Rheumatoid arthritis (RA) is commonly associated with thoracic abnormalities, including interstitial pneumonia and fibrosis (UIP and NSIP are common), pleural effusion or pleural thickening, necrobiotic nodules, OP, bronchiectasis, and bronchiolitis obliterans (
Table 14-1).
Clinical evidence of arthritis precedes the development of pulmonary or pleural disease in about 90% of patients, and 90% have a positive serum rheumatoid factor. Although RA is twice as common in women, extraarticular manifestations of RA, including lung disease, are more common in men. Radiographic findings vary with the manifestation of RA present (see
Table 14-1).
Pleural Disease
Pleural disease, either pleural effusion or pleural thickening, is common in patients with RA being seen in up to 40% of patients at autopsy. However, radiographic evidence of pleural thickening or pleural effusion is present in only 5% to 20% of patients, and it often is asymptomatic. Pleural effusions are usually small and unilateral, being more common on the right. Generally, effusion is not associated with radiographic evidence of lung disease. On HRCT, pleural effusion is visible more often than on radiographs and is seen in more than 40% of patients with findings of interstitial pneumonia.
Interstitial Pneumonia and Fibrosis
Interstitial pneumonia and fibrosis, the most common pulmonary manifestation of RA, is most common in middle-aged men. Dyspnea is common. Histologically, it may represent either NSIP or UIP.
Although pulmonary function abnormalities are present in up to 40% of patients with RA, only about 5% to 10% of patients with RA have radiologically detectable interstitial disease.
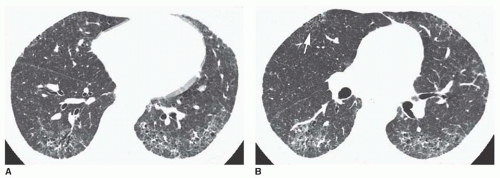
On HRCT, interstitial pneumonia may be associated with a spectrum of abnormalities ranging from ground-glass
opacity to fine reticulation or coarse reticulation with honeycombing. Findings of pulmonary fibrosis (irregular reticulation, traction bronchiectasis, honeycombing) are seen on HRCT in about 10% of patients; ground-glass opacity is seen in 15%.
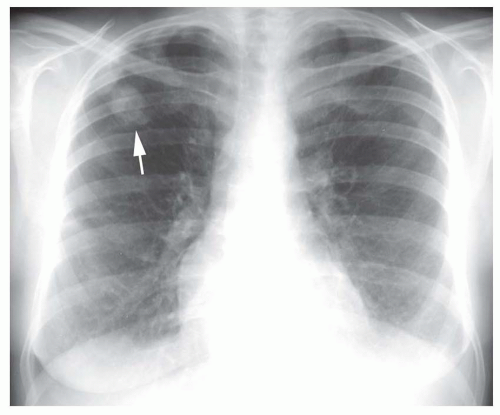
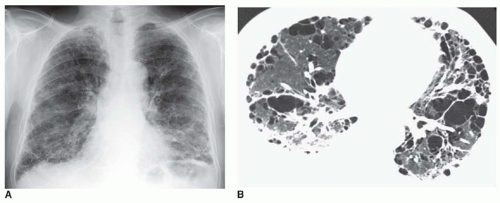
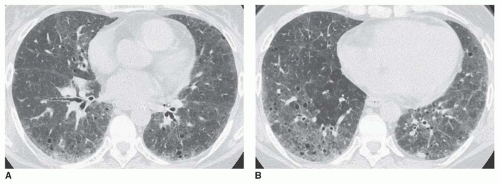
The appearance of RA with interstitial fibrosis may be indistinguishable from that of idiopathic pulmonary fibrosis (IPF) (
Figs. 14-1 and
14-2). However, because some cases are associated with the histologic pattern of NSIP (see
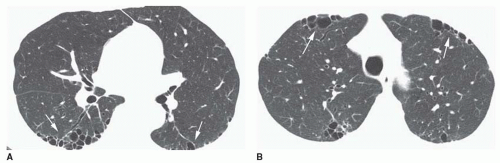
Chapter 13), reticular opacities visible in RA tend to be finer than those seen with IPF (
Figs. 14-3 and
14-4), and honeycombing is less common and less severe. Also, anterior upper lobe honeycombing appears to be more common in the CVD than in IPF (see
Figs. 14-2B and
14-4B). In some patients, this may be a manifestation of LIP rather than UIP or NSIP.
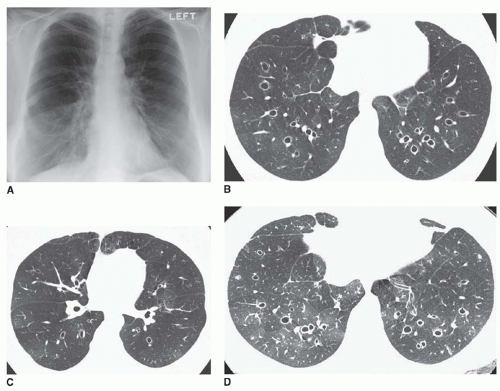
Predominance in the posterior and subpleural lung and at the lung bases is typical of reticular opacities and ground-glass opacity (
Fig. 14-5). Relative sparing of the immediate subpleural lung may be seen, a finding associated with the histologic pattern of NSIP (see
Fig. 14-4).
OP/BOOP may also occur in patients with RA, having typical radiographic and CT features of patchy consolidation or nodules (see
Chapter 13).
Caplan’s Syndrome
Caplan’s syndrome is a rare manifestation of RA occurring in coal miners or patients with occupational exposures to silicates. Nodules are present that resemble necrobiotic nodules histologically but are characterized by concentric layers of light collagen and black dust-laden cells. Caplan’s syndrome is characterized by single or multiple lung nodules ranging from a few millimeters to 5 cm in diameter, similar to rheumatoid nodules. The nodules may cavitate. An upper lobe predominance may be seen, resembling silicosis or coal-worker’s pneumoconiosis, but nodules in Caplan’s syndrome appear rapidly in “crops” in contrary to the slow progression of silicosis.
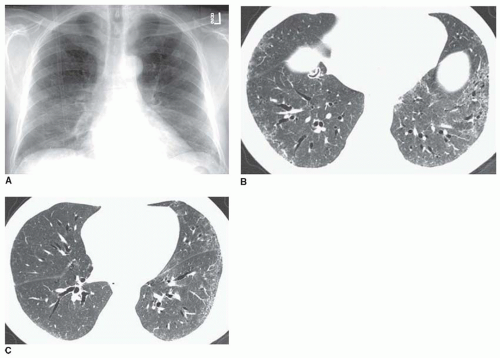
Bronchiectasis
Bronchiectasis is associated with RA, particularly in smokers. It may reflect chronic infection, which has an increased incidence in rheumatoid patients or, associated with i nfection, it may be a factor in the development of RA. Also, bronchiectasis is commonly present in patients with bronchiolitis obliterans (
Fig. 14-7). On CT, it is present in 20% of patients.
Bronchiolitis Obliterans
Bronchiolitis obliterans (see
Chapter 23) is a rare manifestation of RA. Although it is often associated with penicillamine treatment, this is not always the case. Radiographs
are normal or show increased lung volumes. HRCT may show bronchiectasis, mosaic perfusion, and air trapping (see
Fig. 14-7).