pressure of 110/75 mm Hg, and a respiratory rate of 25 breaths per minute. His physical examination is significant for an entry wound in his right axilla without any obvious exit wound. He also complains of right upper quadrant abdominal pain on palpation, although there is no external sign of injury.
Imaging considerations
Imaging modality choice depends on the mechanism of injury and the clinical examination. Children with a reliable, unremarkable physical examination who have sustained isolated minor thoracic trauma generally do not require imaging. While there are no specific thoracic trauma clinical scenarios that mandate chest imaging, children who have sustained major thoracic trauma (such as penetrating injury); have significant associated injuries (such as femur fracture, intracranial hemorrhage); have multisystem trauma, significant hemothorax, or hemothorax that is not resolving or worsening; or have abnormal physical examination findings should undergo imaging. Particular attention should be given to abnormalities in blood pressure, Glasgow Coma Scale score, respiratory rate, focal chest findings, or the presence of femur fractures, as these findings have been shown to correlate with thoracic injury. There are several imaging options available to the clinician.
Plain radiography
Readily available, cost effective, and with minimal ionizing radiation exposure, plain radiography of the chest is the first-line imaging modality in the pediatric patient with thoracic trauma. Clinically significant injuries are readily identified, such as hemothorax and pneumothorax. While anteroposterior (AP) and lateral views are helpful, an AP view is acceptable in a trauma scenario.
Computed tomography (CT)
Guidelines for the use of CT in blunt or penetrating pediatric thoracic trauma are lacking. However, CT is generally not a first-line imaging modality in most pediatric thoracic trauma, and its routine use, particularly in blunt thoracic trauma, is not encouraged.
Blunt thoracic trauma
CT has been shown to be overused in pediatric blunt thoracic trauma. , While CT is superior to plain radiography in the diagnosis of pediatric thoracic injuries such as pulmonary contusion and pneumothorax, identification of these injuries by chest CT does not change management in most cases. , The mechanism of injury and an abnormal chest x-ray have been proposed as reliable predictors of significant thoracic injury in pediatric patients with blunt thoracic trauma, suggesting that routine chest CT in these patients is not indicated. CT use is better reserved for patients with concerning abnormal physical examination findings and/or initial plain radiography findings that need further clarification of identified pathology. , , Clinical prediction rules for significant thoracic injury in pediatric patients have been developed , and show promise in reducing unnecessary ionizing radiation exposure by limiting the use of chest CT in pediatric patients who have sustained blunt thoracic trauma.
Penetrating thoracic trauma
There are clinical situations where chest CT imaging may be indicated and useful. Penetrating thoracic trauma can produce cardiac or vascular injuries, including the great vessels. Although this injury mechanism is rare in pediatric patients, such injuries are associated with higher mortality. Consider utilization of chest CT in children with suspected cardiovascular injuries or if there is concern for tracheobronchial tree injuries. , It is also reasonable to consider employing chest CT in children with abnormal initial chest radiographs suggestive of aortic injury, such as a widened mediastinum. If CT imaging is employed, contrast-enhanced CT angiography is indicated to evaluate vessels for injury.
Thoracic ultrasound (US) and echocardiography
Focused Assessment with Sonography for Trauma (FAST) is recognized by the American College of Surgeons as an adjunct in the evaluation of pediatric trauma patients but is an evolving technique in this population and is currently not supported as a routine imaging modality. , Thoracic sonography has, however, proven useful in the identification of pleural and pericardial fluid. , The use of thoracic US as a component of the eFAST (extended FAST) examination in adult populations has proven adept at the identification of pneumothorax with emerging applications in the identification of rib fractures and pulmonary contusions. , Echocardiography should be obtained in children with history or physical examination findings suggestive of cardiac injury, elevated cardiac biomarkers (e.g., troponin), or an abnormal electrocardiogram (ECG) to assess for pericardial effusion.
Imaging findings
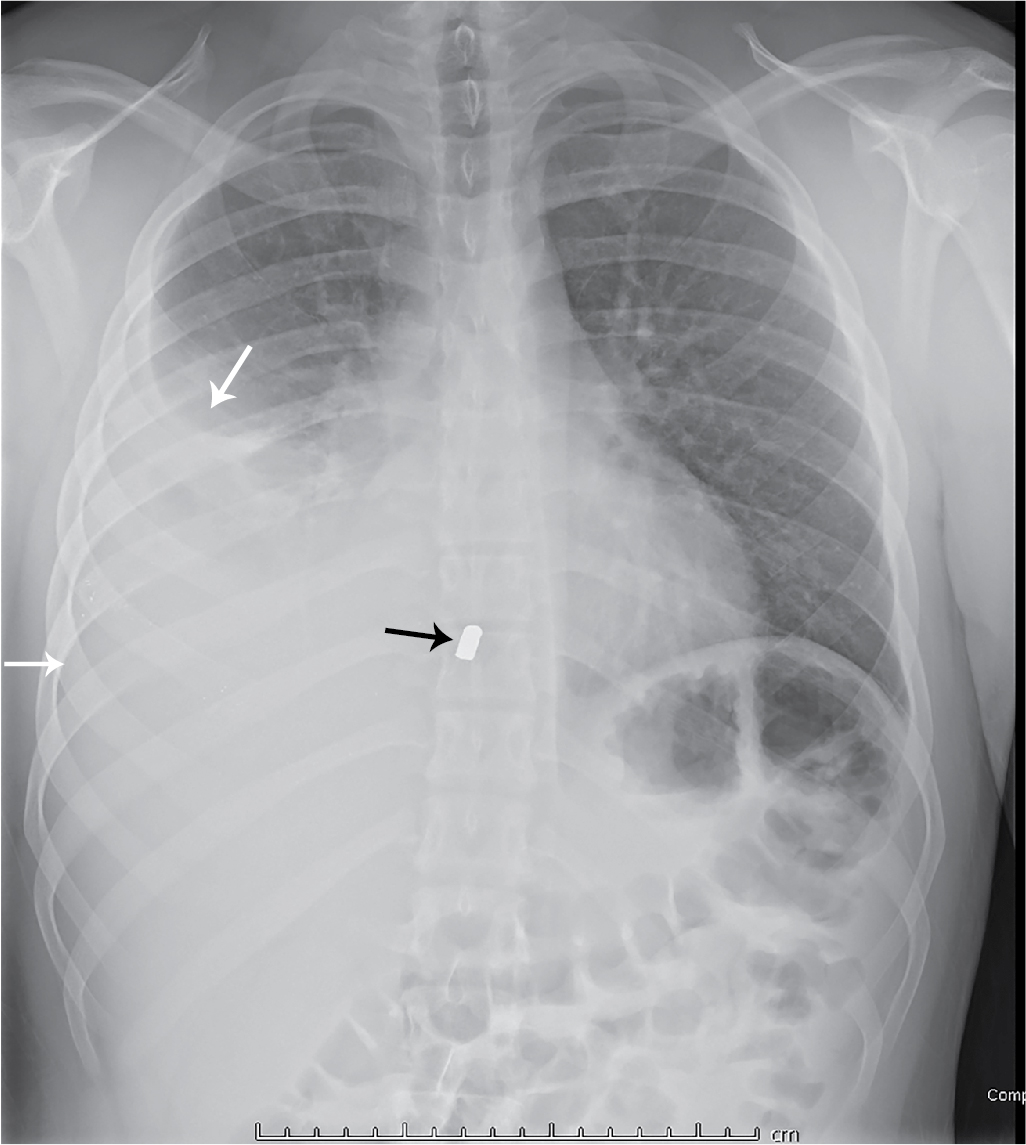
This patient had initial plain radiography of the chest ( Fig. 47.1 ). There is a moderate-sized right pleural effusion, presumed to be a hemothorax given the history of trauma, with a metallic foreign body, presumed to be a bullet fragment. There is no pneumothorax. A chest tube was placed ( Fig. 47.2 ) and a total of 600 mL of blood was ultimately obtained.