Compression therapy has been used for thousands of years in the practical treatment of wounds and ulcers, with the earliest documentation of compression bandages dating back to the Neolithic Age (5,000–2,500 BC). 1 Throughout the more recent centuries, physicians and surgeons have employed compression therapy for the treatment of wounds/ulcers, primarily using inelastic material such as plaster bandages/dressings. Elastic compression bandages were developed in the mid-1800s after Charles Goodyear developed a process by which to increase the durability and elasticity of rubber. In 1885, German dermatologist Dr. Paul Unna developed an elastic bandage impregnated with zinc oxide paste to help promote healing, which currently is known as the “Unna’s boot.”
In modern medical practice, compression therapy continues to demonstrate an important role in prevention and therapy for a variety of venous diseases, for example, perioperative venous thrombosis, varicose veins, postthrombotic syndrome (PTS), and venous stasis ulcers. There are hundreds of products available on the market today that offer varying degrees of compression. It is imperative that the prescribing provider has an understanding of the pathophysiology of venous disease to guide clinical management, and is also familiar with different products and their specific intended uses.
5.2 Mechanism of Action
The goal of compression therapy is to counteract the effects of gravity upon the venolymphatic circulation. Namely, pressure exerted on an area of the body’s surface with elastic or inelastic materials will help to decrease ambulatory venous hypertension and interstitial pressures to prevent malfunction resulting in venous and lymphatic disorders. 1
5.2.1 Laplace’s Law
Laplace’s law in relation to compression states that external pressure (P) is directly proportional to the tension of material (T) and inversely proportional to the radius of curvature (R) to which tension is applied (P = T/R). 2, 3 Applied to the use of compression bandages/stockings, the law of Laplace dictates that the greatest amount of external pressure will be directed to the ankle (~100%), and external pressure progressively decreases as the radius of the leg increases more proximally (~70% at the knee, ~ 40% at the thigh). This provides the basis for the decreasing graduated compression concept ( ▶ Fig. 5.1).
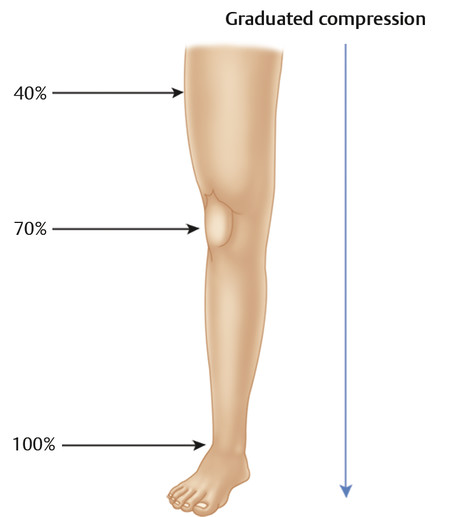
Fig. 5.1 Given Laplace’s law (P = T/R), as the thickness/radius of the leg decreases toward the ankle, greater pressure will be exerted.
5.2.2 Physiology Consequences of Compression
The pressure exerted by compression on the surface of the skin is transmitted to the level of both the superficial and deep blood vessels, helping to improve local venolymphatic circulation at multiple levels.
Edema
By applying external compression, the pressure on the tissues works to counteract filtration, preventing reflux of fluid as well as promoting resorption of excess fluid from the interstitial space ( ▶ Fig. 5.2, ▶ Fig. 5.3). Compression stockings have been shown to decrease limb volume and pain associated with limb edema. 4, 5, 6, 7
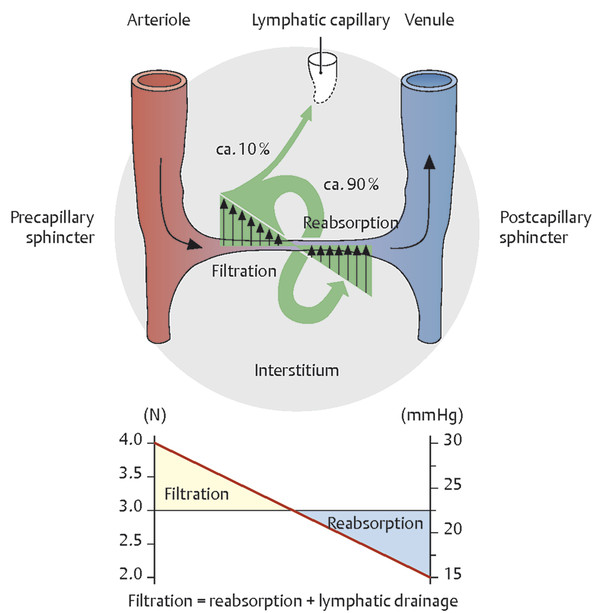
Fig. 5.2 The normal mechanism of lymphatic filtration and reabsorption.
(Used with permission from Schuenke M, Schulte E, Schumacher U. General Anatomy and Musculoskeletal System. Stuttgart: Thieme; 2010. Illustration by Karl Wesker.)
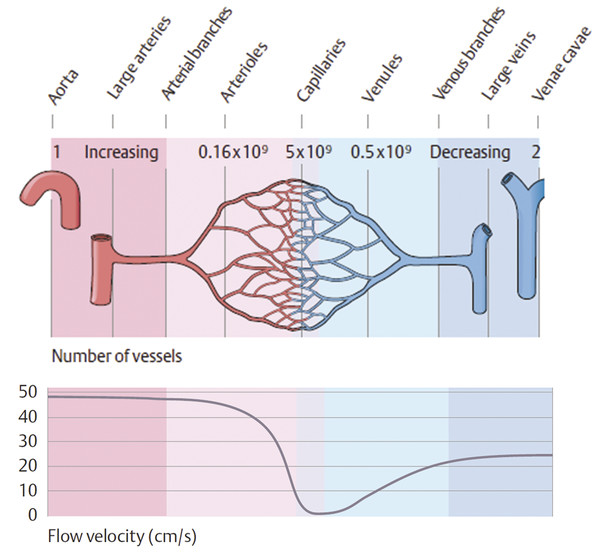
Fig. 5.3 Normal flow velocity across the capillary bed.
(Used with permission from Schuenke M, Schulte E, Schumacher U. General Anatomy and Musculoskeletal System. Stuttgart: Thieme; 2010. Illustration by Karl Wesker.)
Lymphatic Circulation
Compression combined with movement or exercise has been shown to improve contraction of the lymphatic system. 8, 9 Even more important is the impact that compression has upon the capillary bed and downstream lymphatic circulation. Applied compression results in closer proximity of the skin and subcutaneous tissues to the superficial capillary network. This contact results in improved capillary resorption as well as restricted capillary filtration, reducing the lymphatic load ( ▶ Fig. 5.2, ▶ Fig. 5.3). Because compression results in disproportionate removal of water compared to proteins from the tissues, the tissue oncotic pressure increases. This phenomenon necessitates ongoing compression therapy to prevent reaccumulation of water in the tissues, which is important in cases of chronic edema where success is dependent on continued compression. Compression is also shown to have an effect on the breakdown of fibrosclerotic tissue and downregulation of proinflammatory cytokines, reducing membrane permeability and leakage. 10
Venous Circulation
Compression affects the venous circulation by transmitting pressure to narrow or even occlude the superficial and deep venous vessels. The amount of external pressure required to diminish the venous diameter is dependent on body positioning. When a patient is recumbent, pressures as low as 10 to 15 mm Hg are sufficient to reduce venous diameter. 11 Pressures of 20 to 25 mm Hg are sufficient in compressing the superficial veins in the supine position, while pressures of 35 to 40 mm Hg are required in the upright position. 12, 13 Other studies have shown that when using an external blood pressure cuff inflated to 40 to 60 mm Hg in patients with known incompetent valves, they were able to have noticeable decrease or complete resolution of venous reflux as well as decrease in vein diameter. 14, 15 This phenomena was also noted in patients with congenital absence of venous valves, indicating that improvement in reflux and ambulatory venous hypertension may in part be related to the degree of resistance to retrograde flow provided by external compression and not just related to improved valve closure. 16
Capillary Circulation
By increasing local tissue pressure, compression accelerates blood flow in capillaries and reduces capillary filtration, resulting in improved venous flow, improved distribution of microcirculation blood flow, and normalization of leukocyte adhesion ( ▶ Fig. 5.2, ▶ Fig. 5.3). 17, 18, 19, 20, 21, 22, 23 Compression therapy also contributes to ulcer healing by increasing flow volume, thereby reducing endothelial interaction with leukocytes and activation of the inflammatory cascade, which can lead to increased membrane permeability and microvascular damage. 24 Compression also has an indirect mechanical effect in venous leg ulcers by tightening the intracellular junctions between endothelial cells, which has a role in reducing proinflammatory cytokines. 25, 26
Arterial Circulation
The impact of compression therapy on arterial circulation is also important in consideration of compression therapy. With the degree of external compression applied comes the risk of reduction of not only venous diameter but also arterial diameter. It is suggested that pressures above 60 mm Hg will decrease local arterial perfusion, particularly in the recumbent patient. Studies have shown that skin necrosis and ulceration have occurred during prolonged compression, possibly related to unrecognized/occult peripheral arterial occlusive disease. 27 For patients with critical limb ischemia (ankle-brachial index [ABI] < 0.5), sustained compression therapy is therefore a contraindication. However, it is now felt that patients with systolic ankle pressures between 60 and 100 mm Hg in the supine position may still benefit from inelastic compression, using 40 mm Hg or less as an initial pressure with the basis that the massaging effect of compression during ambulation will help to increase venous return and improve the arteriovenous pressure gradient, resulting in improved arterial flow. 28
5.3 Types of Compression Therapy
Compression therapy includes many different devices made of various materials, including graduated compression stockings, bandages, boots, and intermittent pneumatic compression devices. Therapies are generally divided into elastic and inelastic techniques based upon the extensibility (or stretch) of the material with which the device is made.
5.3.1 Inelastic Compression
Inelastic devices include short stretch and no stretch (i.e., inextensible) options, which include the gauze boots (Unna’s boot), dressings, pneumatic compression devices, and inelastic bandages and garments. Inelastic bandages produce high “working pressures” during ambulation and lower “resting pressures.” Because extensibility is dependent on the contraction of muscle, there is little variation in the pressure exerted on the superficial vessels. Furthermore, if the muscle pump is ineffective (as in patients with muscle atrophy or immobility), then the benefit of inelastic compression is limited. 1, 29, 30
The most well-known inelastic compression device is the Unna’s boot, which is composed of a colorless gelatin crepe bandage impregnated with glycerin and zinc oxide paste. 31 The Unna’s boot is used in the treatment of ulcers resulting from chronic venous insufficiency because it results in local pressure when the patient ambulates while simultaneously promoting ulcer healing. Because it requires several days of use to exert maximal effectiveness, care must be taken so that pressure is not excessive enough to cause limb ischemia. Therefore, it is imperative that an experienced team directs application and management of the Unna’s boot.
Pneumatic compression devices are another well-known inelastic device commonly used for deep vein thrombosis (DVT) prevention and also applied primarily at night for patients with refractory edema and venous ulcers.
5.3.2 Elastic Compression
Elastic compression consists of extensible or long-stretch materials, such as compression stockings, multilayer elastic wraps, and elastic bandages. Elastic compression works in all positions, including the supine position. Unlike inelastic compression, elastic compression must be removed at night to avoid arterial inflow problems. 32
Compression Stockings
Elastic compression stockings have both short- and long-term applications. Common applications for short-term therapy include in the postsurgical setting as well as following endovenous therapies and sclerotherapy. Long-term use may be indicated in patients with chronic venous insufficiency. Compression stockings should be routinely adjusted as the diameter of the leg and edema decrease/stabilize to ensure a proper fit.
Compression Stocking/Bandage Pressures
The sub-bandage pressure is determined by a combination of three things: material stiffness and elasticity, size and shape of the leg, and activity level of the patient. 33 The universally adopted unit of measure for pressure exerted by elastic compression stockings is millimeters of mercury (mm Hg), which has been the measure used worldwide in studies regarding compression therapy. 3, 34
Style and Sizing
It is important that clinicians have the necessary training and adhere to guidelines for assessing and caring for patients who wear compression stockings. 33 Wearing an improperly fitted stocking can result in pressure-induced necrosis related to inadequate perfusion. In cases where the stocking is too long, the stocking may roll down and effectively create a tourniquet for the remaining lower extremity. Therefore, the amount of lengthwise stretch is also an important factor to consider to prevent stockings from slipping down. 32
Elastic stockings come in various different lengths. The particular style and length for a patient is best determined by the type and degree of disease, but other factors to consider are ease of use, comfort, and cost. Compression stockings can be custom made or standard fit.
Knee-high stockings end just below the knee. While they do not treat pathology in the thigh, they will help to prevent accumulation of fluid in the lower leg and sequelae of chronic edema, venous insufficiency, and varicose veins. This style tends to be best tolerated by the patient and is also the easiest to apply and least expensive.
Thigh-high stockings extend to the upper/midthigh level. These can be useful in patients who have significant pathology in the thigh or who have undergone vein ablative therapy/surgery to the level of the thigh to prevent recanalization ( ▶ Fig. 5.4).
Full-length stockings or tights include coverage from the foot to the level of the hips. Full-length stockings can cover one leg or both legs. For patients who feel that the stocking is too oppressive, some brands can be ordered with the foot open to air.
Compression stocking sizes and fits vary by manufacturer, so it is important to obtain accurate measurements prior to prescribing the stockings. Once measurements are obtained, the stockings can be appropriately fitted for maximum comfort and benefit, which will help to improve patient compliance.

Fig. 5.4 Pressure dressings (left) followed by application of thigh-high compression stockings (right) in a patient post sclerotherapy.
Materials
Compression stockings can be made from a variety of materials, including nylon, cotton, spandex, and natural rubber. The most commonly used material in elastic stockings is spandex with different proportions of added cotton or other materials. 3 The combination and thickness of the fibers determines the elasticity of the stocking.
Use of Stockings
Stockings that are to be worn every day should be prescribed for a period of 3 to 6 months and should be replaced with new stockings after the recommended time period. 28, 29 It is important that before the stockings are replaced, the patient is reevaluated by a physician to determine whether the pressure gradient needs to be adjusted or can be maintained. Stockings generally should be put on in the morning and taken off at night to sleep; however, their use should be individualized. 35 When the stocking is too tight at the calf, it can cause a feeling of strangulation, and is an incorrect fit for that patient. An important factor to improve the clinical course of the venous disease is the daily use of stockings. However, due to a variety of reasons, which can include patient discomfort as well as technical difficulty in use, many patients end up not using the stockings as recommended by their physician. 36 A systematic review of compression hosiery found that patients who complied with wearing stockings tended to be older or had endured their symptoms longer. 33 Patients may be noncompliant with wearing stockings if they feel they do not work or they are too tight or too hot. 33 In addition, patients who are obese or elderly may have difficulty applying the stockings, leading to noncompliance. 13
5.4 Clinical Indications
For many years, compression therapy was based on empiric studies. However, with more recent prospective and detailed randomized studies by different medical societies and with the rise of dedicated research by various authors, the International Compression Club was created where parameters were established for the use of graduated compression pressures in stockings. 30
5.4.1 Prevention of Varicose Veins and Telangiectasias
The etiology of varicose veins has not yet been fully elucidated. Data suggest that a molecular defect in the vessel wall leads to dilation of the vein, and anatomic abnormalities result in disturbances of hemodynamics that promote progression of disease. Because the deep venous system is encased by a musculofibrous sheath, these veins can accommodate changes in blood pressure that increase the volume of the vessel. Conversely, the superficial veins are not contained within a sheath and valves become incompetent when the vessel lumen expands beyond capacity. Blood is then routed into smaller vessels and produces abnormal dilation, resulting in clinically visible varicose veins and telengiactasias. 11
External compression of previously untreated veins by bandages or graduated stockings produces pressure to move blood toward the heart rather than outward to the vessel wall. There are no randomized controlled trials demonstrating that compression therapy prevents progression of venous disease. However, patients with varicose veins report relief of symptoms with all classes of compression stockings. 37, 38, 39 Physiologic improvement in varicose veins only occurs with 30 to 50 mm Hg stockings. 11
The need for compression therapy prior to an intervention remains highly controversial. Ablation of varicosities has proven more efficacious and cost-effective in the treatment of superficial reflux and argues against a trial of compression therapy prior to ablation as required by many third-party payers. 13
5.4.2 Sclerotherapy
Sclerotherapy involves injection of a liquid or foam sclerosing agent into the targeted vessels causing inflammation and focal thrombosis of the target vessel, eventually resulting in permanent obliteration and fibrosis. Sclerotherapy is one of many minimally invasive treatment options available for the treatment of varicose veins and has been found to be safe. Sclerotherapy has demonstrated decreased wound infection and neovascularization compared to conventional surgery, with significant improvement in clinical and quality-of-life metrics. 40
Compression therapy serves several purposes following sclerotherapy of varicose veins, including direct apposition of the treated vein walls to produce better fibrosis, decreased thrombus formation and subsequent risk of recanalization and postsclerosis pigmentation, prevention of telangiectatic matting, improvement of the physiologic function of the calf muscle pump, and increased blood flow through the deep venous system which prevents damage to the valves by the sclerosing agent. 11
One study found that patients who used postsclerotherapy elastic compression stockings had a statistically significant degree of symptom improvement at 6 weeks compared to those who did not use compression stockings. 41 In addition, patients who wore the compression stockings for 3 weeks had less postsclerotherapy hyperpigmentation compared with those who wore them for a shorter duration. Finally, there was less bruising, telangiectatic matting, edema, and ulceration in those who wore compression stockings compared to those who did not wear stockings. 41
Stockings in the 20 to 30 mm Hg pressure range at the ankle have beneficial effects after sclerotherapy of small telangiectasias. However, a compression pressure of 30 to 40 mm Hg at the ankle corresponds to approximately 10 to 20 mm Hg elsewhere in the leg and is generally recommended for better outcomes. 42 Some physicians support the use of foam pads or rolled cotton wool to augment local pressure beneath the compression stocking ( ▶ Fig. 5.5).

Fig. 5.5 Pads used with compression bandage to create more pressure over the desired area in the lower extremity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree