Fig. 26.1
“Line of perpendicularity.” This curve demonstrates the average caudal or cranial angulation required across the RAO to LAO spectrum to achieve perpendicularity to the valve plane
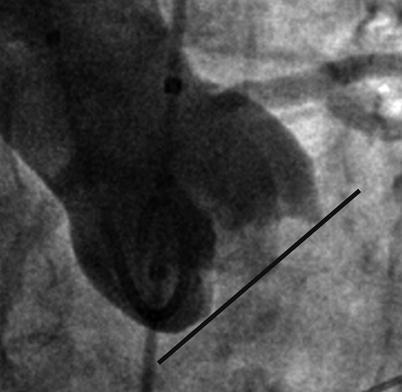
Fig. 26.2
Determination of the correct aortic valve plane. A fluoroscopic projection where the inferior margins of the three sinuses of Valsalva provide a perpendicular view to the aortic valve plane (black line)
Multislice Computed Tomography
Image Acquisition
Multislice computed tomography (MSCT) uses three-dimensional volume-rendered transparent reconstructions of the thoracic aorta. Reconstructions are produced on workstations from double oblique transverse images (Fig. 26.3). Projections perpendicular to the native aortic valve plane are found by placing a point on the inferior most aspect of each aortic valve cusp. From these points, a triangular trace can be created. Particular attention must be paid to determining the most inferior margin of each aortic cusp from the orthogonal projection of the root. If the inferior margin is chosen erroneously for one or more aortic cusps, the valve plane chosen may be incorrect. Angles at present are determined manually by rotating the three-dimensional aortic reconstructions to discern the appropriate projection. An angle is deemed appropriate when the triangle is not evident and is replaced by a line, suggesting that the three placed points are in line. A contrast volume of between 80 and 120 ml is usually required for image acquisition, which includes imaging of the peripheral vasculature.
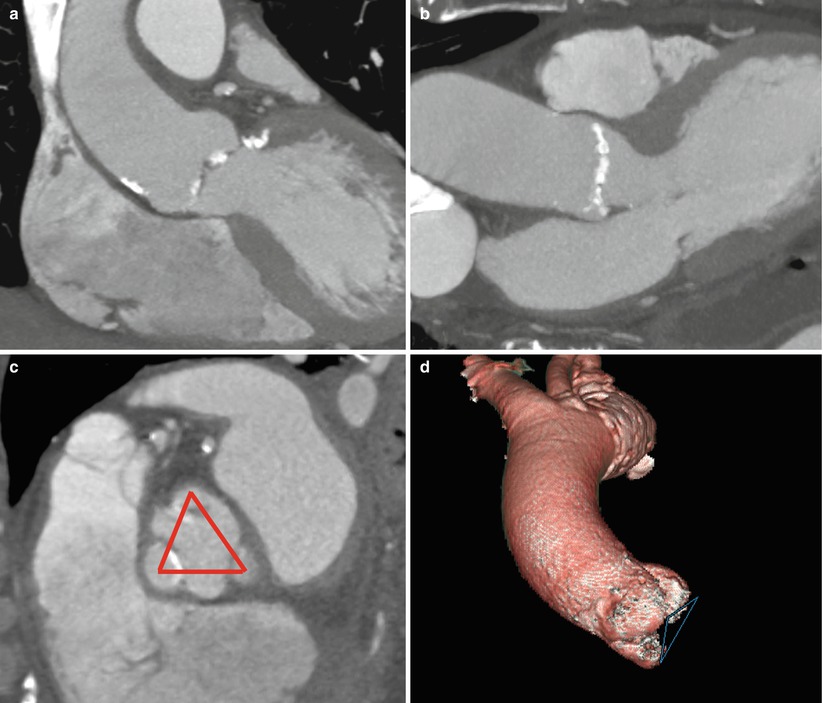
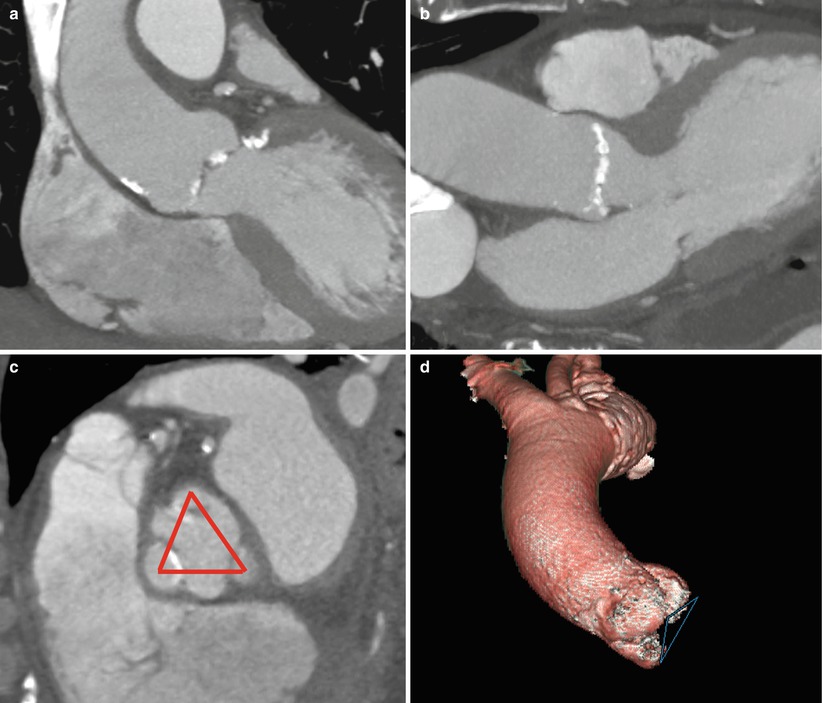
Fig. 26.3
Stepwise approach to construction of a three-dimensional volume-rendered image of the aortic root. The aorta is bisected from a routine coronal projection (a) to create a sagittal oblique multiplanar reformat (b). From the sagittal oblique, an orthogonal projection of the root (c) is acquired using the standard oblique workstation tool. After scrolling to the most inferior margins of the aortic cusps on the orthogonal projection of the root, points are deposited on these most inferior margins and linked in a triangular fashion (d). A three-dimensional volume-rendered image of the ascending aorta is then created with the triangle in place
Predictive Accuracy
Preliminary studies evaluating the ability of MSCT to accurately predict optimal fluoroscopic deployment projections have been promising. Kurra et al. conducted a small prospective study comparing MSCT-generated predictive angles with conventional angiography. The degree of cranial and caudal angulation required to obtain an optimal projection angle in both LAO 40° and RAO 20° projections was assessed using both modalities. A suitable deployment projection could be found in all patients with the use of MSCT and in 38 of 40 patients using conventional angiography. The degree of cranial angulation required in the LAO view was not significantly different between the two modalities (cranial: 25 ± 9 vs. 23 ± 8, p = 0.214). A small but significant difference in the degree of caudal angulation required in the RAO projection was demonstrated between conventional angiography and matched MSCT images (caudal 21 ± 9 vs. 29 ± 10°, p = 0.002), but no post-deployment assessment was made for either modality to determine accuracy.
The accuracy of MSCT compared with conventional angiography in determining optimal angiographic deployment projections has to date only been evaluated in one study [4]. Twenty patients who underwent TAVR with pre-procedural MSCT angle prediction were compared with a proceeding consecutive cohort of 20 patients that underwent TAVR with conventional angiographic angle prediction. Baseline characteristics were well matched in both groups. Post-deployment accuracy of each predicted fluoroscopic projection was classified as excellent, satisfactory, or poor (as defined in Fig. 26.4). When MSCT was used, an excellent or satisfactory final valve implant projection angle was achieved in 18 cases (90 %) versus 13 cases (65 %) when conventional angiography was used. While statistical significance was not achieved (p = 0.06), a strong trend was observed favoring MSCT. Given that both TAVR and the utilization of MSCT to generate predictive angiographic deployment projection are relatively new technologies, larger studies assessing the role of MSCT are yet to be conducted and furthermore, no outcome data is currently available.
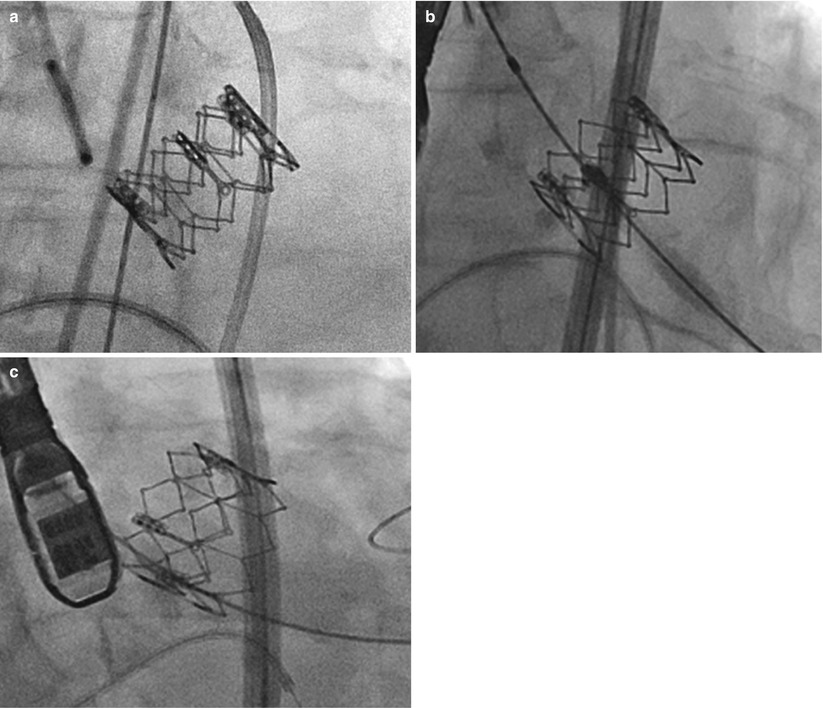
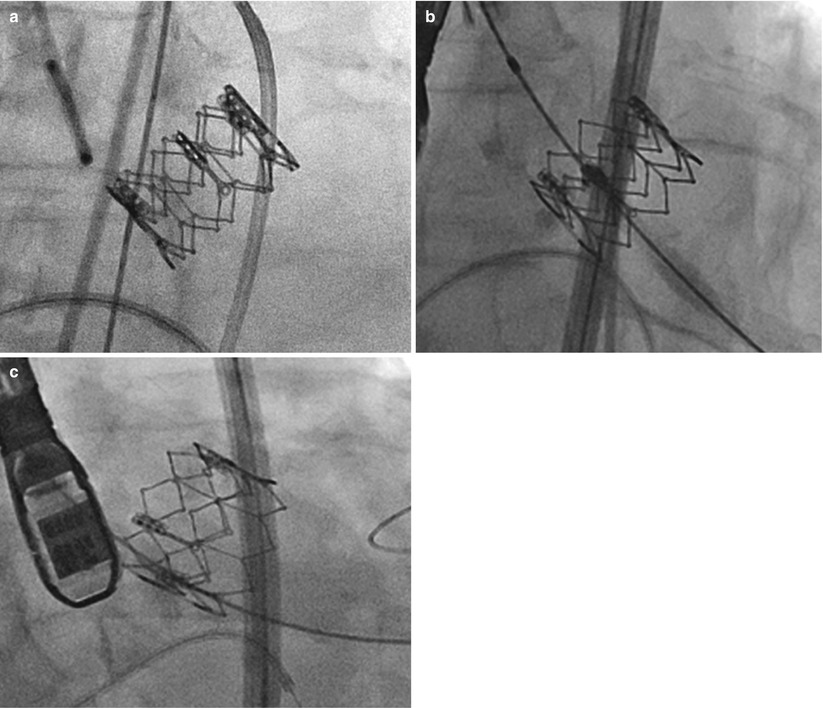
Fig. 26.4
Accuracy of angiographic projection of valve deployment. (a) Excellent—superior struts line up perfectly. (b) Satisfactory—superior valve struts project differently but within the height of a cell. (c) Poor—superior valve struts project in different planes, with a distance greater than the height of a cell
Additional Advantages
The use of MSCT to generated predictive angles offers additional advantages. In TAVR patients, MSCT has a well-established role in pre-procedural assessment and planning [7–11]. MSCT provides detailed assessment of:
Aortic valve characteristics (annulus size, leaflet number, and degree of calcification which can be used in conjugation with echocardiography derived data)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree