Chest Trauma
In European countries, blunt chest trauma is significantly more common than penetrating chest trauma (e.g., gunshot or stab wounds). Two-thirds of all blunt chest injuries are caused by road traffic accidents, with a mortality rate of up to 25%.1 Whole-body CT is the mainstay imaging modality in emergency polytrauma management. The image reconstruction speed of modern CT scanners is fast enough to provide the entire image dataset for clinical decision-making within a very short time. Therefore, CT has now supplanted radiography of the chest and pelvis for management of hemodynamically stable polytrauma patients.2,3
Nonetheless, chest radiography continues to have its place for hemodynamically unstable patients. It is easier to perform than CT, if necessary, even during ongoing resuscitation, and is able to demonstrate a number of important findings (e.g., tension pneumothorax, large hemothorax, malpositioned implants).2
For CT, intravenous contrast injection is needed to detect vascular injuries and rupture of parenchymatous organs. Sagittal image reconstructions are useful for accurate diagnosis of spinal injuries. With volume rendering technique (VRT) even complex bone fractures can be quickly and clearly visualized.
15.1 Blunt Chest Trauma
15.1.1 Lung Parenchyma
Almost one of every two patients with blunt chest trauma has lung contusions. This involves alveolar hemorrhage and interstitial edema in the region of the greatest mechanical impact on the lung parenchyma (coup and, possibly, contrecoup). CT demonstrates ill-defined ground-glass opacities of variable density, which may evolve to consolidations (▶Fig. 15.1). At times, massive contusions trigger adult respiratory distress syndrome. Lung contusions resolve within a few days. Conversely, persistent pulmonary opacities are suggestive of another cause, such as infection, aspiration, blood clot, or atelectasis.
 Fig. 15.1 Lung contusion. CT image. Ill-defined ground-glass opacities in the right upper lobe. Furthermore, moderate dependent opacities in the posterior lower lobes. |
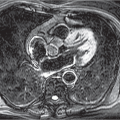
Lung lacerations result from rupture of the lung tissue. They may be solitary or multiple. Air-filled cavities are consistent with pneumatoceles, whereas consolidations are caused by hematomas. A combination of these two types with fluid-fluid levels is possible (▶Fig. 15.2). Pneumatoceles generally resolve with parenchymal scarring within 1 to 3 weeks.4
Aspiration pneumonia manifests within the first day of injury as pulmonary opacity. It is typically located in the posterior portions of the lower lobes.
15.1.2 Mediastinum
Pneumomediastinum is suggestive of a rupture of the trachea, esophagus, or central, mediastinal bronchi. Occasionally, acute life-threatening tension pneumomediastinum occurs. On chest radiography, pneumomediastinum may be misinterpreted as pneumothorax if air is seen only beneath the mediastinal pleura and no other mediastinal air collections are visible.2 The risk of misinterpretation is much lower on CT. Pneumomediastinum often spreads to adjacent compartments, causing cervical and thoracic soft-tissue emphysema (▶Fig. 15.3).
Tracheobronchial ruptures are relatively rare. They very often involve the right mainstem bronchus. The resultant posterior displacement of the collapsed lung is known as “fallen lung sign.” Tracheal tears usually occur in the lower tracheal at the transition from the cartilaginous to the membranous part (▶Fig. 15.4).
Rupture of the esophagus is rarely seen in its thoracic part since the dorsal location confers good protection. The cervical esophagus is more commonly affected. Thoracic esophageal rupture is associated with a mortality rate of 90%, generally because of acute mediastinitis.4
Many vascular injuries involve the thoracic aorta. By contrast, the other mediastinal vessels are rarely implicated. It has been estimated that around three-quarters of all patients with aortic rupture do not reach the hospital alive; likewise, the mortality
rate within the first 24 hours in the hospital is considerable.5,6 Aortic injuries are classified into four types or severity grades7,8:
rate within the first 24 hours in the hospital is considerable.5,6 Aortic injuries are classified into four types or severity grades7,8:
 Fig. 15.2 Lung lacerations. CT image. Cystic structures (pneumatoceles) in both lower lobes, one with a small air-blood level (arrow). Besides, small left pneumothorax, small left pleural effusion and lung contusions. |
Type I: intimal tear.
Type II: intramural hematoma.
Type III: pseudoaneurysm.
Type IV: rupture.
 Fig. 15.4 Tracheal rupture. CT image. Defect at the transition from the cartilaginous to the posterior membranous part of the trachea (arrow). Resultant mediastinal emphysema and massive thoracic soft-tissue emphysema. |
 Fig. 15.5 Mediastinal hematoma. CT image. Retrosternal structure of soft-tissue density (arrows). Furthermore, pseudoaneurysm of the descending aorta (arrowhead). |
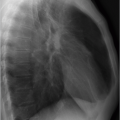
Detection of a mediastinal hematoma on CT is suggestive of aortic injury (▶Fig. 15.5). Tears in the vascular wall, thrombi in the aortic lumen, pseudoaneurysm (▶Fig. 15.6), and contrast extravasation secondary to rupture can be directly visualized. Contour discontinuity, a double aortic lumen, or pseudocoarctation are seen additionally. The latter term describes the abrupt tapering of the aortic lumen distal to the left subclavian artery compared with the ascending aorta.3 Around 90% of aortic injuries occur in the anteromedial portion of the aortic isthmus distal to the origin of the left subclavian artery9 because at this site the ligamentum arteriosum fixes in place the aortic arch. While type I aortic injuries (intimal tear) need only conservative therapy, emergency treatment is recommended for the other types, preferentially with endovascular stentgraft placement.8 For hemodynamically unstable patients, it is
important that aortic injury be diagnosed based on the radiography findings (▶Fig. 15.7), as presented in Table 15.1. Negative chest radiography just about rules out aortic rupture (predictive value 96-98%).7,10
important that aortic injury be diagnosed based on the radiography findings (▶Fig. 15.7), as presented in Table 15.1. Negative chest radiography just about rules out aortic rupture (predictive value 96-98%).7,10
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree