and Zdeněk Fryšák1
(1)
Department of Internal Medicine III – Nephrology, Rheumatology and Endocrinology, Faculty of Medicine and Dentistry, Palacky University Olomouc and University Hospital Olomouc, Olomouc, Czech Republic
Keywords
Predominantly solid nodulePredominantly cystic noduleSpongiform noduleCalcificationsAcoustic shadowMicrocalcifications9.1 Complex Nodule with Cystic Degeneration
9.1.1 Essential Facts
Most cystic lesions of the thyroid result from hemorrhage and subsequent degeneration of preexisting solid nodules [1].
In McHenry’ study of 389 patients, cystic nodules were present in 70 (18%) patients. Thyroidectomy was performed in 28 (40%) of them because of an abnormal or persistently nondiagnostic FNAB or compressive symptoms. Six patients (8.6%) had thyroid carcinoma [3].
There is a high risk of false negative results when there is a large complex nodule size (≥4 cm). It is therefore recommended that FNAB be repeated after 6 months even if the result of the first FNAB is negative [2].
According to the 2015 American Thyroid Association (ATA) Guidelines: Isoechoic or hyperechoic solid nodule, or partially cystic nodule with eccentric uniformly solid areas without microcalcifications, irregular margin or extrathyroidal extension, or “taller-than-wide” shape prompts low suspicion for malignancy 5–10% [4].
Spongiform or partially cystic nodules without any of US suspicious features have a low risk of malignancy, <3% [4].
9.1.2 US Features of Complex Nodules with Cystic Degeneration
For classification of predominantly solid nodule (Fig. 9.2), predominantly cystic nodule (Fig. 9.1), spongiform nodule (Fig. 9.3) and US features of complex nodule cystic part; see more in introduction to Section III (part 1.1.2.3) and Chap. 7 (part 7.2).
Spongiform and other mixed cystic solid nodules may exhibit bright reflectors on US imaging, caused by colloid crystals or posterior acoustic enhancement of the back wall of a microcystic area. These may be confused with microcalcifications by less proficient sonographers. Therefore, because of potential misclassification, FNAB may still be considered for nodules interpreted as spongiform, but with a larger cut-off size [5].
9.2 Complex Nodule with Calcifications
9.2.1 Essential Facts
Calcification within the thyroid gland is a common finding on US, with the incidence 14–55% [6].
Histologically, thyroid calcifications are divided into psammomatous (calcium deposits in the epithelium) and dystrophic (amorphous deposits in fibrous tissue) [6].
Calcification can be detected in both benign and malignant nodules, with malignancy rates of 29–59% [6].
Benign nodules have dystrophic coarse calcifications, especially with long disease duration [7].
Peripheral dystrophic calcifications (coarse calcifications shown on US) are more frequently associated with benignity. They can also occur, however, in malignant lesions, up to 18% [6].
Papillary thyroid carcinoma (PTC) frequently forms psammomatous calcification (fine stippled microcalcifications on US) [6, 8]; (Figs. 15.8bb and 15.9bb)
Incidence of dystrophic calcifications is higher in older patients, ≥45 years of age. Fine stippled psammomatous calcifications predict PTC, particularly in younger patients (<45 years). The sensitivity of dystrophic and psammomatous calcification for the detection of malignancy is 63.5% and 24.3%, respectively; the specificity is 69.8% and 96.8% respectively [8].
A risk of malignancy in thyroid nodules with calcifications: punctuate calcifications 23.3%, rim calcifications 16.7%, central coarse calcifications 16.7%, without calcifications 8.5% [9].
9.2.2 Ultrasound Features of Calcifications [1]
Peripheral calcifications are bright echoes observed at the surface of a thyroid nodule.
Calcifications are categorized according to the shape:
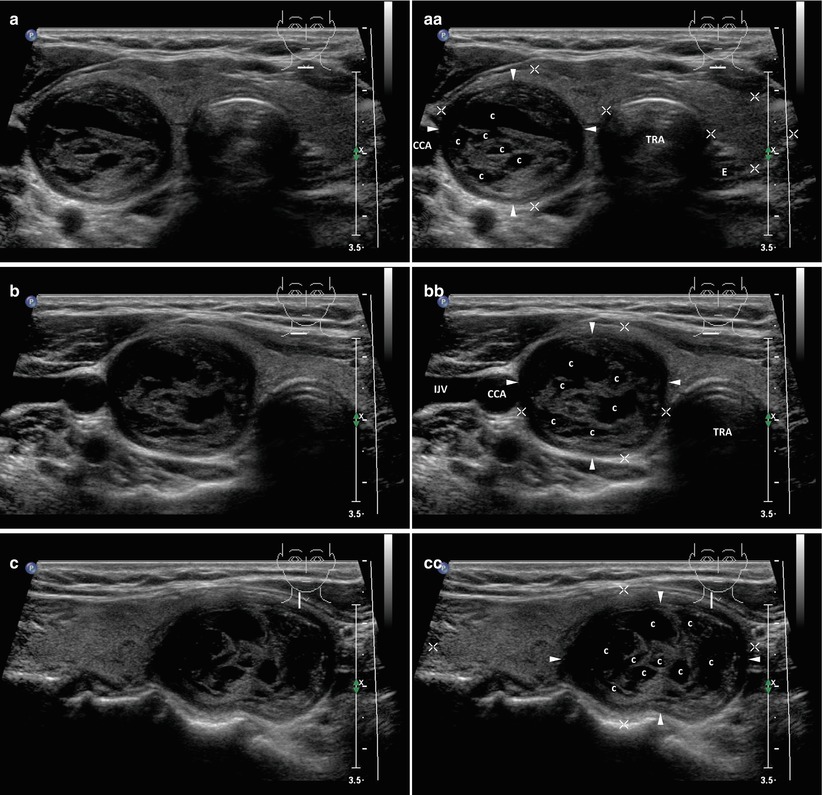
Fig. 9.1
(aa) A 63-year-old woman with complex, predominantly cystic nodule (arrowheads), size 28 × 22 × 20 mm and volume 7 mL in the RL: solid part coarsened structure; hyperechoic; diffuse frequent small cystic cavities (c) and thick septa; halo sign; Tvol 23 mL, asymmetry—RL 16 mL and LL 7 mL; transverse. (bb) Detail of complex, predominantly cystic nodule (arrowheads): diffuse small cystic cavities (c) and thick septa; halo sign; transverse. (cc) Detail of complex, predominantly cystic nodule (arrowheads): diffuse small cystic cavities (c) and thick septa; halo sign; longitudinal