Chapter 3 Clinical Methods
A- and B-Scans
Introduction
Ophthalmic ultrasonography examination techniques are designed to evaluate all aspects of the globe in a methodical, reproducible manner.1–14 The specific type of examination performed is determined by the indication for examination. Contact B-scan and diagnostic A-scan are most commonly used to evaluate the posterior globe and orbit. Anterior ocular structures can be evaluated with a modified immersion B-scan examination, but are most commonly evaluated with ultrasound biomicroscopy (Chapter 4). This chapter describes the proper methods for performing A- and B-scans.
Basic positioning and patient preparation
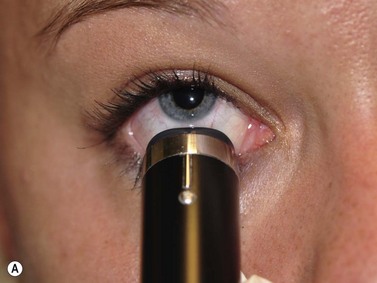
Optimal positioning of the patient and the ultrasound display monitor significantly aids in the ease of obtaining and evaluating captured images. In most cases, scanning the eye with contact B-scan and diagnostic A-scan is most effective if performed with the patient in the reclined position. The ultrasonographer is positioned to the patient’s right or left side at the examiner’s discretion. The ultrasound display monitor and the patient’s head should be located parallel and in close proximity to each other to allow for simultaneous viewing of the ultrasound probe position on the eye and the display monitor (Figure 3.1).
B-scan probe
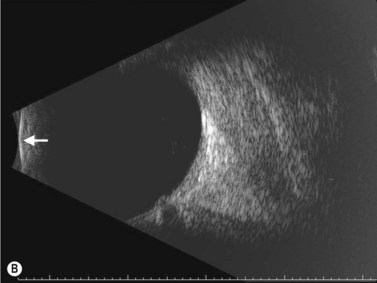
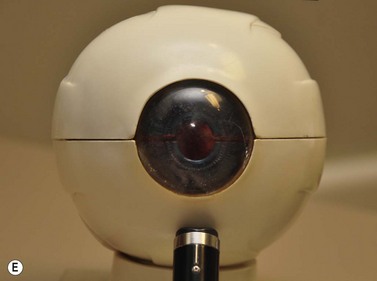
The B-scan probe is a two-dimensional echo display that is used to determine the topographic features of posterior segment pathology including location, shape and extent of lesions (Chapter 2)![]() See Clip 3.1. B-scan probes have a marker along the side of the probe close to the probe tip that indicates the top of the B-scan ultrasound display (Figure 3.2A). The transducer inside the B-scan probe oscillates along the plane of the marker only, towards the marker and away from the marker. Therefore, the top of the B-scan display corresponds to the area indicated on the marker and the bottom of the display corresponds to the plane 180° away from the marker. The probe tip corresponds to the white line on the far left side of the B-scan display. The echoes to the right of this line correspond to the ocular structures opposite the probe tip. The further right the ocular structure, the further away is its echo (Figure 3.2B).
See Clip 3.1. B-scan probes have a marker along the side of the probe close to the probe tip that indicates the top of the B-scan ultrasound display (Figure 3.2A). The transducer inside the B-scan probe oscillates along the plane of the marker only, towards the marker and away from the marker. Therefore, the top of the B-scan display corresponds to the area indicated on the marker and the bottom of the display corresponds to the plane 180° away from the marker. The probe tip corresponds to the white line on the far left side of the B-scan display. The echoes to the right of this line correspond to the ocular structures opposite the probe tip. The further right the ocular structure, the further away is its echo (Figure 3.2B).
B-scan probe positions
Transcorneal scans
Axial scans
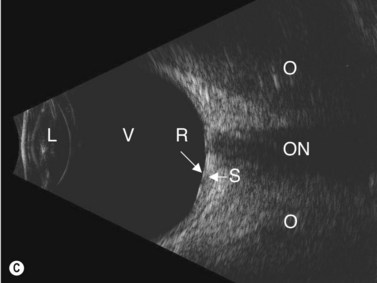
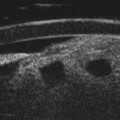
The axial scan is obtained by placing the B-scan probe tip directly over the cornea while the patient looks in primary gaze (Figure 3.3)![]() See Clip 3.2. The resulting image shows the posterior segment of the globe where the marker tip is at the top of the B-scan display, the crystalline lens and the optic nerve in the center and the portion of the globe 180° degrees from the marker at the bottom of the screen. The axial scan is the easiest scan to interpret because the lens and the optic nerve are centered in the image. However, several issues make this scan less than ideal. There is significant sound attenuation and refraction as a result of going through the crystalline lens showing a diminished resolution in the B-scan image. In pseudophakic eyes, the intraocular lens causes intense sound reverberation echoes obstructing most views to the posterior segment. However, the axial scan can be very helpful in the evaluation of some specific disorders affecting the macula (Chapter 10), Tenon’s space (Chapter 12), and the optic nerve (Chapter 13).
See Clip 3.2. The resulting image shows the posterior segment of the globe where the marker tip is at the top of the B-scan display, the crystalline lens and the optic nerve in the center and the portion of the globe 180° degrees from the marker at the bottom of the screen. The axial scan is the easiest scan to interpret because the lens and the optic nerve are centered in the image. However, several issues make this scan less than ideal. There is significant sound attenuation and refraction as a result of going through the crystalline lens showing a diminished resolution in the B-scan image. In pseudophakic eyes, the intraocular lens causes intense sound reverberation echoes obstructing most views to the posterior segment. However, the axial scan can be very helpful in the evaluation of some specific disorders affecting the macula (Chapter 10), Tenon’s space (Chapter 12), and the optic nerve (Chapter 13).
Axial scans are always obtained with the probe marker facing upward or horizontally.12 The vertical axial scan is obtained with the marker in the upright position toward 12 o’clock and the horizontal axial scan is obtained with the marker nasally. For oblique axial scans the probe marker is facing toward the upper of the two meridians being examined.
Para-axial scans
Para-axial scans can be helpful in the evaluation of the peripapillary fundus. The para-axial scan images the fundus directly adjacent to the optic nerve. To obtain the scan, the probe tip is placed directly over the cornea as in the axial scan; however, the sound beam is shifted slightly to the peripapillary area of interest. The sound beam is directed through a portion of the crystalline lens in these scans and some sound attenuation, although not as marked as that occurring with the axial scan, occurs resulting in decreased resolution. Para-axial scans are integral in obtaining accurate dimensions of peripapillary mass lesions (Chapter 11).
Trans-scleral scans
Longitudinal scan
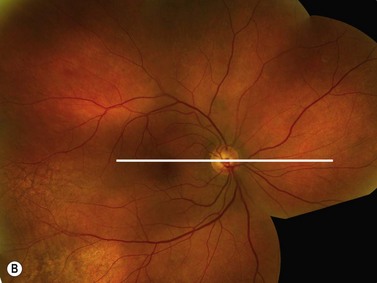
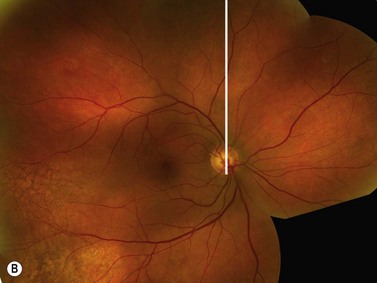
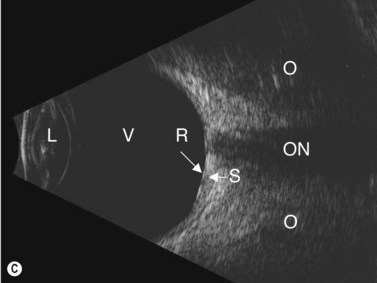
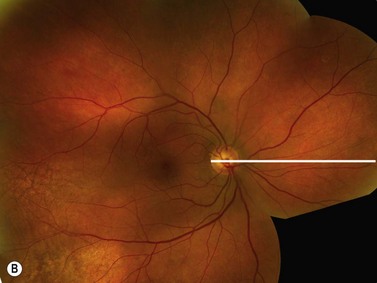
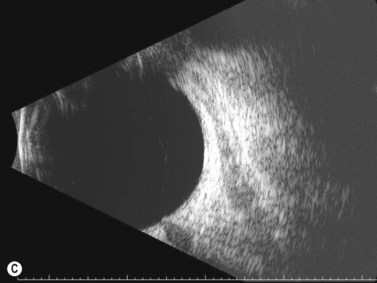
The longitudinal scan is obtained by placing the probe marker in the direction of the clock hour to be imaged (Figure 3.4)![]() See Clip 3.3. The transducer located within the probe moves perpendicular to the limbus, sweeping along the radial plane of the fundus located opposite the probe tip. The resulting image shows the fundus along a specific clock hour. The fundus anterior to the equator is located at the top of the B-scan display, the fundus posterior to the equator is imaged centrally and the optic nerve is located at the bottom of the display. In this manner, the longitudinal scan shows the anterior to posterior extent of posterior segment pathology. The longitudinal scan does not usually require the examiner to actively rotate the probe. However, if the desired area to be examined is in the periphery, it can be helpful to place the probe tip closer to the fornix resulting in an image that demonstrates the peripheral fundus at the top of the display with the optic nerve at the far bottom of the display, or completely absent from the display. The longitudinal scans are labeled according to the clock hour imaged anterior to posterior. If the probe is placed at 9 o’clock with the marker towards the pupil, the transducer sweeps along the 3 o’clock plane (Figure 3.5). The resulting image is labeled as a longitudinal scan of 3 o’clock, or L3.
See Clip 3.3. The transducer located within the probe moves perpendicular to the limbus, sweeping along the radial plane of the fundus located opposite the probe tip. The resulting image shows the fundus along a specific clock hour. The fundus anterior to the equator is located at the top of the B-scan display, the fundus posterior to the equator is imaged centrally and the optic nerve is located at the bottom of the display. In this manner, the longitudinal scan shows the anterior to posterior extent of posterior segment pathology. The longitudinal scan does not usually require the examiner to actively rotate the probe. However, if the desired area to be examined is in the periphery, it can be helpful to place the probe tip closer to the fornix resulting in an image that demonstrates the peripheral fundus at the top of the display with the optic nerve at the far bottom of the display, or completely absent from the display. The longitudinal scans are labeled according to the clock hour imaged anterior to posterior. If the probe is placed at 9 o’clock with the marker towards the pupil, the transducer sweeps along the 3 o’clock plane (Figure 3.5). The resulting image is labeled as a longitudinal scan of 3 o’clock, or L3.
Longitudinal scan is the best orientation to evaluate membranes for insertion into the optic disc or adjacent to the optic disc (Chapter 10). It is also essential in the localization of small fundus abnormalities such as a retinal tear or a focal tractional retinal detachment as well as for the evaluation of the macula described later in this chapter.