History
Evaluation of the painful wrist and hand begins with a thorough history and physical examination, with the history alone often leading the physician to the diagnosis, whereas the examination serves as a confirmation. The history begins consistently with a review of demographics relevant to use of the hand, specifically age, sex, handedness, and occupation. The nature of the primary symptom is then ascertained with evaluation of character, location, onset, timing, and alleviating and aggravating factors. It is often helpful to have the patient point with one finger to the specific location of maximum symptomatology. Any pain should be evaluated through an analog scale to aid later comparisons. Associated symptoms may include paresthesias or numbness, weakness, color or temperature changes, snapping, popping, and decrease in coordination. Details are obtained regarding the mechanism of onset, including any history of trauma, change in activity levels or overuse, prior injury, and prior treatment.
A complete medical and surgical history with a full review of systems should be obtained at the first encounter and updated at each subsequent visit. Diabetes, vascular, cardiac, pulmonary, and renal dysfunction can all play a role in hand conditions, and any rheumatologic or dermatologic conditions should be noted. Social history involves smoking, alcohol and substance abuse, HIV and/or hepatitis status, and any hobbies or sports in addition to the basic demographic information listed previously. Family history may be relevant in many nontraumatic conditions.
After this initial survey of the history and character of the symptoms, most problems will easily stratify into one of four groups: acute traumatic, acute nontraumatic, chronic posttraumatic, and chronic nontraumatic (Table 14.1). Some patients may have sustained a past trauma, which was felt to be insignificant at the time but led to delayed symptoms (i.e., an undiagnosed scapholunate sprain leading to later degenerative changes). However, initial examination and imaging will often reveal signs of a past trauma and help to place the patient into one of the four groups. This process of stratification leads the examiner to additional relevant aspects of the history, guides the physical examination, and helps to narrow the differential diagnosis.
Table 14.1. Differential diagnosis of hand and wrist pain | ||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||
Physical Examination
Once the history has been taken, the physical examination serves to confirm or refute the physician’s initial impression. A systematically performed examination of the neck and entire upper extremity will allow for precise localization of symptoms and any functional deficits of the wrist or hand while revealing any proximal or systemic causes that might be overlooked in an overly focused examination. By establishing a routine order of examination, the entire extremity can be evaluated in a thorough yet efficient manner. The examination proceeds through inspection, sensibility testing, range of motion, palpation and instability examination, grading of motor function, and finally provocative maneuvers so that trust between the patient and physician can be gradually established while potentially painful maneuvers are saved for the end of the examination. Comparison to the contralateral extremity is often helpful in detecting subtle changes from normal.
Inspection begins with a general review of the patient, ascertaining physiological age, general health status and mobility, posture, and gait. The skin of the hands is evaluated for any wounds, erythema, rashes, or swelling. Skin color, temperature, trophic changes, and rapidity of capillary refill may reveal problems with vascular perfusion. Muscular atrophy may be readily apparent on inspection. Alteration in the resting position of the wrist or normal cascade of the digits can be an indirect sign of tendon dysfunction or injury. One should note the location of any old scars or previous incisions.
In the office setting, sensibility is tested by moving light touch, pin prick, and two-point discrimination. The median nerve is tested at the volar tip of the index finger, whereas the ulnar nerve is tested at the volar tip of the small finger. The radial nerve is tested at the dorsal first web space. Bilateral symptoms or symptoms not conforming to typical peripheral nerve distributions should prompt a search for a more proximal nerve compression or injury at the brachial plexus or cervical root level.
Active and passive ranges of motion of the upper extremities are then evaluated. First the patient performs neck flexion, extension, and lateral rotation with the neck extended as a quick screen for cervical root compression. Any pain or decreased range of motion noted when the patient raises his or her arms straight up and then places his or her hands behind his or her head and then behind his or her back can reveal shoulder pathology that may play a part in the patient’s pain. Elbow motion is tested in flexion and extension. Forearm pronation and supination is an essential part of wrist evaluation that is often neglected. The wrist is tested in flexion, extension, radial deviation, and ulnar deviation and fingers are tested through flexion and extension at each joint. Ranges are compared with the opposite extremity. Differences between active and passive range are of particular importance. Take note of any sounds produced by range of motion, including crepitance, snapping of tendons, or the clunking of carpal instability.
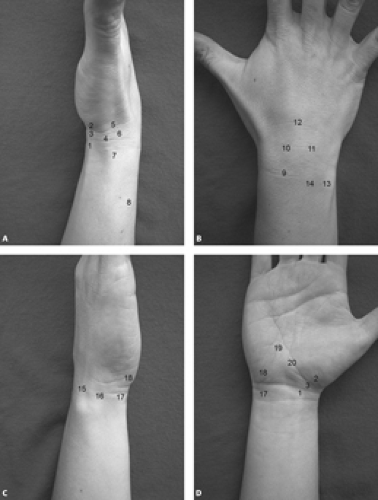
As a result of the compact anatomy of the hand and wrist, palpation should be performed very precisely and systematically to match areas of tenderness to specific anatomic structures. The size, contour, and mobility of any masses can be appreciated and differentiated from areas of edema, tenosynovitis, or fluctuance. It is helpful to palpate the joints of each finger and to stress the joints if instability is a concern. Examine the flexor and extensor mechanisms of each digit for tenderness or subluxation. The wrist is best divided into four zones for a complete evaluation. A stepwise examination of each zone can ensure that all relevant structures have been examined and remind the examiner of the differential diagnosis during the process (Fig. 14.1).
Palpation of the radial aspect of the wrist proceeds from the volar aspect around to the dorsal side. The flexor carpi radialis (FCR) is easily traced distally from the forearm and is tender in FCR tendonitis. At its distal extent, the trapezial ridge is palpable and is tender in trapeziometacarpal arthritis. Just proximal to the trapezial ridge is the distal pole of the scaphoid, which is most prominent during radial deviation. A mass proximal to this may represent a volar ganglion cyst or radial artery aneurysm. The abductor pollicis longus (APL) and extensor pollicis brevis (EPB) of the first extensor compartment are identified at the base of the thumb metacarpal and are tender as they pass over the radial styloid in DeQuervain’s tenosynovitis. Dorsal to the EPB within the distal aspect of the “anatomic snuffbox” one can palpate the dorsal aspect of the trapeziometacarpal joint. Just proximal to this is the scaphoid waist, and any tenderness here should elicit suspicion for a scaphoid fracture, even if initial radiographs are negative. The next most proximal structure is the radial styloid, which will be tender if fractured, followed by the crossing of the APL and EPB over the radial wrist extensor tendons of the second extensor compartment. Tendonitis here is known as “intersection syndrome” (1).
Proceeding to the dorsal zone of the wrist, the extensor pollicis longus (EPL) is palpable as it curves around Lister’s tubercle, a bony prominence on the dorsal distal radius. This is a common site of tendon rupture as a sequelae of distal radius fracture (2). One centimeter distal to Lister’s tubercle is the scapholunate joint, the most common site of intercarpal ligament injuries and a common site of ganglion cysts (3). Dorsal ganglia may become more prominent with flexion of the wrist or may remain occult. With the wrist flexed, the proximal pole of the scaphoid is easily felt to the radial side and the lunate is felt to the ulnar side. Lunate tenderness may raise suspicion of Kienböck’s avascular necrosis of this bone. The finger extensors may be tender as they emerge from under the extensor retinaculum in tenosynovitis secondary to overuse or rheumatoid arthritis. Distally, the bony ridge of the second through fifth carpometacarpal (CMC) joints may be tender in acute fractures or dislocations or in degenerative arthritis (CMC bossing).
Palpation of the ulnar side of the wrist proceeds from dorsal to volar. The most prominent feature of the dorsal ulnar side of the wrist is the ulnar head. Just radial to this one can palpate the distal radioulnar joint (DRUJ). By stabilizing the radius and translating the distal ulna in the dorsal–volar plane, one can determine whether any pathologic instability exists, indicating ligament injury or disruption. Comparison to the contralateral wrist is usually necessary. This maneuver should be repeated in full pronation, neutral rotation, and full supination to fully assess for instability. One centimeter distal to the DRUJ, the lunotriquetral joint is palpable and is another potential site of intercarpal injury and instability. Translation of the triquetrum relative to the lunate is known as the lunotriquetral ballottement test and is a sign of instability (4). Just distal to this joint, the dorsal aspect of the hamate is palpable and is a potential site of avulsion fractures seen in association with CMC dorsal dislocation. The extensor carpi ulnaris (ECU) is the next most ulnar structure and should be palpated along its length for tenderness indicating tendonitis and for subluxation during active wrist supination and flexion. Just volar to the ECU, the ulnar styloid is prominent within the “ulnar snuffbox” between
the ECU and flexor carpi ulnaris (FCU). This may be tender in acute fracture or nonunion. The triangular fibrocartilage complex (TFCC) is a structure analogous to the meniscus of the knee and may be palpated distal to the ulnar head and styloid on both sides of the ECU. Tenderness here may indicate a tear in the setting of an acute injury or may indicate degeneration of this structure secondary to impingement between the lunate and a prominent ulnar head (ulnar impaction syndrome) (5). The FCU may be traced distally from the forearm to its insertion on the pisiform at the base of the hypothenar eminence. Tenderness here may indicate FCU tendonitis or pisotriquetral arthritis. Arthritis is distinguished from tendonitis by pain and crepitance with ballottement or radioulnar translation of the pisiform over the triquetrum. The ulnar artery and nerve curve around the radial aspect of the pisiform. A pulsatile mass could indicate an aneurysm of the ulnar artery, and tenderness in association with paresthesias or numbness of the ulnar two digits can point to entrapment of the ulnar nerve within Guyon’s canal. Distal and radial to the pisiform and in line with the ring finger, the hook of the hamate can be palpated. Tenderness here, especially after a checked golf or baseball swing, may indicate a fracture of the hook.
the ECU and flexor carpi ulnaris (FCU). This may be tender in acute fracture or nonunion. The triangular fibrocartilage complex (TFCC) is a structure analogous to the meniscus of the knee and may be palpated distal to the ulnar head and styloid on both sides of the ECU. Tenderness here may indicate a tear in the setting of an acute injury or may indicate degeneration of this structure secondary to impingement between the lunate and a prominent ulnar head (ulnar impaction syndrome) (5). The FCU may be traced distally from the forearm to its insertion on the pisiform at the base of the hypothenar eminence. Tenderness here may indicate FCU tendonitis or pisotriquetral arthritis. Arthritis is distinguished from tendonitis by pain and crepitance with ballottement or radioulnar translation of the pisiform over the triquetrum. The ulnar artery and nerve curve around the radial aspect of the pisiform. A pulsatile mass could indicate an aneurysm of the ulnar artery, and tenderness in association with paresthesias or numbness of the ulnar two digits can point to entrapment of the ulnar nerve within Guyon’s canal. Distal and radial to the pisiform and in line with the ring finger, the hook of the hamate can be palpated. Tenderness here, especially after a checked golf or baseball swing, may indicate a fracture of the hook.
The last zone to examine is the palmar zone, which includes the digital flexors and the median nerve as they pass through the carpal canal. Tenderness over the transverse carpal ligament, which runs between the trapezium radially and the hamate hook and pisiform ulnarly, may indicate compression of the median nerve in carpal tunnel syndrome or tenosynovitis of the flexor tendons from overuse or rheumatoid arthritis, which frequently leads to secondary carpal tunnel syndrome. Reproduction of paresthesias into the median nerve distribution with a gentle tapping (Tinel’s sign), direct pressure (carpal compression test), or wrist flexion for up to 30 seconds (Phalen’s test) is indicative of median nerve dysfunction secondary to entrapment, especially if all three tests are positive (6).
Muscle groups of the hand and wrist can be divided based on whether the muscle originates purely within the hand (intrinsic) or from the elbow or forearm (extrinsic). Additionally, they can be divided by the peripheral nerve, which innervates them. Median nerve extrinsic function can be tested by resisted proximal interphalangeal (PIP) flexion (flexor digitorum superficialis), digital interphalangeal (DIP) flexion of the index and long fingers (flexor digitorum profundus), thumb interphalangeal (IP) flexion (flexor pollicis longus), and wrist flexion with radial deviation (flexor carpi radialis). Median nerve intrinsic function can be tested by placing the thumb into opposition and having the patient resist pressure on the thumb from one of the examiner’s fingers as another palpates the opponens muscle for tone. Ulnar extrinsic function is tested through resisted DIP flexion of the ring and small fingers, whereas intrinsic function is tested by placing the index finger into abduction and having the patient resist an adduction force on the index finger from one of the examiner’s fingers as another palpates the tone of the first dorsal interosseous muscle. The radial nerve does not innervate any intrinsic muscles; therefore, its function is tested by resisted extension of the wrist and the metacarpophalangeal (MCP) joints. The examiner should be aware that extension of the IP joints can occur through the ulnar nerve-innervated intrinsic muscles even in the total absence of radial nerve function. Finally, objective strength measurements can be obtained through commercially available grip and pinch dynamometers.
By this point in the examination, the physician has evaluated the integrity of the skin and vascularity with inspection; the bony and ligamentous structures with range of motion tests and palpation; the sensory nerves with sensibility tests; and the motor nerves, muscles, and tendons with manual motor tests. Finally, there are a number of provocative maneuvers that attempt to isolate and stress specific areas of the hand and wrist confirm or refute the suspected diagnosis. These are discussed individually as each disorder is reviewed throughout the Chapter.
Evaluation of Specific Disorders
Acute Traumatic Disorders
General Approach
The general trauma history focuses on any pre-existing injuries and the exact mechanism of the trauma, including the position of the hand at the time of injury and direction of force applied; whether any wounds are the result of penetrating, lacerating, or crushing forces; presence of environmental contaminants; and the time of injury. The patient should be asked to localize the site or sites of maximal pain as precisely as possible and to note any associated symptoms such as numbness or instability. Performing a thorough generalized physical examination should reveal any deficits in skin coverage, nerve function, or vascular inflow and outflow. Functional evaluation of bone, ligament, and tendon may require placement of a wrist or digital block with a local anesthetic, but this should only be performed after a complete neurovascular examination has been performed.
Vascular Injuries
History and Examination
Lacerations to arteries and veins are often quite apparent on physical examination alone based on the location of wounds and the presence of bleeding. Do not blindly clamp bleeding structures because of the risk of damaging nearby nerves. Instead, apply direct pressure at or proximal to the site of injury for a short period of time to allow for clotting. Distal perfusion is assessed by the color, capillary refill, and skin turgor of the digits. An Allen’s test can localize an arterial injury in the face of redundant arterial flow by occluding both the radial and ulnar arteries as the patient exsanguinates the hand by making a fist. The hand is opened and pressure is released from one of the vessels. Brisk capillary refill to the hand is a sign that the vessel is patent, whereas persistent pallor indicates lack of blood flow. This test can also be performed in the finger to evaluate the digital arteries (7).
Adjunctive Studies
A crush injury to the hand can be more difficult to assess because the artery may be
ruptured, stretched, and thrombosed or simply in temporary spasm. Even with direct visualization of the vessel, it may be impossible to distinguish thrombosis from spasm or to determine the extent of the zone of injury. Handheld arterial Doppler ultrasound can reveal the presence or absence of arterial blood flow, although retrograde flow can give a false-positive result. Duplex ultrasound can distinguish direction of flow but may not be as readily available. A local anesthetic block may decrease sympathetic tone and vasoconstriction, distinguishing arterial spasm from thrombosis. In rare cases, an arteriogram may be needed to localize the zone of injury and to evaluate perfusion. Magnetic resonance angiography is emerging as a useful noninvasive method for vascular evaluation, but contrast angiography remains the gold standard (7).
ruptured, stretched, and thrombosed or simply in temporary spasm. Even with direct visualization of the vessel, it may be impossible to distinguish thrombosis from spasm or to determine the extent of the zone of injury. Handheld arterial Doppler ultrasound can reveal the presence or absence of arterial blood flow, although retrograde flow can give a false-positive result. Duplex ultrasound can distinguish direction of flow but may not be as readily available. A local anesthetic block may decrease sympathetic tone and vasoconstriction, distinguishing arterial spasm from thrombosis. In rare cases, an arteriogram may be needed to localize the zone of injury and to evaluate perfusion. Magnetic resonance angiography is emerging as a useful noninvasive method for vascular evaluation, but contrast angiography remains the gold standard (7).
Treatment
Once an arterial injury has been identified and localized, it may be treated by ligation, pharmacologic vasodilation or thrombolysis, or operative revascularization depending on the type of injury and status of distal perfusion. Venous insufficiency and congestion, which may follow a crushing injury, will often result in swelling and a dark cyanosis as the lack of venous outflow impedes arterial inflow. This is treated either by restoring outflow through the veins with venous repair or grafting or by providing alternate outflow through heparinized pledgets on the nail bed or the use of medicinal leeches for 5 to 6 days until normal venous flow is restored (8).
Flexor Tendon Ruptures and Lacerations
History
Tendon injuries may occur as a result of a direct laceration to the tendon or from an indirect force leading to rupture or avulsion of the tendon. In either case, it is important to note the specific mechanism of injury. The direction of a penetrating injury can indicate which structures are at risk, whereas a transverse laceration may cause more superficial and predictable injury. If the fingers were flexed around the blade of a knife at the time of injury, then the site of injury on the tendon may move away from the skin wound during an examination with the fingers extended. Closed ruptures may occur from acute traumatic injuries after a period of inflammatory degeneration secondary to overuse, prior injury, or autoimmune conditions. In both ruptures and lacerations, the tendon that has separated from its bony insertion may retract proximally. Physical findings of point tenderness or swelling along the flexor sheath may indicate the site of the retracted tendon stump. The “jersey finger” is a closed rupture or avulsion of the flexor digitorum profundus from the distal phalanx after a forceful hyperextension of a flexed DIP joint, as may happen when tackling by grasping a jersey collar. Spontaneous flexor pollicis longus rupture in patients with rheumatoid arthritis may occur from abrasion against a scaphoid osteophyte (Mannerfelt lesion) (9).
Examination
Loss of the normal digital cascade may be the first sign of tendon injury (Fig. 14.2). After a neurovascular examination, a local anesthetic is given and any wounds are explored remembering that the visible tendon injury may be proximal or distal to the skin wound. Tender or palpable masses may indicate the cut end of a retracted tendon. Loss of isolated active DIP joint flexion indicates a flexor digitorum profundus injury, whereas loss of isolated active PIP flexion indicates a flexor digitorum superficialis injury. Loss of active thumb IP flexion indicates flexor pollicis longus injury.
Adjunctive Studies
Diagnosis of flexor tendon injury is usually made by history and physical examination alone. Plain radiographs may indicate the position of a retracted proximal tendon stump if a fragment of bone has been avulsed with the tendon. Otherwise, ultrasound or MRI may be useful to localize the tendon (10). Frequently, the proximal tendon is located at the time of surgical repair through open exploration of the palm or carpal tunnel. Radiographs or computed tomography (CT) scans may identify a scaphoid osteophyte resulting in flexor pollicis longus rupture.
Treatment
Most acute flexor tendon ruptures and lacerations are treated with open direct repair followed by a closely monitored rehabilitation protocol for protected early motion. Avulsions may require fixation to bone through suture anchors or transosseous sutures. Attritional ruptures may require intercalated tendon grafts or tendon transfers.
Extensor Tendon Ruptures and Lacerations
History and Examination
Injury history is the same as that for flexor tendon injuries. Closed rupture of the terminal extensor tendon’s insertion on the distal phalanx produces a characteristic extensor lag of the DIP joint known as a mallet finger. This is usually the result of a direct axial load to the fingertip. PIP joint hyperflexion may produce avulsion of the central slip from the dorsal base of the middle phalanx. This may not produce an immediate deficit in PIP extension as a result of the intact lateral bands. With time, however, the lateral bands may
subluxate and lead to the characteristic PIP joint flexion and DIP joint hyperextension of the boutonnière deformity. This can be difficult to treat if not immediately recognized; therefore, any tenderness over the central slip insertion after an acute injury should be treated as a presumed avulsion.
subluxate and lead to the characteristic PIP joint flexion and DIP joint hyperextension of the boutonnière deformity. This can be difficult to treat if not immediately recognized; therefore, any tenderness over the central slip insertion after an acute injury should be treated as a presumed avulsion.
Forceful flexion or extension of the finger may lead to rupture of the radial sagittal band, which maintains the alignment of the extensor tendon over the MCP joint. The patient can maintain full MCP extension but cannot initiate it from a flexed position as a result of subluxation of the extensor tendon. Closed rupture of the EPL tendon can occur after distal radius fracture from disruption of the tendon’s vascular supply as it passes around Lister’s tubercle (6). Degeneration from rheumatoid synovitis may also lead to rupture of the EPL or of progressive rupture of the digital extensors beginning ulnarly, like in Vaughn-Jackson syndrome. With each of these conditions, there may be swelling and tenderness at the site of the rupture and loss of IP joint extension after EPL rupture or MCP joint extension after EDC ruptures.
Adjunctive Studies
Plain radiographs may show avulsion fragments in association with the mallet finger or central slip avulsions. CT scans may show distal radius fracture displacement responsible for abrading the EPL. Ultrasound and MRI are rarely used for verifying the diagnosis of extensor tendon rupture, but MRI may provide more anatomic detail regarding the location of the tear and any associated synovitis (10).
Treatment
Some extensor lacerations are treated by direct suture repair. Avulsions may require suture anchors or transosseous suture repairs. Mallet fingers with or without a small associated bony avulsion fragment can be treated with extension splinting alone (11). Large avulsion fragments or subluxation of the joint may necessitate internal fixation. Central slip avulsions are treated with extension splinting of the PIP joint and DIP flexion exercises to prevent lateral band subluxation and shortening, which lead to the boutonnière deformity. Sagittal band rupture is treated with extension splinting at the MCP joint (12). Attritional ruptures of the extensor tendons at the wrist usually are not amenable to direct repair, and tendon transfers are generally used to restore extension to these digits (13).
Fractures
History and Examination
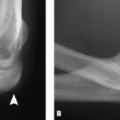
The general trauma history and physical as outlined previously is sufficient to evaluate most fractures of the hand and wrist. The examiner should note any focal tenderness, crepitance, and angular or rotational deformity of the digits (Fig. 14.3). With flexion, each finger should point to the scaphoid tubercle at the base of the thenar eminence and should not significantly overlap the other fingers. In the carpus, fractures are often difficult to visualize on initial radiographs; therefore, any tenderness of the scaphoid should be presumed to be an occult fracture and treated as such until proven otherwise. Similarly, tenderness over the hook of the hamate or the dorsal aspect of the CMC joints should prompt further studies to evaluate these areas for fracture.
Adjunctive Studies
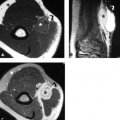
Routine posterior–anterior (PA), lateral, and oblique plain radiographs are sufficient to diagnose and treat most hand and wrist fractures. Traction or postreduction views are best for highly comminuted or displaced fractures. Dorsal fracture–dislocations of the CMC joints are best seen on a supinated oblique view for the index and long metacarpals or a pronated oblique view for the ring and small metacarpals. Hamate hook fractures may be seen on a “carpal tunnel” view looking down the longitudinal axis of a hyperextended wrist; however, CT scans may be more sensitive for visualization of some hook fractures (14). They may also be useful to assess the congruity of the articular surface in any of the intra-articular fracture patterns. Scaphoid fractures are best visualized on either a routine PA, oblique and lateral radiographs or an ulnarly deviated and 45-degree pronated PA view (Fig. 14.4). CT scans can be obtained to look for occult scaphoid fracture or to evaluate the deformity of a fracture seen on radiographs, but an MRI scan is more sensitive than CT scanning in detecting marrow edema and diagnosing an occult fracture or avascular necrosis of the proximal pole (15). A bone scan is also sensitive for detecting occult fractures but gives little information regarding bony architecture.
Treatment
Fracture pattern and injury to the associated surrounding tissues usually dictate treatment. Simple, stable fractures with minimal displacement or stable reductions can usually be treated with splinting or
casting. Displaced and unstable fractures require closed reduction and percutaneous pinning to maintain reduction. Intra-articular phalangeal fractures, proximal phalangeal shaft fractures, oblique metacarpal shaft fractures, CMC dorsal fracture–dislocations, and thumb metacarpal base fractures all typically require reduction and fixation resulting from the deforming forces of the surrounding tendons. Multiple fractures and fractures associated with significant trauma to the soft tissues are indications for open reduction and internal fixation (ORIF) so that early range-of-motion exercises can be started to limit stiffness. Displaced carpal fractures, including the scaphoid, usually require ORIF to reduce articular displacement and minimize the risk of nonunion. There is not a clear consensus on the ideal treatment of distal radius fractures. Closed reduction and casting, pinning, external fixation, and internal plate fixation are all legitimate techniques. A shearing fracture of the articular surface, or Barton’s fracture, is likely to displace unless secured with an internal plate.
casting. Displaced and unstable fractures require closed reduction and percutaneous pinning to maintain reduction. Intra-articular phalangeal fractures, proximal phalangeal shaft fractures, oblique metacarpal shaft fractures, CMC dorsal fracture–dislocations, and thumb metacarpal base fractures all typically require reduction and fixation resulting from the deforming forces of the surrounding tendons. Multiple fractures and fractures associated with significant trauma to the soft tissues are indications for open reduction and internal fixation (ORIF) so that early range-of-motion exercises can be started to limit stiffness. Displaced carpal fractures, including the scaphoid, usually require ORIF to reduce articular displacement and minimize the risk of nonunion. There is not a clear consensus on the ideal treatment of distal radius fractures. Closed reduction and casting, pinning, external fixation, and internal plate fixation are all legitimate techniques. A shearing fracture of the articular surface, or Barton’s fracture, is likely to displace unless secured with an internal plate.
Dislocations and Ligament Injuries
Distal Interphalangeal Joint
History and Examination
As a result of the high level of articular congruity and the relatively small normal arc of motion of the DIP joint, isolated collateral ligament injuries and true dislocations are rare. Avulsions of the terminal extensor tendon and the flexor digitorum profundus (FDP) tendon may be associated with avulsed fragments of the distal phalangeal base, which may destabilize the joint and lead to dorsal or volar subluxation. These conditions have been discussed previously under tendon injuries.
Proximal Interphalangeal Joint
History and Examination
The PIP joint has a large arc of motion and is highly dependent on ligamentous support. It is therefore susceptible to injury from axial, angular, and torsional loads that can damage the collateral ligaments, capsule, volar plate, and the central slip of the extensor mechanism as well as the articular and periarticular bone. The middle phalanx may dislocate volarly or dorsally with or without avulsion of the phalangeal base. Collateral ligament injuries may also be associated with an avulsion fragment but are usually intrasubstance tears (16). The direction of dislocation or instability will usually indicate which structures have been disrupted. Point tenderness can confirm injury to the central slip, collaterals, or volar plate.
Adjunctive Studies
Pre- and postreduction anteroposterior, lateral, and oblique radiographs can identify any associated articular injuries. Comminuted articular fractures may require a CT scan to identify depressed fragments.
Treatment
After initial reduction under digital block, the stability of the joint is assessed. For dorsal dislocations, a stable joint is treated with buddy taping or extension block splinting. Unstable joints may require internal fixation, reattachment of the volar plate, or external fixation. Early range-of-motion exercises are essential to prevent stiffness. For volar dislocations, the central extensor slip is assumed to be disrupted, and the joint is splinted in extension with DIP flexion exercises to prevent subluxation of the lateral bands and development of the boutonnière deformity (12). Isolated collateral ligament injuries can usually be treated with buddy taping and range-of-motion exercises, but significant instability of the index finger radial collateral ligament or thumb interphalangeal joint ulnar collateral ligament may mandate open repair to preserve stability for pinch. Displaced avulsion fragments may require internal fixation. Inability to maintain reduction or avulsion fragments of more than 25% of the joint surface require open treatment (16).
Metacarpophalangeal Joint
History and Examination
Dislocations of the thumb and finger MCP joints are typically dorsal and are secondary to hyperextension forces. They are divided into simple and complex dislocations in which simple dislocations maintain some articular contact and are usually easily reducible, whereas in complex dislocations, the proximal phalanx overrides the metacarpal with complete loss of articular contact. The complex dislocations may have interposition of the volar plate or collateral ligament, which can block closed reduction.
Injuries to the collateral ligaments are unusual other than the thumb ulnar collateral ligament and the index radial collateral resulting from the stresses to which they are subjected with grip and pinch. Ulnar deviation greater than 20 degrees indicates index ulnar collateral ligament rupture, whereas radial deviation laxity greater than 30 degrees indicates rupture of the thumb ulnar collateral ligament (17). A tender mass over the thumb ulnar collateral ligament may represent a Stener lesion, in which the adductor aponeurosis is interposed between the two ends of the collateral ligament, precluding healing (18–20).
Adjunctive Studies
Standard three-view radiographs pre- and postreduction are mandatory, and stress views of the joint may be helpful if the physical examination is equivocal. Arthrograms, ultrasound, and MRI have all been described to identify the presence of a Stener lesion.
Treatment
Closed reduction is performed on simple dislocations. Complex dislocations merit one attempt at closed reduction with the finger in hyperextension, but they usually require open reduction to remove the interposed volar plate. Collateral ligament injuries with minimal laxity may be treated with a period of immobilization, whereas those with laxity greater than 20 degrees for the fingers or 30 degrees for the thumb require open repair.
Carpometacarpal Joint
History and Examination
CMC joint dorsal dislocations can occur secondary to a forceful axial load down the metacarpal. Either the dorsal CMC capsule is disrupted or a fragment is avulsed from the dorsum of a carpal bone. There will be point tenderness and swelling over the CMC joint. The fourth and fifth CMC joints are the most commonly injured (21).
Adjunctive Studies
A three-view radiograph of the hand and a pronated oblique to see the dorsum of the small and ring finger CMC joints or a supinated oblique to view the dorsum of the long and index finger joints is adequate.
Intercarpal Ligaments
Anatomic Considerations
Hyperextension forces may lead to injury to the ligaments between the eight bones of the carpus. Normally, the distal carpal row pushes the scaphoid into flexion and triquetrum into extension, but these forces balance one another through the ligamentous attachments to the lunate. Disruption of the scapholunate ligament (SLIL) allows the triquetrum to pull the lunate into extension. Disruption of the lunotriquetral ligament (LTIL) allows the scaphoid to pull the lunate into flexion (23). High-energy injuries may lead to tears, which progress through the SLIL to the space of Poirer distal to the lunate and back proximally through the LTIL. This can lead to a “perilunate” dislocation of the carpus with the lunate remaining reduced or to a dislocation of the lunate with the carpus remaining in place (24). Disruption of intercarpal ligaments can lead to a midcarpal instability between the proximal and distal carpal rows.
History and Examination
The typical mechanism of injury for SLIL injuries and perilunate and lunate dislocations is a fall or impact that causes hyperextension, ulnar deviation, and supination of the wrist. The patient with an SLIL or LTIL injury may give a history of a minor wrist sprain with persistent dorsal pain. There may be tenderness over the SLIL 1 cm distal to Lister’s tubercle. Applying pressure to the volar scaphoid as the wrist is radially deviated may reveal scaphoid subluxation (25). LTIL injuries will be tender 1 cm distal to the DRUJ and may reveal increased pain with ballottement of the triquetrum relative to the lunate. Carpal dislocations are typically the result of high-energy trauma such as in motor vehicle accidents and will typically present with significant swelling, ecchymosis, and deformity of the wrist. The median nerve may be compressed by a volarly dislocated lunate; therefore, a careful neurovascular examination is a necessity. Midcarpal instability is usually associated with a painful and audible clunk as the distal carpal row subluxes and then reduces back against the proximal row with ulnar deviation of the wrist (26).
Adjunctive Studies
SLIL injuries can be classified as static or dynamic based on plain radiographs. In dynamic injuries, the standard three-view wrist series is normal. A clenched fist or ulnar deviation view, however, will cause the angle between the scaphoid and lunate to increase beyond 60 degrees, indicating excessive flexion of the scaphoid. Static injuries will demonstrate scapholunate interval widening and abnormal scaphoid flexion even without provocative maneuvers. Similarly, partial lunotriquetral injuries may show no change on the normal radiographs, whereas complete injuries will show flexion of both the lunate and scaphoid while the triquetrum extends. Midcarpal instability, in contrast, is often visible as volar flexion of the entire proximal carpal row on routine radiographs (26). Partial intercarpal ligament injuries may not be apparent on either static or dynamic radiographs. In these cases, fluoroscopic examination may reveal abnormal carpal motion. A number of studies have compared the sensitivity and specificity of arthrography versus routine MRI and MR arthrography to detect partial tears (27–29). Similar sensitivity and specificity is noted for arthrography and routine MRI, but MR arthrography may have additional sensitivity and reveal the specific location of any tears. Some surgeons bypass both plain and MR arthrography in favor of diagnostic arthroscopy, which allows for accurate diagnosis and treatment at the same setting.
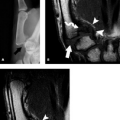
Perilunate and lunate dislocations are often missed initially with the abnormal appearance of the carpus mistakenly attributed to poor radiographic technique. The normal lateral film should show the radius, lunate, and capitate all in line, like stacked cups. In perilunate dislocations, the capitate is displaced dorsally to the lunate and radius, whereas in lunate dislocations, the capitate is in line with the radius while the lunate is displaced and flexed volarly (Fig. 14.5). On PA views, this appears as disruption of the normally smooth contour of the distal edge of the proximal carpal row. Traction views and postreduction views will much more clearly demonstrate the intercarpal injuries along with any associated fractures.
Treatment
SLIL tears seen at arthroscopy but without radiographic instability are débrided and treated with a brief period of immobilization. Tears with dynamic instability are typically treated with open repair and reinforcement of the repair using dorsal wrist capsule to restrict flexion of the scaphoid. Static SLIL instability is treated with ligament repair or arthrodesis of the scaphoid to the capitate or to the trapezoid and trapezium to restrict scaphoid flexion. Interosseous tendon weaves have also been described to stabilize the scaphoid, but both approaches result in abnormal carpal kinematics and loss of wrist range of motion (30).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree