The elbow is composed of a complex set of articulations that allow two degrees of freedom of motion: elbow flexion and extension and forearm pronation and supination. These articulations facilitate the positioning of the hand in space and help to stabilize the upper extremity for power and detailed work activities. The elbow or cubital articulations are made up of the ulnohumeral joint and the radiohumeral joint and a third articulation between the proximal radius and ulna. The ulnohumeral or trochlear joint is a hinge joint that allows elbow flexion and extension. Because the axis of this articulation is oriented distally and medially, a valgus tilt averaging 5 to 7 degrees results, which contributes (along with the valgus orientation of the ulnar shaft with respect to the olecranon) to the “carrying angle” of the elbow (1). The radiohumeral and proximal radioulnar joints allow forearm rotation. The radiohumeral joint is a uniaxial hinge joint between the capitellum and the radial head, whereas the proximal radioulnar joint is a uniaxial pivot joint. The stability of the elbow is highly dependent on the congruity of these articulations.
In addition, the ulnohumeral and radiohumeral joints are stabilized medially by the ulnar collateral ligament complex (sometimes referred to as the medial collateral ligament complex) and laterally by the lateral ulnar collateral ligament complex. The ulnar collateral ligament complex (Fig. 9.1) is composed of the anterior oblique (occasionally referred to as the “bundle”), posterior oblique (bundle), and transverse ligaments, with the anterior oblique ligament being the primary stabilizer of the elbow against valgus stress (2, 3). Furthermore, the anterior band of the anterior oblique ligament is the primary restraint to valgus stress at 30, 60, and 90 degrees of flexion (4). Although the anterior band is the primary restraint to valgus stress in the overhead athlete, it is believed that the posterior band is more important at higher degrees of flexion (5).
The lateral ulnar collateral ligament complex (Fig. 9.2) is composed of the radial collateral, lateral ulnar collateral, annular, and accessory collateral ligaments. Whereas the ulnar collateral ligament complex is comprised of discreet bands, the lateral ulnar collateral ligament complex is less well defined. The main function of the complex is to provide stability to the elbow during external rotation and varus stress. Insufficiency of the complex may result in the development of posterolateral rotatory instability with subluxation of the radial head posteriorly (6–8). The proximal radioulnar joint is stabilized by the annular ligament.
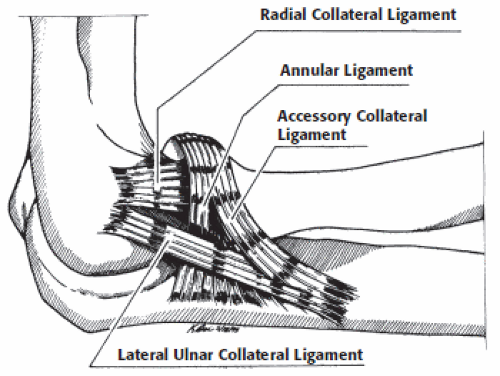 Figure 9.2 The lateral ulnar collateral ligament complex is composed of the radial collateral, the lateral ulnar collateral, the annular ligament, and the accessory collateral ligament. |
The dynamic contribution of the muscles and tendons to elbow stability under normal conditions is minimal (9, 10). Significant demands are placed on both the static and dynamic structures of the elbow, which, when damaged with overuse injuries (e.g., medial epicondylitis or ulnar collateral ligament tears) or trauma (such as in an elbow dislocation), may lead to loss of normal elbow function. This Chapter discusses the clinical assessment of the painful elbow with special attention given to the pathologic entities best evaluated by MRI.
Documentation and Scoring
Several elbow scoring systems have been developed to assist in objectively assessing preoperative symptoms and function and postoperative outcomes. The goal is to provide a reproducible, controlled system of comparing treatment outcomes from various centers. Morrey et al. (11) published a numeric scoring system (known as the Mayo elbow performance index) for the evaluation of elbow pain, motion, strength, instability, and function, which has proven to be useful in evaluation of patient outcomes. Other elbow scoring systems have been introduced by the Hospital for Special Surgery, Pritchard et al. and Morrey and Andrews (12, 13). The degree of elbow function or disability may also be evaluated with use of the Modified American Shoulder and Elbow Surgeons patient self-evaluation form (14) and the Disabilities of the Arm, Shoulder and Hand questionnaire (15). The former focuses exclusively on functional limitations, whereas the latter incorporates questions related to functional limitations, symptoms, and psychosocial problems.
History
A thorough evaluation of any orthopaedic disorder would be incomplete without a detailed history. In the evaluation of the elbow, the history is even more crucial when physical findings are subtle and radiographs are normal. The mechanism of injury and the character and chronicity of the patient’s symptoms help to delineate the possible causes of elbow pain or dysfunction and complement the physical examination and radiographic findings in the efficient formulation of a diagnosis.
In recording a thorough history, one should begin with documentation of the patient’s demographic information. The age, sex, hand dominance, vocation, and sports that the patient may participate in are determined. The normal level of activity of the patient is determined because treatment of the injured elbow in the dominant extremity of a professional athlete may be different from the treatment of an injury to the nondominant elbow of an elderly patient.
Information regarding the chief symptom is then obtained. The patient should be asked to detail the time
course, severity, chronicity, and treatment course of his or her injury. The patient should be asked about the sequence of events leading him or her to seek treatment. Additionally, the physician should inquire about previous elbow injuries and previous treatments, surgeries, or studies that have been obtained, which might aid in diagnosis and formulation of a treatment plan.
course, severity, chronicity, and treatment course of his or her injury. The patient should be asked about the sequence of events leading him or her to seek treatment. Additionally, the physician should inquire about previous elbow injuries and previous treatments, surgeries, or studies that have been obtained, which might aid in diagnosis and formulation of a treatment plan.
Detailed information should then be obtained about the patient’s signs and symptoms. Information about bruising or swelling noted by the patient in the injured elbow should be obtained, including the location and severity. Patients should be asked not only if they have pain, but also if they have symptoms of instability, weakness, crepitus, locking, stiffness, loss of motion, numbness, or paresthesias. Frequently, patients may report only of loss of function if they are unable to clearly identify their symptoms. This is particularly the case in high-level throwing athletes, who may present for evaluation with vague symptoms such as a reduction in pitching velocity or control or numbness or tingling in the ulnar nerve distribution, which is often associated with medial elbow instability.
Each of the patient’s symptoms should be addressed individually in detail. If the patient reports pain, then the location, duration, character, and timing of the pain should be determined. The physician should also inquire about symptom aggravators and relievers (such as pulling, pushing, supination, throwing, the use of anti-inflammatories, and rest). Often, the characteristics of the symptoms help to narrow the examiner’s differential diagnosis. For instance, symptoms of locking are classic for loose bodies in the elbow, whereas a history of the athlete feeling an acute “pop” on the medial side of the elbow followed by a sudden loss in throwing velocity suggests an ulnar collateral ligament tear. Pain with a loss of motion of the elbow may indicate elbow arthritis or an osteochondral defect. A determination of the pain medicine requirements, including type (e.g., nonsteroidal, narcotic) and frequency of medication taken, provides an objective gauge of the patient’s pain level.
The etiology of the elbow disorder should then be determined. Elbow dysfunction may occur as a result of a variety of mechanisms, including overuse in injuries such as tendinitis, traumatic injury (such as elbow dislocation or distal biceps rupture), or extrinsic causes such as referred shoulder pain, brachial plexus neuropathy, or cervical spine disorders. Patients presenting with overuse elbow problems rarely recall a specific injury, but may relate a history of heavy or repetitive lifting, a change in training regimen or equipment, or a new household project. Although patients with overuse injuries frequently do not recall an initial injury, they are usually able to articulate their symptoms and can often demonstrate exacerbating motions and positions of the extremity, which will cause pain.
In contrast, patients with traumatic elbow injuries seek medical care because of an acute event. The mechanism of injury may be recalled clearly by the patient. A fall onto an outstretched hand may result in an elbow dislocation or fracture. A sudden, forceful eccentric contraction of the muscles about the elbow may result in a distal biceps or triceps rupture. Because these patients usually present acutely, their initial symptoms are frequently global and not always specific. Patients who present after an acute injury should be questioned carefully about the mechanism of the initial injury and subsequent treatment. If the patient was taken to the emergency room, information about clinical findings and any radiographs taken at the time should be obtained. If the patient sustained an elbow dislocation, the direction of the dislocation and information on the postreduction stability examination should be obtained. The patient should also be carefully questioned about the location of swelling and bruising that developed after the acute injury and if he or she experienced any numbness after the event or after any treatment.
Finally, a brief medical history should be documented. Previous injuries of the cervical spine or associated neurologic problems (such as a brachial plexopathy or multiple sclerosis) may mimic elbow pathology or cause referred pain in the elbow. Any history of shoulder
or wrist problems on the ipsilateral side should also be obtained, because these may result in referred pain to the elbow or may lead to elbow pathology (like in the case of chronic distal radioulnar joint instability). A history of symptoms involving multiple joints should raise questions about a possible underlying rheumatologic disorder.
or wrist problems on the ipsilateral side should also be obtained, because these may result in referred pain to the elbow or may lead to elbow pathology (like in the case of chronic distal radioulnar joint instability). A history of symptoms involving multiple joints should raise questions about a possible underlying rheumatologic disorder.
General Physical Examination
Physical examination of the elbow is performed in a systematic fashion and should be carried out on both elbows using the patient’s uninvolved elbow as a control. The examination begins with inspection of the elbow and is followed by palpation of the anatomic structures and assessment of both active and passive range of motion. The examination is completed with a series of provocative maneuvers. Each segment of the examination should also be performed systematically to ensure that subtle abnormalities are not overlooked. Of course, in the case of an acute traumatic injury, a limited physical examination may be more appropriate depending on the degree of patient discomfort.
It is also important to incorporate examination of the cervical spine and shoulder into the elbow examination. Cervical spine pathology may cause referred symptoms to the elbow, and as such, an evaluation of the cervical spine should be routinely performed as part of the complete elbow examination. Additionally, the range of motion, strength, and stability of the ipsilateral shoulder should be documented. Shoulder pathology may lead to compensations at the elbow and subsequent injury, especially in throwing athletes.
Inspection
One of the most important, yet frequently unappreciated, aspects of the physical examination is the visual inspection. The inspection should begin as soon as the physician enters the examining room. Attention to the patient’s use of their affected arm when moving about the examination room before the formal examination begins may give the examiner clues to the problem. One of the more telling clues is noted when the patient protects the elbow when removing a shirt, sling, or protective device. Patients with significant intra-articular effusions will often keep the arm flexed to approximately 70 degrees, a position of maximal capsular volume and comfort for the patient.
First, the carrying angle of the patient’s elbow should be measured. This is measured with the elbow completely extended and with the forearm in maximal supination. The carrying angle represents the angle formed by the long axis of the humerus and the long axis of the ulna. The normal carrying angle is approximately 13 degrees in females and 11 degrees in males (16). However, older throwing athletes may have an increase in this angle (17). This angle may also appear to be increased as a result of a loss of extension. It may be decreased or even in varus (cubitus varus or “gun stock” deformity) after previous trauma such as a supracondylar humerus fracture.
Next, the examiner looks for areas of asymmetry between the two upper extremities. Asymmetry may be the result of muscle wasting, trauma, swelling, degenerative joint disease, or extrinsic disorders such as nerve injury. It is important to examine the anterior, medial, lateral, and posterior aspects of the elbow because each of these areas may reveal pathologic information. Specifically, the physician should inspect the lateral recess, olecranon, medial epicondyle region, and antecubital fossa. Joint effusion will cause fullness of the lateral recess of the elbow, an area just distal to the lateral condyle of the humerus. Olecranon bursitis will cause an area of discrete swelling over the olecranon process.
Palpation
Palpation of the elbow is used to identify defects, prominences, or tenderness of the bony or soft tissue structures of the elbow. Starting anteriorly, the antecubital fossa is palpated. The most medial structure is the median nerve followed by the brachial artery, distal biceps tendon, lacertus fibrosus, and musculocutaneous nerve. Generally only the brachial artery pulse and distal biceps tendon are palpable.
On the medial side of the elbow, the medial epicondyle of the distal humerus is the most prominent bony landmark (Fig. 9.3). It is the origin of the ulnar collateral ligament complex as well as the flexor–pronator muscle mass, comprised of the pronator teres, flexor digitorum profundus, flexor digitorum superficialis, flexor carpi radialis, palmaris longus, and flexor carpi ulnaris. Pain with palpation directly over the medial epicondyle may be indicative of medial epicondylitis in adults or possibly an injury to the medial epicondylar growth plate in a skeletally immature patient. In general, patients with medial epicondylitis have tenderness just anterior and distal to the medial epicondyle, whereas patients with ulnar collateral ligament injuries are more tender approximately 2 cm distal to the medial epicondyle. The supracondylar ridge of the humerus lies just proximal to
the medial epicondyle. This region should be palpated for enlarged lymph nodes and the presence of a congenital supracondylar process, which (along with the attached ligament of Struthers) may cause median nerve or brachial artery compression symptoms. The ulnar nerve should be palpated beginning above the medial epicondyle and then as it travels around the posterior and distal aspect of the medial epicondyle and distally into the flexor carpi ulnaris. Gentle palpation of the nerve should not be painful and should not cause radicular symptoms in the ulnar digits of the hand. The medial aspect of the triceps should also be palpated, because anomalous bands of the triceps tendon may snap over the medial epicondyle, causing ulnar nerve symptoms (18). The ulnar collateral ligament complex should be palpated starting proximally at its origin on the medial epicondyle and working distally to its insertion on the sublime tubercle of the proximal ulna just distal to the joint line. Tenderness of the ligament, especially in a throwing athlete, should raise concerns about injury to the ulnar collateral ligament complex. However, pain could also be the result of injury to the overlying flexor–pronator muscle group, and special testing may be required to delineate the nature of the pathology.
the medial epicondyle. This region should be palpated for enlarged lymph nodes and the presence of a congenital supracondylar process, which (along with the attached ligament of Struthers) may cause median nerve or brachial artery compression symptoms. The ulnar nerve should be palpated beginning above the medial epicondyle and then as it travels around the posterior and distal aspect of the medial epicondyle and distally into the flexor carpi ulnaris. Gentle palpation of the nerve should not be painful and should not cause radicular symptoms in the ulnar digits of the hand. The medial aspect of the triceps should also be palpated, because anomalous bands of the triceps tendon may snap over the medial epicondyle, causing ulnar nerve symptoms (18). The ulnar collateral ligament complex should be palpated starting proximally at its origin on the medial epicondyle and working distally to its insertion on the sublime tubercle of the proximal ulna just distal to the joint line. Tenderness of the ligament, especially in a throwing athlete, should raise concerns about injury to the ulnar collateral ligament complex. However, pain could also be the result of injury to the overlying flexor–pronator muscle group, and special testing may be required to delineate the nature of the pathology.
Posteriorly, palpation should begin with the olecranon bursa, which overlies the triceps insertion into the olecranon. Any pain with palpation, thickening of the bursa, or the presence of an olecranon osteophyte (within the substance of the triceps) should be noted. The distal triceps should also be palpated for tenderness or for a frank defect, which may be present in the case of a triceps tear or avulsion. The tip of the olecranon and the olecranon fossa are more easily palpable with the arm flexed past 60 degrees. The posteromedial aspect of the olecranon is a frequent location of osteophyte formation in throwing athletes, resulting in elbow impingement symptoms and pain on full extension. Pain with palpation in this area may indicate osteophyte formation or the presence of loose bodies.
Working laterally, the radial head is palpated posteriorly. It is easily palpated and located by repetitively pronating and supinating the elbow while axially loading the elbow. Any pain or crepitation should be noted with this maneuver as well as subluxation of the radial head, which may be indicative of elbow instability. An elbow joint effusion may also be palpated in the area posteriorly between the olecranon tip, radial head, and lateral epicondyle (Fig. 9.4). The lateral epicondyle is located 2 cm proximal to the radial head and is less prominent than the medial epicondyle. The wrist extensors (or “mobile wad of Henry”) originate on the lateral epicondyle, and tenderness on palpation in this area may suggest lateral epicondylitis. Pain with palpation of the medial aspect of the extensor bundle distal to the radial head may be indicative of radial nerve entrapment, as in radial tunnel syndrome. The lateral ulnar collateral ligament complex is less defined than the ulnar collateral ligament complex.
Range of Motion
The evaluation of both active and passive range of motion is important in the complete physical examination of the elbow. Active range of motion is tested first and identifies the functional limitations of motion. Active elbow flexion–extension and pronation–supination as well as wrist dorsiflexion and palmar flexion should be assessed. Measurements of passive range of motion are performed when limitations in active motion are noted. Limitations of active and passive elbow motion may be the result of true mechanical or static restrictions such as soft tissue contracture, degenerative joint disease, or loose bodies. Limitations in active and passive motion may also be the result of patient guarding secondary to pain. Conversely, isolated limitations in active motion (with normal passive motion) may be the result of dynamic loss as is seen in patients with neurologic deficits or tendon ruptures. Again, both elbows should be examined to determine subtle differences in motion.
Normal elbow range of motion in the sagittal plane (extension–flexion) is typically 0 to 140 degrees ± 10 degrees, whereas forearm rotation values are normally between 80 and 90 degrees of pronation and supination (19–21). Range of motion in the sagittal plane should be tested with the forearm in neutral rotation and with the arm adducted at the side, because the patient may attempt to compensate for loss of motion by changing their shoulder position. Forearm rotation should be measured with the arm adducted and with the elbow flexed to 90 degrees.
When measuring elbow range of motion, the examiner should evaluate the patient’s reports of pain during motion and at the end points and also assess for crepitation during motion. The “feel” of the end point of full extension and full flexion is also important in the evaluation. In the normal elbow, the end point in terminal extension is hard (as a result of bony contact between the olecranon tip and the olecranon fossa) and soft in full flexion (as a result of muscle impingement). In the case of motion loss, a solid end point may indicate the presence of loose bodies or spurs that are blocking
motion, whereas a soft end point may be caused by capsule contractures, joint effusion, tendon contracture, or ligament injury.
motion, whereas a soft end point may be caused by capsule contractures, joint effusion, tendon contracture, or ligament injury.
Strength Testing
Strength testing of the elbow should include motor examination of the entire extremity. This is particularly true for throwing athletes, because weakness of the rotator cuff or scapular stabilizers may lead to poor throwing mechanics and subsequent elbow injury. Therefore, a thorough motor examination of the rotator cuff, deltoid, and scapular stabilizers should be performed. Again, testing should be performed on both the injured and noninjured extremity.
In elbow strength testing, the brachialis is tested by resisting patient elbow flexion with the forearm in pronation. The strength of the brachioradialis may be tested by resisting patient elbow flexion with the forearm in neutral rotation. The biceps brachii is tested with the arm in 45 degrees of flexion with the forearm in full supination with the examiner resisting elbow flexion (22). Alternatively, the examiner may resist active patient supination with the elbow flexed to 90 degrees to test biceps brachii strength. Triceps strength may be evaluated by resisting active extension of the elbow with the forearm in neutral rotation. Resisted pronation, wrist extension, and wrist flexion should be evaluated with the arm adducted and the elbow flexed to 90 degrees and repeated with the elbow in extension. The evaluation of grip strength, thumb abduction strength, and intrinsic hand muscle strength should also be performed, because they may provide evidence of nerve entrapment syndromes of the median, posterior interosseous, and ulnar nerves, respectively (22).
Neurologic and Vascular Examination
In patients with subtle reports of elbow pain or weakness, a thorough neurologic examination must be performed. This includes an examination of sensory, motor, and reflex functions of the upper extremity because cervical spine conditions may cause referred elbow pain.
Sensation should be checked in the axillary nerve region (lateral deltoid patch), the musculocutaneous nerve (which distally becomes the lateral antebrachial cutaneous nerve, providing sensory innervation to the lateral volar aspect of the forearm), the superficial radial nerve (dorsal radial surface of the hand), the median nerve (volar surfaces of the thumb, second and third digits), and ulnar nerve (volar surfaces of the fourth and fifth digits).
Finally, a vascular examination should be performed to evaluate the patient for evidence of arterial compression or the brachial, radial, and ulnar arteries. The brachial artery and median nerve may be compressed as they pass under the ligament of Struthers, which is present in approximately 1% of the population. The ligament, when present, passes from the medial epicondyle to the supracondylar process of the humerus.
It is important to recognize that elbow symptoms may be present in thoracic outlet syndrome (TOS) or axillary venous occlusion. The modified Wright test, which is used to determine TOS, is performed by palpating the patient’s radial pulse. The patient’s arm is then placed in abduction and external rotation while the pulse is monitored. Patients are then instructed to rotate their head to the involved shoulder. A diminished pulse confirms TOS. In overhead athletes, axillary venous occlusion may occur as a result of repetitive impingement with the action of throwing (arm abduction) and is manifested by pain and venous engorgement of the upper extremity and a generalized “dead arm” feeling during throwing periods.
Specific Examinations for Elbow Pathology
There are many afflictions of the elbow that may be adequately evaluated using a thorough general physical examination complemented by the appropriate radiographic studies. These injuries include most fractures, acute dislocations, and arthritis. The clinical evaluation of soft tissue injuries of the elbow, which are some of the more common causes of elbow pain and dysfunction, may be much more difficult. These injuries include tendinitis and tendinopathies, tendon ruptures, ligamentous injuries, and nerve entrapment disorders. In the evaluation of these entities, many special signs and tests have been described to aid in the evaluation of these processes. MRI is also an important adjunct because of its ability to accurately evaluate soft tissue structures of the elbow. The following is a discussion of the evaluation of those entities in which MRI is most effectively used to improve diagnostic accuracy.
Examination of Elbow Tendinopathies
Lateral Epicondylitis
Lateral epicondylitis, or “tennis elbow,” was originally described by Major in 1883 (23, 24). Although 95% of cases are a result of causes other than tennis, it is estimated that 10% to 50% of people who regularly play tennis may have symptoms of lateral epicondylitis at some point (25–27). The onset of symptoms may be acute or gradual, and a history of repetitive flexion–extension or pronation–supination motions may be related. Among athletes playing racquet sports, the backhand is the most common swing to produce symptoms (26). Because the incidence of lateral epicondylitis is much less at the professional level, it is thought that poor swing mechanics initiate the process (27). Patients may describe a constant burning pain of the lateral aspect of the elbow that is aggravated by the actions of shaking hands, grasping objects, carrying luggage, and pouring from a pitcher.
On physical examination, patients have point tenderness over the origin of the extensor carpi radialis brevis or the entire extensor wad insertion on the lateral epicondyle. The pain increases with resisted wrist extension with the elbow extended and the forearm fully pronated. Resisted forearm supination may also aggravate the patient’s symptoms. In a modified test, the wrist may be passively volar-flexed while the elbow is in extension, further stressing the wrist extensors. The “chair test,” in which the patient is asked to lift a chair with the forearm pronated, may also elicit pain over the lateral epicondyle (28). It is important for the examiner to differentiate
between the more proximal palpable tendon tenderness of lateral epicondylitis and deep pain in the midforearm extensor area, which may be elicited with resisted supination, findings more suggestive of posterior interosseous nerve entrapment.
between the more proximal palpable tendon tenderness of lateral epicondylitis and deep pain in the midforearm extensor area, which may be elicited with resisted supination, findings more suggestive of posterior interosseous nerve entrapment.
Medial Epicondylitis
Medial epicondylitis, or medial tendinosis of the wrist flexor–pronator group, occurs far less frequently than lateral epicondylitis. Lateral epicondylitis is up to seven times more common, most likely because most grasping activities place the wrist in relative extension (29




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree