Computed tomography angiography (CTA) is an exciting technology that allows noninvasive assessment of the vasculature. Over the past few decades, the use of CTA has grown tremendously due to the introduction of multidetector CT (MDCT), which enables acquisition of isotropic volumetric data. Technologic advances in MDCT, coupled with the advances in imaging workstations, have permitted high-quality multiplanar and three-dimensional (3-D) reformations that have opened new paradigms in the field of vascular imaging. As a consequence of these developments, MDCT angiography has superseded conventional catheter-based angiography as the preferred technique for diagnosis of cardiovascular disease. Ongoing innovations in MDCT technology, such as the introduction of dual energy CT (DECT), have further diversified the role of imaging in visualization and characterization of vascular abnormalities. MDCT angiography has thus positioned itself as an integral component in the multidisciplinary management of patients with cardiovascular disease not only by facilitating accurate diagnosis but also by enabling posttreatment follow-up.
The dramatic growth in the field of CTA began with the introduction of spiral or helical CT and achieved greater strides with MDCT, which allowed volumetric acquisition in a single breath hold. The advantages of MDCT over single detector CT include increased temporal and spatial resolution, decreased image noise, efficient x-ray tube use, and longer anatomic coverage, all of which help increase the diagnostic accuracy of the examination. Better z-axis resolution and larger scan volumes also result in improved multiplanar reconstruction in the coronal and sagittal planes. The reduced scanning time achieved by MDCT also helps reduce respiratory and motion artifacts. The development of electrocardiogram gating technology synchronized with CT data acquisition has enabled acquisition of high-resolution images of the heart and coronary arteries within a single breath hold and has thus eliminated motion artifacts. The superiority of MDCT has also been enhanced by improved image postprocessing techniques, which have expanded the role of modern day CTA to virtually all vascular territories. This chapter discusses the key concepts of MDCT angiography technique in the evaluation of vascular disease.
Catheter Versus Computed Tomography Angiography
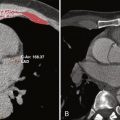
MDCT angiography offers several advantages over conventional catheter-based angiography. The first and foremost benefit is the noninvasive nature of CTA, which limits the morbidity associated with catheter angiography and often causes little patient discomfort. Several of the vascular complications related to catheter angiography (e.g., bleeding, groin hematoma, and vascular thrombosis) are not encountered with CTA. Second, whereas catheter-based angiography provides a limited luminal view of the blood vessels, the volumetric acquisition with MDCT allows clear anatomic definition of the lumen, as well as of mural thrombus, atherosclerotic plaque, vessel wall, and adjacent structures. The exoluminal information provided by MDCT is particularly important when dealing with complex vascular diseases such as for (1) identifying pseudoaneurysms, (2) allowing accurate delineation of true and false luminal flow in arterial dissections, (3) showing perigraft blood flow in aortic stent grafts, and/or (4) depicting hematoma in traumatic vascular injuries. Third, CTA provides excellent depiction of the atherosclerotic plaque complex and its composition (i.e., fibrofatty versus calcified) that can have significant ramifications in patient management. Fourth, the cross-sectional nature of CT data acquisition allows simultaneous assessment of the function and integrity of target organs supplied by the vessels. For example, CT allows detection of ischemic changes in the bowel wall in mesenteric ischemia and delineation of the extent of cerebral infarction in carotid occlusive disease. This additional assessment of end-organ perfusion allows the referring physician to make crucial clinical decisions and has contributed to the frequent use of CTA in routine practice.
Computed Tomography Angiography: Basic Concepts
The basic principle of CTA is similar to that of catheter angiography because it exploits the inherent ability of iodinated contrast material (CM) to absorb x-rays and thereby generate an attenuation difference between the vessel and surrounding structures. This enhancement or the increase in attenuation in a given vessel achieved following intravascular injection of iodinated CM is directly proportional to the iodine concentration. The central purpose of CTA is to achieve an adequate iodine concentration (and thus increased attenuation) within the vessel of interest to enable accurate delineation of the vascular anatomy and disease. However, in contrast to catheter angiography, which involves direct arterial injection of CM, CTA involves intravenous administration of the CM to obtain arterial or venous opacification. Thus, the contrast dynamics governing arterial opacification in CTA are different from those involved in catheter angiography. Moreover, arterial opacification in CTA is not a static process, but rather a dynamic one dependent on several interconnected factors broadly classified as (1) patient-related factors, (2) CM-related factors, and (3) technical parameters. The following sections discuss these factors in greater detail. However, given the wide range of CT technology available, the varying patient physiologic features, the different vascular territories, and the complex cardiovascular diseases encountered, no universal CTA strategy exists. The following discussion is intended as a guide for basic understanding of CTA technique.
Patient-Related Factors
In terms of contrast dynamics and the CTA technique, understanding the influence of patient-related factors is very important. Out of the several patient-related factors, the most relevant include patient body habitus and cardiac output. Certain other factors (e.g., renal function and venous access) are also key to obtain a diagnostically acceptable CTA study. The targeted vascular structure and clinical situation also are essential for planning a CTA examination.
Patient Body Habitus
During planning of CTA, the body habitus of a patient needs careful consideration because of its impact on contrast dynamics. The common measures used to estimate body habitus include the body weight and body mass index. The body weight and the magnitude of contrast enhancement in a CTA examination are inversely related to each other. Therefore, for a given dose of iodinated CM, large patients have a lower degree of contrast enhancement than do small patients. The contrast circulation time and the timing of contrast enhancement (e.g., arterial peak) are not affected by body weight for the most part. The volume and injection rate of the CM should be tailored to the patient’s body weight (i.e., the CTA protocol should be different in large and small patients). When planning CM protocols in patients of large body weight, the following strategies are beneficial: (1) using a higher overall iodine dose (i.e., higher CM volume or concentration) to maintain a constant degree of contrast enhancement and (2) using a faster injection rate to augment the magnitude of contrast enhancement.
Cardiac Output
Cardiac output is a crucial factor affecting the CM circulation time and so determines the timing of contrast enhancement during CTA. Cardiac output governs the following components of contrast dynamics: the time of CM bolus arrival, the peak arterial and parenchymal enhancement, and clearance of the CM from the circulation. The time duration between the injection of CM through an intravenous route and the peak arterial enhancement in the aorta are directly proportional to cardiac output. However, the magnitude of arterial enhancement is inversely related to cardiac output. Therefore, the degree of arterial enhancement is lower in patients with high cardiac output as compared with patients with low cardiac output. In addition, in patients with low cardiac output, an increased and prolonged magnitude of peak aortic enhancement results from the late peak arterial enhancement because of delayed arrival of the CM and the reduced clearance of the CM from circulation. Given the significant interpatient and intrapatient variability of cardiac output, the scan timing must be individualized for each patient. The scan timing can be tailored to each patient either by test bolus or through a bolus tracking technique (discussed in detail later).
Renal Function
Patients must be screened before CTA to assess for risk of CM-induced nephropathy. A detailed discussion of this disorder is beyond the scope of this chapter. Serum creatinine and (estimated glomerular filtration rate [eGFR]) should be routinely checked before CM use in high-risk patients such as those with diabetes, myeloma, sickle cell anemia, cardiac failure, or a personal or family history of renal disease. Patients with an eGFR of more than 60 mL/minute/1.73 m 2 receive the usual dose of intravenous CM. Patients with an eGFR between 30 and 60 mL/minute/1.73 m 2 are given intravenous hydration and a standard or reduced dose (pertinent to the clinical situation) of CM. Intravenous CM is not administered to patients with an eGFR of less than 30 mL/minute/1.73 m 2 .
Intravenous Access
The routine use of power injectors for intravenous delivery of the CM in CTA requires appropriate venous access to maintain the desired injection rate and thus optimal iodine flux. Obtaining adequate intravenous access is crucial not only to sustain the high injection rate (i.e., ≤8 mL/second for cardiac CTA studies) for the intended iodine flux, but also to prevent unintended extravasation of the CM. For most diagnostic CTA studies with an injection rate of 3.5 mL/second, a 22-gauge intravenous cannula is sufficient. However, higher injection rates of 5, 7, or 10 mL/second mandate intravenous access of 20, 18, and 17 gauge, respectively. When a disparity exists between the size of the intravenous access and the desired injection rate, the scan delay and CM volume must be adjusted according to the timing of acquisition.
Contrast-Related Factors
A key determinant of a diagnostically acceptable CTA scan is an optimized CM administration protocol. The CM delivery technique must be tailored to the specific vascular structure being studied and the clinical question that needs to be answered. In addition, the timing of CTA data acquisition should be synchronized with the CM delivery technique to optimize arterial enhancement. Arterial opacification is a time-dependent phenomenon, and attenuation of the vessels can be altered by changing the injection parameters. The fundamental components of a CM administration protocol include the volume (milliliters) and injection rate (milliliters/second) of the CM, the injection duration (seconds), the scan delay (seconds), and the use of a saline flush.
Iodine Concentration
The iodine concentration of the CM directly affects the magnitude of peak contrast enhancement. With all factors kept constant (i.e., volume and injection rate of the CM and injection duration), increasing the iodine concentration increases the iodine delivery rate and results in a higher degree of peak enhancement and a prolonged duration of enhancement. The time to peak enhancement is not affected by the iodine concentration, however. Interest in the use of CM with high iodine concentrations (≥350 mg iodine/mL) for various MDCT applications is growing. The use of CM with high iodine concentrations has enabled the use of lower CM volumes as compared with CM with low iodine concentrations. However, the decrease in CM volume shortens the duration of enhancement and thus necessitates the use of faster scanning to permit data acquisition in the arterial phase. Iodine concentration and injection rate have the same proportional effect on arterial enhancement, and hence use of higher iodine concentrations is a substitute for a higher injection rate when increased iodine delivery rate is desired. For example, increasing the CM injection rate from 4 to 5 mL/second and increasing the iodine concentration from 300 to 350 mg iodine/mL result in a rise in arterial enhancement by 45%.
Injection Rate
The degree of arterial enhancement is directly proportional to the rate of iodine administration (i.e., doubling the injection rate produces an enhancement response that is twice as strong). A faster injection rate is also associated with a shorter time to peak enhancement. The incremental increase in enhancement observed following faster injection plateaus beyond a certain limit for a given patient, however. Studies show that increasing the injection rate beyond 8 mL/second does not produce stronger enhancement because of pooling of the CM in the central venous system and CM reflux into the inferior vena cava. This limit might be reached at a slower injection (i.e., <8 mL/second), when patients have a low cardiac output or diminished right ventricular function. The injection rates in large patients should be faster than those in small patients when the injection duration and volume of the CM are kept constant. Another important concept pertaining to injection rate is the ability to separate out contrast enhancement phases during multiphasic scans by using faster injection rates. For example in multiphase MDCT examination of the liver, more optimal separation of arterial and portal venous phases is possible with a faster injection rate. The routinely recommended CM injection rate for CTA studies is approximately 5 mL/second, which allows downregulation (≤4 mL/second) and upregulation (≥6 mL/second) according to the patient’s physiology.
Injection Duration
The duration of CM injection affects both the timing and the magnitude of contrast enhancement and is determined by the CM volume and injection rate. The longer the injection duration is, the greater the amount of iodine mass deposited will be. This results in a continuous temporal increase in arterial enhancement caused by the cumulative effects of freshly arriving CM and recirculated CM. In patients with normal cardiac output, peak arterial contrast enhancement is achieved shortly after termination of CM injection. As the volume of the CM increases, so does the time required to reach the peak of arterial or parenchymal contrast enhancement.
Selecting the appropriate injection duration based on patient-related factors and the clinical objective of the scan is important. For longer scanning (e.g., evaluation of the aorta and iliac arteries), the injection duration should be increased to maintain optimal enhancement throughout the period of image acquisition. However, too long an injection duration is not beneficial because it can result in undesirable parenchymal and venous enhancement and also leads to wastage of the CM. A shorter injection duration often results in inadequate degree and duration of contrast enhancement. To obtain optimal arterial enhancement in large patients, the injection duration should be longer than that for small patients for a fixed injection rate. Adding a constant factor (3 or 4 seconds) to the injection duration with a fast injection rate is often beneficial, to widen the temporal window for acquisition during peak arterial enhancement.
Contrast Material Volume
The volume of the CM for diagnostically acceptable CTA is mainly determined by the intended degree of enhancement and the vessels to be scanned. It also depends on several factors, including patient body weight, iodine concentration, CM injection rate, and scan duration. Contrast enhancement of 250 to 300 HU has been suggested to be adequate for the diagnosis of numerous vascular disorders. Larger patients often require a higher iodine dose to achieve a degree of contrast enhancement comparable to small patients. Furthermore, the CM requirement can be reduced by up to 15 to 25 mL with the use of a saline flush.
The CM volume, the CM injection rate, and the injection duration are interrelated. Their relationship can be described by the following simple equation:
CM volume ( mL ) = Injection flow rate ( mL / second ) × Injection duration ( seconds )
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree