Congenital Urinary Tract Abnormalities
Ramesh S. Iyer, MD
LEARNING OBJECTIVES
1. List three common imaging examinations used to evaluate congenital anomalies of the urinary tract.
2. Describe how you would perform a VCUG, including desired bladder fill volume.
3. Discuss the vesicoureteral reflux grading system.
4. Identify ureteropelvic junction obstruction on renal US.
5. Describe typical renal US and VCUG features of complete collecting system duplication.
6. Identify posterior urethral valves on VCUG.
INTRODUCTION
Congenital abnormalities of the urinary tract have a wide spectrum of etiologies and imaging appearances. They are most often discovered during the workup for a urinary tract infection (UTI) or suspected on prenatal imaging. The primary imaging modalities used are ultrasound and voiding cystourethrogram (VCUG). Renal scintigraphy may be used to characterize pathologies such as parenchymal scar and collecting system obstruction. MR urography is also being increasingly utilized, offering both anatomic and functional information.
VESICOURETERAL REFLUX
Vesicoureteral reflux (VUR) refers to retrograde passage of urine from the bladder into the ureters and often into the renal pelvis and calices. It is typically imaged and managed in the context of UTIs. The main concern with reflux is that infected urine can travel from the bladder into the kidney, causing pyelonephritis. Recurrent pyelonephritis may cause renal scar, which in turn predisposes to hypertension, proteinuria, and chronic renal insufficiency later in life.1, 2, 3 and 4
The associations among reflux, UTIs, and renal pathology have become more controversial in recent years. The prevalence of VUR in asymptomatic children is commonly reported as 1%, compared to 25% to 40% in children with UTIs.2,5,6 But recently, authors have reported a higher incidence of reflux in asymptomatic children than previously suspected.1,7 UTIs have not been shown to cause VUR, and acute pyelonephritis and reflux frequently occur independently of one another.3,8 Severe reflux is also more likely to cause pyelonephritis by renal scintigraphy, but not necessarily scar formation.9
VUR is divided into primary and secondary causes. Primary or congenital reflux, which is more common, results from a short intramural segment of the distal ureter. The bladder wall musculature acts as a passive valve, and if the distal ureter traverses the wall with too straight a course, then reflux occurs.1,2 Secondary VUR occurs in the setting of either bladder outlet obstruction (e.g., posterior urethral valves [PUVs]) or neurogenic bladder.1 As with pediatric UTIs, the majority of VUR occurs in children under 2 years of age. Girls are affected more often than are boys by a 2:1 ratio.10 There is strong evidence for heritability with reflux: the prevalence of asymptomatic VUR in siblings of children with reflux is 25% to 50%.2,10, 11 and 12
Basic imaging modalities used for VUR workup include VCUG and renal ultrasound. Contrast-enhanced voiding urosonography (VUS) is a newer technique for diagnosing reflux, though currently not widely used.13 Fluoroscopic VCUG is the traditional modality of choice for identifying VUR and grading its severity. The exam begins with a scout radiograph to reveal abdominal calcifications, foreign bodies, and bony or other abnormalities. An 8-French bladder catheter is appropriate for most children, while a 5- to 6-French catheter is used for young infants.14 The bladder must be filled to near capacity for a reliable study. Desired bladder volume is estimated using the equations below:
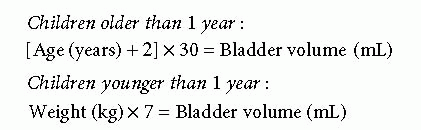
Infants younger than 1 year should have the bladder filled two to three times during the study (filling cycles). The bladder wall contracts involuntarily in young infants, so performing multiple cycles ensures that the bladder is filled adequately and that VUR occurring after the first fill-void cycle is not missed. AP image of the bladder during early filling evaluates for ureterocele or bladder tumor that may be obscured by
more intraluminal contrast. When the bladder is near capacity, oblique views of the distal ureters/ureterovesical junctions (UVJs) and AP view of the kidneys are performed. Voiding images are captured in the lateral projection for boys and AP projection for girls. Obtaining voiding images both before and after catheter removal is recommended, particularly for boys, to facilitate bladder cycling in infants and bladder drainage if needed. Urethral disease in girls is rare, and so one voiding image is usually enough.1,14 A postvoid image of the kidneys should also be acquired.
more intraluminal contrast. When the bladder is near capacity, oblique views of the distal ureters/ureterovesical junctions (UVJs) and AP view of the kidneys are performed. Voiding images are captured in the lateral projection for boys and AP projection for girls. Obtaining voiding images both before and after catheter removal is recommended, particularly for boys, to facilitate bladder cycling in infants and bladder drainage if needed. Urethral disease in girls is rare, and so one voiding image is usually enough.1,14 A postvoid image of the kidneys should also be acquired.
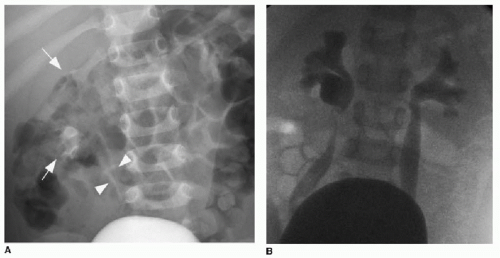
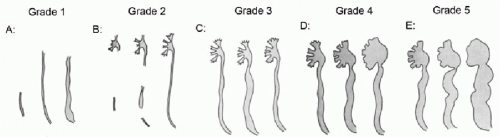 FIG. 19.1 • Grading system for vesicoureteral reflux.1, 2, 3, 4 and 5 (Modified and reprinted with permission: Lebovitz RL, Olbing H, Parkkulainen KV, et al. International system of radiographic grading of vesicoureteric reflux: international reflux study in children. Pediatr Radiol. 1985;15(2):105-109.) A: Grade 1 reflux into ureter only. B: Grade 2 reflux into renal pelvis and calices with sharp fornices. C: Grade 3 reflux into mildly dilated/blunted calices. Ureteral dilatation is mild. D: Grade 4 reflux into moderately dilated renal pelvis and calices, as well as ureteral dilatation and tortuosity. E: Grade 5 reflux into severely dilated/blunted calices, as well as moderate to severe ureteral dilatation and tortuosity. |
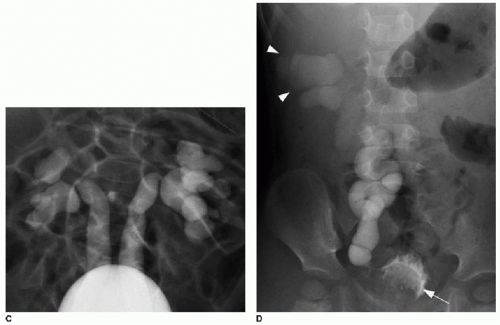
The international grading of VUR is based on VCUG findings.15 Grading is from 1 through 5, with grade 5 being most severe (Fig. 19.1). Grade 1 reflux enters the ureter only. Grade 2 reflux enters the kidney without collecting system dilatation; the renal calyces remain sharp. With grade 3 reflux, there is mild calyceal dilatation and blunting. With grades 4 and 5 reflux, there is progressive pelvicalyceal dilatation and ureteral enlargement and tortuosity (Fig. 19.2).
Renal US should also be performed in children with confirmed or suspected reflux. There may be little or no collecting
system dilatation by ultrasound despite having severe reflux by VCUG. Renal morphology such as scarring or collecting system duplication is shown (Fig. 19.3). Additional findings on US seen with reflux are urothelial thickening and fluctuating caliber of the pelvicalyceal system and ureter.1
system dilatation by ultrasound despite having severe reflux by VCUG. Renal morphology such as scarring or collecting system duplication is shown (Fig. 19.3). Additional findings on US seen with reflux are urothelial thickening and fluctuating caliber of the pelvicalyceal system and ureter.1
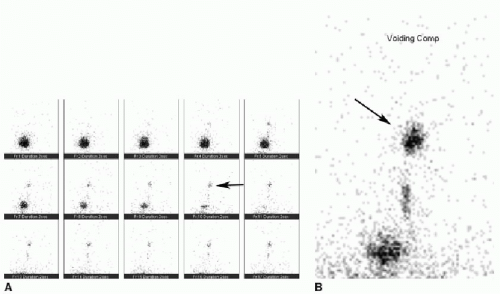
Direct radionuclide cystography may also be performed to assess for reflux. Technetium 99m-labeled sulfur colloid is mixed with normal saline and introduced into the bladder through a catheter. Planar images are then obtained continuously over the bladder and kidneys, often for a 1-hour duration (Fig. 19.4). Radionuclide cystograms are limited by lack of anatomic detail in grading VUR and their inability to accurately show the male urethra. However, they have reportedly greater sensitivity than VCUG because of continuous imaging over time and similar to slightly lower radiation exposure compared to modern fluoroscopy units.1,2,10 The commonly accepted practice is to perform a VCUG as the initial examination to evaluate reflux severity and identify anatomic abnormalities, and either VCUG or
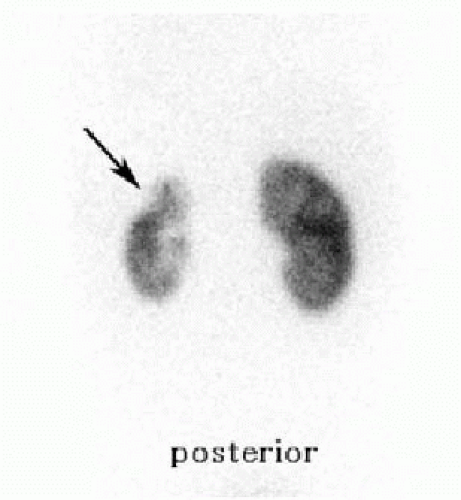
radionuclide cystography for follow-up studies.2 Renal cortical scintigraphy using dimercaptosuccinic acid is highly sensitive for detecting acute pyelonephritis and scar. Both of these conditions appear as photopenic defects in the renal cortex (Fig. 19.5).9,16
radionuclide cystography for follow-up studies.2 Renal cortical scintigraphy using dimercaptosuccinic acid is highly sensitive for detecting acute pyelonephritis and scar. Both of these conditions appear as photopenic defects in the renal cortex (Fig. 19.5).9,16
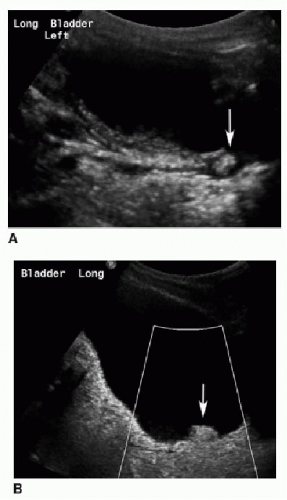
The majority of VUR tends to resolve spontaneously by 4 to 6 years of age. This is because of maturation of the UVJ and lengthening of the intramural ureteral segment. There is a higher spontaneous resolution rate with mild reflux (greater than 80% for grades 1 and 2) than with higher grades (50% for grade 3, 30% for grade 4, rare for grade 5).1 Along with lower reflux grade, male gender, unilateral disease, and age at presentation of less than 1 year are predictive of resolution.17 It is currently standard practice to administer antibiotics once reflux is diagnosed and to continue therapy until reflux has resolved, to prevent recurrent UTIs and renal scarring. However, recent studies have shown that antibiotic prophylaxis does not significantly reduce these risks, particularly for mild to moderate reflux.18, 19 and 20 An antireflux intervention may be necessary for persistent and/or symptomatic high-grade VUR. This includes either surgical ureteral reimplantation or endoscopic subureteral injection of a bulking agent such as dextranomer/hyaluronic acid (Deflux). After endoscopic injection, ultrasound will show an echogenic mound at the UVJ (Fig. 19.6).
URETEROPELVIC JUNCTION OBSTRUCTION
Ureteropelvic junction (UPJ) obstruction is the most common cause of congenital urinary tract obstruction. It is defined as obstruction of antegrade flow of urine from the renal pelvis into the proximal ureter. There is resultant moderate to marked pelvicaliectasis with a normal size ureter. Boys are affected more often than girls, the left kidney is more often affected than the right, and 30% of UPJ obstructions are bilateral.21,22 The etiology of UPJ obstruction has not been fully clarified. The most likely cause is dysfunction of smooth muscle cells that impairs peristalsis. Other possible intrinsic causes include abnormal innervation, fibrosis, collagen deposition, and kinking.23 Extrinsic compression of the UPJ by a crossing renal vessel may also occur.21 UPJ obstruction typically presents as prenatal hydronephrosis. In neonatal life, a palpable abdominal mass may be found. UPJ obstruction may be associated with other congenital anomalies of the urinary tract. These include VUR, collecting system duplication, contralateral multicystic dysplastic kidney, and UVJ obstruction (Table 19.1).24 and 25
On US, there is hydronephrosis of variable severity and a normal ureter (Fig. 19.7). The renal pelvis is often disproportionately enlarged compared to the calyces. There is abrupt narrowing of the pelvis at the UPJ. Diuretic renal scintigraphy is often performed to evaluate the severity of the obstruction and differential renal perfusion and function. High-grade UPJ obstructions will show a dilated renal collecting system that responds poorly to furosemide challenge (Fig. 19.8).10,27,28 MR urography is also being utilized for evaluation of UPJ obstruction both before and after surgical repair. The exam combines a detailed anatomic evaluation of the urinary tract with functional data including differential renal function.29
Treatment for UPJ obstruction is often conservative, particularly when renal function is preserved. A large fraction of patients with UPJ obstruction identified prenatally resolve without intervention.30,31 Indications for surgical repair include reduced renal function and severe sustained or increased hydronephrosis.32 The traditional surgical management of UPJ obstruction is pyeloplasty. Ureteral stents crossing the anastomosis are left in place for several weeks postoperatively.10
COLLECTING SYSTEM DUPLICATION
A duplex or duplicated collecting system represents a kidney that is drained by two pelvicalyceal systems. With complete duplication, there are two distinct ureters that drain separately into the bladder. With incomplete duplication, there may be a bifid renal pelvis, two ureters superiorly that join at the midureter level, or two ureters that join just proximal to the bladder.27,33,34




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree