The shoulder is unique in its construction, relying primarily on soft tissue restraints for stability, yet maintaining the greatest mobility of any joint in the body allowing for motion in the sagittal, coronal, and transverse planes as well as in rotation. This range of motion is necessary for the placement of the hand in position for prehension. Significant demands are placed on both the static and dynamic structures of the shoulder, which, when damaged with overuse injuries (e.g., rotator cuff disease) or trauma such as in traumatic unidirectional instability), may lead to loss of normal shoulder function. This Chapter discusses the clinical assessment of the shoulder with special attention given to the pathologic entities best evaluated by MRI.
Documentation and Scoring
Many scoring systems have been developed to better determine objectively preoperative symptoms and postoperative outcomes, allowing for a reproducible, controlled method of comparing treatment options from various centers. In 1978, Rowe et al. (1) published a scoring system for the evaluation of results after surgery for glenohumeral instability. Similar scoring systems have been published in the evaluation of rotator cuff disease (2, 3). A more thorough scoring system was devised by Constant and Murley (4), which addressed the limitations in the aforementioned scoring systems, which were developed to quantify outcomes related to a single diagnosis. More recently, the American Shoulder and Elbow Society has adopted a standardized form that incorporates patient and physician evaluation of shoulder function, including activities of daily living, and is appropriate for the scoring of patients regardless of diagnosis (5).
History
A thorough evaluation of any orthopaedic symptom would be incomplete without a detailed history. In the examination of the shoulder, the history is even more important when physical findings are subtle and radiographs unremarkable. The mechanism of injury and the character and chronicity of the patient’s symptoms help to narrow the possible causes of shoulder pain and complement the physical examination and radiographic findings in reaching a final diagnosis.
History-taking begins with documentation of the patient’s demographic information. The age, sex, hand dominance, vocation, and avocation are determined. Intensity of activity is recorded because it has different significance between age groups; treatment of the injured shoulder in the dominant extremity of the professional athlete may be different than that necessary in the nondominant shoulder of an elderly patient. Medicolegal issues should also be determined because these may adversely affect the efficacy of treatment (6).
Information regarding the chief symptom is then obtained. Patients primarily report pain, but they may also report instability, weakness, crepitus, or stiffness or loss of motion. However, patients may report only of loss of function if they are unable to clearly identify their symptoms. The inability to recognize symptoms is not uncommon because the deep structures of the shoulder are complex.
Each of the patient’s symptoms should be addressed. If the patient reports pain, then the location, duration, character, and timing of the pain should be determined as should factors that alter the nature of the symptoms. Often, the characteristics of the painful symptoms help focus the examiner’s differential diagnosis. For instance, symptoms of night pain are classic (although not exclusive) for rotator cuff disease, whereas symptoms of the arm “going dead” acutely with overhand throwing are suggestive of anterior shoulder subluxation (7). Pain with motion of the shoulder, which is associated with crepitus, may indicate glenohumeral arthritis, but it may also have subacromial or scapulothoracic origins. A determination of the pain medicine requirements, including type (e.g., nonsteroidal, narcotic) and frequency of medication taken, provides an objective gauge of the patient’s level of pain.
The etiology of the shoulder injury should then be determined. Shoulder injuries occur by a variety of mechanisms, including overuse injuries such as impingement (8), idiopathic processes such as adhesive capsulitis (9–11), or traumatic injuries such as glenohumeral dislocation (1, 12–16) or acromioclavicular (AC) separations. Patients presenting with overuse or idiopathic shoulder problems rarely recall a specific injury; rather, they see their physician because their “shoulder hurts” (17). Although patients with overuse injuries frequently do not recall the initial injury, they are usually able to articulate their symptoms and to demonstrate exacerbating motions and positions of the extremity.
Patients with idiopathic onset of shoulder pain may be experiencing the early phases of adhesive capsulitis or calcific tendinitis. The physician should note whether pain, weakness, or loss of motion represents the primary symptom. After first considering an intrinsic etiology, the physician must always be weary of extrinsic causes of shoulder pain such as brachial plexus neuropathy or cervical spine disorders (18).
In contrast, patients with traumatic shoulder injuries seek medical care because they “hurt their shoulder”
(17). The mechanism of injury is recalled clearly by the patient. A fall onto an outstretched arm may result in a rotator cuff injury, labral injury, or fracture, whereas a posteriorly directed force applied to the arm with the shoulder in the position of abduction and external rotation may result in anterior glenohumeral instability. Because these patients usually present acutely, their symptoms are frequently initially global and not always specific (Table 3.1).
(17). The mechanism of injury is recalled clearly by the patient. A fall onto an outstretched arm may result in a rotator cuff injury, labral injury, or fracture, whereas a posteriorly directed force applied to the arm with the shoulder in the position of abduction and external rotation may result in anterior glenohumeral instability. Because these patients usually present acutely, their symptoms are frequently initially global and not always specific (Table 3.1).
Table 3.1 Specific injury histories | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Patients who report shoulder instability should be questioned regarding the mechanism of the initial injury and subsequent subluxation or dislocation episodes, the frequency of instability, and the manner in which the shoulder was reduced (i.e., in the emergency department).
The physician should inquire about previous shoulder injuries or prior shoulder surgery because this information may clarify the current symptoms. In addition, the type and outcome of previous interventions such as injections, physical therapy, or surgery assist in determining a diagnosis and formulating a treatment plan.
Finally, a brief medical history should be documented. Previous injuries of the cervical spine or associated neurologic problems may mimic shoulder pathology. Psoriasis may be a precursor to psoriatic spondyloarthropathy involving the shoulder, and diabetes mellitus predisposes patients to development of adhesive capsulitis. Brachial neuritis often manifests first with shoulder pain after a viral illness or unrelated previous surgical procedure. Generalized muscular dystrophy, especially fascioscapularhumeral dystrophy, can manifest with painful shoulder dysfunction before the onset of weakness.
General Physical Examination
Physical examination of the shoulder is performed in a systemic fashion and should be carried out on both shoulders using the patient’s uninvolved shoulder as a control. The examination begins with inspection of the shoulder girdle and is followed by palpation of the anatomic structures and assessment of range of motion, both active and passive. The examination is completed with a series of provocative maneuvers. Each of these segments of the examination should also be performed systematically to ensure that subtle abnormalities are not overlooked. In addition, the examiner becomes increasingly comfortable with normal and abnormal findings with each examination. The examination is then documented in an organized manner so that the history and physical examination can be synthesized to arrive at a final diagnosis.
Inspection
One of the most important, yet frequently unappreciated, aspects of the physical examination is the visual inspection. The inspection should begin as soon as the patient interview begins. Attention to the patient’s use of the shoulder when moving about the examination room before the formal examination begins may give the examiner clues into the problem. One of the more telling clues is noted when the patient protects the shoulder when removing a shirt, sling, or other protective device.
On formal inspection, the examiner looks for general asymmetry between the two shoulders. Asymmetry may be the result of muscle wasting, trauma, swelling, degenerative joint disease, or extrinsic disorders such as scoliosis or hemiplegia. It is important to examine the anterior, lateral, and posterior aspects of the shoulder because each of these areas may reveal pathologic information.
Anteriorly, the clavicle and the sternoclavicular and AC joints are the most prominent structures because their subcutaneous location makes abnormalities fairly easy to detect (Fig. 3.1). Asymmetry in the anterior axillary region is more difficult to detect but should not be overlooked because this area may reveal a deficiency to suggest a pectoralis major avulsion (Fig. 3.2) or other injury. Laterally, the most common asymmetry is noted in the deltoid, which may reveal wasting from axillary nerve palsy or from previous surgery, resulting in deltoid avulsion from the acromion (Fig. 3.3). Inferior subluxation of the glenohumeral articulation (sulcus sign) is an indicator of multidirectional instability (Fig. 3.4). Poste
riorly, wasting of the rotator cuff muscles in the supraspinatus and infraspinatus fossa may be dramatic (Fig. 3.5). Wasting may be secondary to disuse atrophy seen in glenohumeral arthritis or in chronic rotator cuff tears or in primary neurologic causes such as suprascapular nerve palsy (Fig. 3.6). More isolated areas of atrophy, including periscapular musculature, may indicate involvement of extrinsic causes such as brachial plexus neuropathy. Patterns of muscle wasting with primary muscular dystrophy are specific, especially in fascioscapularhumeral dystrophy, and it is not unusual for the orthopaedic surgeon to be the first to make this diagnosis in the patient with shoulder pain.
riorly, wasting of the rotator cuff muscles in the supraspinatus and infraspinatus fossa may be dramatic (Fig. 3.5). Wasting may be secondary to disuse atrophy seen in glenohumeral arthritis or in chronic rotator cuff tears or in primary neurologic causes such as suprascapular nerve palsy (Fig. 3.6). More isolated areas of atrophy, including periscapular musculature, may indicate involvement of extrinsic causes such as brachial plexus neuropathy. Patterns of muscle wasting with primary muscular dystrophy are specific, especially in fascioscapularhumeral dystrophy, and it is not unusual for the orthopaedic surgeon to be the first to make this diagnosis in the patient with shoulder pain.
 Figure 3.3 Avulsed deltoid origin related to previous deltoid detachment performed during routine rotator cuff repair. |
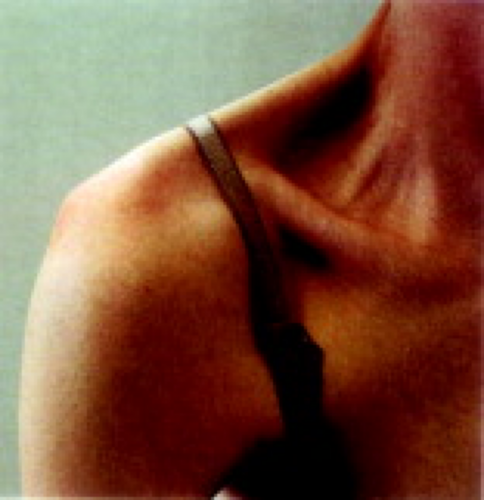 Figure 3.4 Sulcus sign of the right shoulder in a patient with multidirectional instability. Note the sulcus inferior to the prominent lateral acromion. |
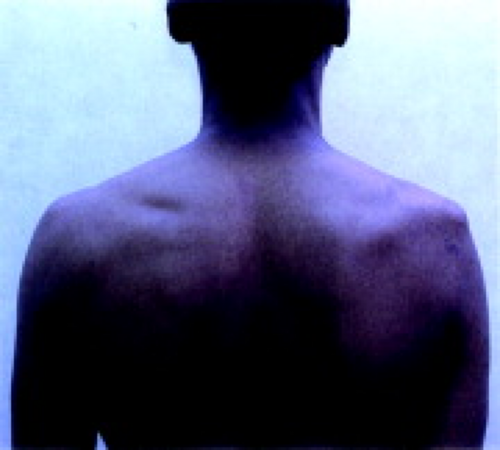 Figure 3.5 Supraspinatus and infraspinatus wasting resulting from degenerative disease of the right shoulder. |
Palpation/Crepitus/Rent
Palpation of the shoulder is used to identify defects, prominences, or pain in the bone and soft tissue structures of the shoulder. The examination begins with palpation of the bones and articulations, beginning with the sternoclavicular joint, where anterior or posterior dislocations and degenerative changes may occur. Palpation continues laterally along the clavicle to the AC joint. A painful AC joint may indicate an arthritic or traumatized joint. Shoulder separation is noted by the painful prominence of the distal end of the clavicle associated with hypermobility of the AC joint. Palpation is continued along the acromion and scapular spine. Finally, palpation of the proximal humerus and tuberosities is carried out, eliciting pain from fractures.
Palpation of the soft tissues is performed subsequently. This begins with palpation of the axilla to assess the pectoralis major anteriorly for ruptures. The pectoralis major may be made more prominent by having patients place their hands on their hips and press medially. The posterior boundary of the axilla is defined by the latissimus dorsi. Palpation of the deltoid is then performed with the examiner being sure to palpate the anterior, middle, and posterior thirds of the muscle. This examination confirms findings of atrophy or injury noted on previous inspection.
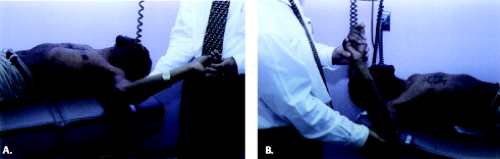
Palpation of the rotator cuff is helpful in diagnosing rotator cuff disease, but it also is more difficult to perform. It is most easily executed by placing the examiner’s fingers on the anterolateral aspect of the acromion with
the palm of the hand resting posteriorly. The examiner’s fingers then palpate in the interval between the anterior and middle thirds of the deltoid (Fig. 3.7). Palpation reveals tenderness in an inflamed bursa, rotator cuff, or biceps tendon. Experienced examiners may be able to palpate a defect in the rotator cuff resulting from rotator cuff rupture or biceps dislocation or a prominence caused by calcific deposit. The examination is rendered more effective by extending the shoulder in neutral abduction to expose the tuberosities, intertubercular groove, and supraspinatus tendon anterior to the acromion. Because rotator cuff disease occurs primarily at the anterior aspect of the supraspinatus, palpation just off of the anterolateral corner of the acromion yields the most effective examination.
the palm of the hand resting posteriorly. The examiner’s fingers then palpate in the interval between the anterior and middle thirds of the deltoid (Fig. 3.7). Palpation reveals tenderness in an inflamed bursa, rotator cuff, or biceps tendon. Experienced examiners may be able to palpate a defect in the rotator cuff resulting from rotator cuff rupture or biceps dislocation or a prominence caused by calcific deposit. The examination is rendered more effective by extending the shoulder in neutral abduction to expose the tuberosities, intertubercular groove, and supraspinatus tendon anterior to the acromion. Because rotator cuff disease occurs primarily at the anterior aspect of the supraspinatus, palpation just off of the anterolateral corner of the acromion yields the most effective examination.
Anteromedial to the supraspinatus attachment to the greater tuberosity, the biceps tendon is located in the bicipital groove. It can be found most easily by palpating anteriorly on the humeral head with the arm in approximately 10 degrees of internal rotation. If in doubt about the location of the biceps tendon, the examiner can follow the easily visualized distal biceps proximally. Rotation of the humerus with the examiner’s fingers over the region of the intertubercular groove assists in detecting the bicipital groove. It is important not to palpate the biceps too vigorously because a normal biceps tendon is tender when palpated forcefully, resulting in a false-positive result. Examination of the contralateral shoulder confirms the sensitivity of the biceps.
Crepitus is a nonspecific sign on physical examination because it may represent rotator cuff disease, intra-articular pathology such as labral tears or degenerative arthritis, or scapulothoracic bursitis. With experience, the origin of crepitus may be more easily determined. Crepitus is identified when the examiner’s hand rests over the region of the acromion and deltoid. Crepitus from an irregular bursa/rotator cuff articulating with a roughened undersurface of the acromion and coracoacromial ligament is best noted by bringing the patient’s arm into approximately 60 to 90 degrees of forward elevation and rotating the arm internally and externally. Crepitus from an arthritic glenohumeral joint is noted by passive motion of the glenohumeral joint with the arm in neutral abduction, again rotating the arm internally and externally. Crepitus from the scapulothoracic articulation is noted posteriorly with full elevation of the upper extremity.
Range of Motion—Active/Passive
The evaluation of both active and passive range of motion is important in the complete physical examination of the shoulder. Active range of motion is tested first and identifies the functional limitations of motion. Limitations of shoulder motion may be the result of true mechanical or static restrictions such as adhesive capsulitis (soft tissue contracture) or degenerative joint disease (bony obstruction), or it may be the result of dynamic loss as is seen in patients with large rotator cuff tears or neurologic deficiencies. Limitations in motion may be voluntary or involuntary, depending on pain related to the underlying condition.
The Society of American Shoulder and Elbow Surgeons has recommended that the evaluation of active range-of-motion tests of the shoulder should include an assessment of forward elevation, external rotation at neutral and 90 degrees of abduction, and internal rotation (19). All tests are performed preferably with the patient standing, because this position keeps the
examining table from interfering with the examination. In addition, both shoulders are examined simultaneously (except for internal rotation), allowing for the patient’s contralateral shoulder to serve as a control.
examining table from interfering with the examination. In addition, both shoulders are examined simultaneously (except for internal rotation), allowing for the patient’s contralateral shoulder to serve as a control.
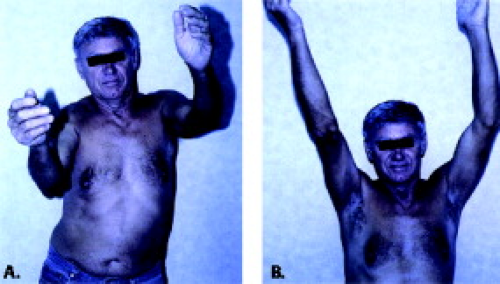
Forward elevation is an examination of the patient’s ability to raise his or her arm maximally in the plane of scapular motion, located between the sagittal and coronal planes (Fig. 3.8). Because two thirds of the overall shoulder range of motion occurs at the glenohumeral articulation and one third occurs at the scapulothoracic articulation (20), this examination evaluates the patient’s true functional range of motion in overhead reaching ability. Limitations in glenohumeral range of motion can be determined by careful examination of the scapulothoracic rhythm and range. If limitations or an abnormal motion exists, the patient should be observed both anteriorly and posteriorly to determine which articulation is abnormal. A common finding in patients with a weak or painful shoulder is “hiking,” which is a pathologic shoulder rhythm in which elevation or rotation of the scapula precedes glenohumeral abduction in an effort to maximize total elevation of the extremity (Fig. 3.9).
 Figure 3.8 Total active forward elevation is measured as maximal elevation performed with the humerus in the scapular plane located between the sagittal and coronal planes. |
External rotation is performed with the patient’s elbow flexed at 90 degrees and the elbow located at the patient’s side. The patient then rotates his or her forearm externally while maintaining a vertical humerus and a flexed elbow (Fig. 3.10). Neutral rotation is defined when the forearm is directly anterior, that is, in the sagittal plane, and 90 degrees external rotation is noted when the forearm is rotated directly laterally in the coronal plane.
Internal rotation is evaluated by instructing patients to place their hand behind their back and reach their thumb as high as possible. This examination is not performed simultaneously but rather sequentially to minimize interference between the two extremities. The maximum height that the patient is able to reach the thumb is documented by the anatomic level, for instance, the iliac crest, lumbar spine, or thoracolumbar junction (Fig. 3.11).
 Figure 3.11 Internal rotation is documented as the maximum cephalad position the patient can reach with the extended thumb. |
Measurements of passive range of motion are performed when limitations in active motion are noted. An increase seen in passive range of motion over that noted
in active range of motion suggests a functional cause for motion loss. The most common diagnosis resulting in this discrepancy is large and massive rotator cuff tears, although neurologic causes may result in a similar clinical picture (Fig. 3.12). Passive range of motion may be performed with the patient supine to increase patient comfort.
in active range of motion suggests a functional cause for motion loss. The most common diagnosis resulting in this discrepancy is large and massive rotator cuff tears, although neurologic causes may result in a similar clinical picture (Fig. 3.12). Passive range of motion may be performed with the patient supine to increase patient comfort.
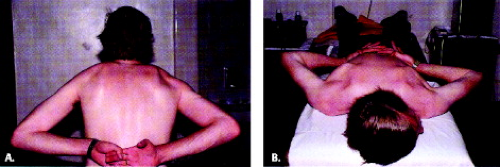
Determination of the subtle loss in range of motion is essential in the throwing athlete because contractures frequently limit internal rotation and horizontal adduction in this patient population. These alterations in the normal mechanics of the shoulder, if not addressed, may result in increased stresses on the anterior capsule and secondarily on the elbow. Subtle restrictions of passive motion again can be detected by measuring internal and external rotation of the shoulder with the humerus abducted 90 degrees and the scapula stabilized by the examiner’s hand (Fig. 3.13). Alternatively, internal rotation loss can be quickly detected (but not quantitatively measured) by observing scapular winging on standing or prone patients with their hands clasped behind their back (Fig. 3.14). An external rotation contracture (limited internal rotation) is frequently noted (Fig. 3.15).