Abstract
Assessment of contractile function in the context of heart failure is mandatory. Of course, one has to measure the left ventricular ejection (LVEF) for distinguishing heart failure with preserved ejection fraction (LVEF > or = 50%), and heart failure with reduced ejection fraction (LVEF < 45%). But, that is not enough. One has to take advantage of the new and advanced imaging modalities for assessing the right ventricular function as well. The right ventricle is essential for the functional prognosis as well as for predicting the risk of death. Cardiac magnetic resonance could be complementary to echocardiography. Nuclear medical imaging is useful, especially for the assessment of function, and cardiac magnetic resonance is crucial for the anatomy and the look of myocardial fibrosis.
Therefore, there is an urgent need to learn how to use echocardiography and each of its modalities, cardiac magnetic resonance and nuclear Imaging, to best understand the reasons for heart failure and their consequences. Not every patient should get each of these modalities; a choice is mandatory according to the clinical setting.
Keywords
Anatomy, Function, Left and right ventricles, Strain, Fibrosis, Perfusion and metabolism
12.1
Introduction
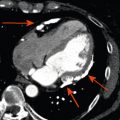
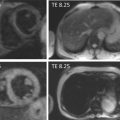
Heart failure (HF) is a growing problem worldwide. Almost 6 million Americans and 15 million Europeans have HF [ , ]. Normal ventricular function requires coordinated electrical activation and contraction but also appropriate pre- and after-loads. Given the 3D pattern of ventricular activation and contraction, the assessment of mechanical activation using conventional imaging methods is complex [ , ]. Several imaging techniques might be necessary in HF patients. For instance, the most prevalent etiology of HF is coronary artery disease. In that context, one must assess myocardial viability (and sometimes ischemia) using stress echocardiography, stress nuclear medical imaging, or cardiac magnetic resonance (CMR) [ , , ]. CMR provides imaging of the scar (subendocardial or transmural or patchy, according to the etiology). With regards to the objective of this chapter of contractility in HF, one might also be aware of the potential usefulness of innervation imaging for best adapting the treatment strategy in HF patients [ , ]. This nuclear technique might help to best select patients requiring an intra-cardiac defibrillator (ICD).
HF is complex. There are several etiologies and clinical expressions reported in guidelines for HF with depressed ejection fraction (EF) and HF with preserved EF when the left ventricular (LV) EF ≥ 50%. For dealing with this complexity and multiplicity of the HF syndrome, imaging is no longer thought of as a single and mono parametric approach. One has to use a combination of techniques for a precise diagnosis and, hopefully, a greater individualization of patients’ treatment strategies [ ].
That is not clearly demonstrated yet; it is efforts remain necessary to affirm the key role of imaging techniques for best treating patients with HF even if the role of imaging is to increase guideline after guideline for HF [ ]. For instance, the impact of cardiac resynchronization therapy (CRT) on global systolic and diastolic performance in dyssynchronous hearts provides an interest in understanding the physiological background for optimal LV performance. Unfortunately, contradictory results have been published, and even if the subject is still in debate, imaging techniques are not key in the indication of CRT [ ]. The complexity of LV function assessment in HF patients is related to the complexity of heart anatomy and of electromechanical interaction and to the load dependency of all the parameters that are obtained in clinical practice [ , , ]. One must thus keep testing imaging techniques in trials in order to demonstrate their key role. Also, imaging techniques have to be available, cost-effective, robust, and feasible; also, they are performed by only a very few experts.
The starting point for this chapter about HF and contractility is based on the work of Torrent-Guasp et al. [ ]. This author showed that both ventricles consist of a single myofiber band extending from the right ventricular (RV) muscle just below the pulmonary artery to the LV muscle where it attaches to the aorta; it is twisted and wrapped into a double helical coil during evolutionary and embryological development. In this construct, sequential activation and contraction beginning in fibers near the pulmonary artery and spreading toward the aortic end of the band might explain the pattern of ejection and suction needed for ventricular output and filling. Disease resulting from ischemic or non-ischemic mechanisms may produce architectural distortion and create a more spherical ventricular shape.
The counter-directional arrangement of muscle fibers helps maintain stability and minimizes energy expenditure. For quantification of fiber orientation, the helix and transverse angles were introduced by Streeter and Hanna [ ]. The helix angle represents the angle between the circumferential axis and the projection of the myofiber onto the circumferential-longitudinal plane. The myofiber helix angle changes continuously from the subendocardium to the subepicardium, from a right- to a left-handed helix, typically ranging from − 60° at the subendocardium to 60° at the subepicardium [ , ]. All the descriptions proposed, especially by Torrent-Guasp et al., have been confirmed using advanced imaging techniques and CMR, in particular. Diffusion-tensor magnetic resonance imaging has confirmed that myocardial fibers within the ventricular mass are arranged in layers of counter-wound helices, encircling the ventricular cavities [ , ]. Evidence suggests that the configuration of these fibers serves to equalize stresses and strains across the thick-walled ventricle, allowing an optimal mechanical functioning of the heart throughout the cardiac cycle [ ]. Nevertheless, if the anatomy seems clearly described, and if one knows approximately how the heart is activated, there is still a lot of mystery, and ongoing work is attempting to deal with the key problem of the coupling between the electrical activation (first) and the mechanical consequence (electromechanical coupling).
In this chapter, we first summarize the echocardiographic capabilities for assessing cardiac function or contractility (global and regional). We will distinguish the assessment of the left and the right ventricles. Then, we will discuss CMR and nuclear imaging approaches that are usually complementary for the best management of any single patient with HF (chronic). Clearly, all imaging modalities should not be used in every individual patient. One will probably use echocardiography for the initial assessment and the follow-up. CMR and nuclear imaging will be used afterward and less frequently for the etiologic diagnosis and to assist in the treatment strategy and/or the prognosis assessment. Also, cardiac CT can provide accurate indices of global LV function. While the technique is not the first-choice modality for this, it can provide a third alternative when echocardiography and CMR are inconclusive or contra-indicated [ ].
12.2
Echocardiographic approach to the LV contractility
During a cardiac cycle, the LV wall shortens, thickens, and twists along the long axis. Shortening and thickening can be quantified by measuring regional strains. Strain or myocardial deformation from developing forces is expressed as either the fractional or the percent change from the original dimension [ , ]. Positive radial strains represent wall thickening (radial deformation), whereas negative strains represent segment shortening (e.g., circumferential shortening, longitudinal shortening, and fiber shortening) [ ].
Three perpendicular axes orienting the global geometry of the LV define the local cardiac coordinate system: radial, circumferential, and longitudinal.
Echocardiographic techniques like tissue Doppler imaging have excellent temporal resolution (± 4 ms) and could be used for the assessment of myocardial deformations [ ] (see Chapter 2 ).
The base and apex of the LV rotate in opposite directions. Twist defines the base to apex gradient in the rotation angle along the longitudinal axis of the LV and is expressed in degrees per centimeter [ , ]. Torsion and twist are equivalent terms. Torsion can also be expressed as the axial gradient in the rotation angle multiplied by the average of the outer radii in apical and basal cross-sectional planes, thereby representing the shear deformation angle on the epicardial surface (unit degrees or radians) [ ]. This normalization can be used as a method for comparing torsion for different sizes of LV. When the apex-to-base difference in LV rotation is not normalized, the absolute difference (also in degrees or radians) is stated as the net LV twist angle [ ].
Speckle-tracking echocardiography (STE) has emerged as an alternative technique [ ] (see Chapter 2 ). The robustness and the clinical applicability of that technique are nowadays only validated for the assessment of global longitudinal strain [ , ]. When considering regional longitudinal strains, there are inaccuracies according to the software used. Longitudinal LV mechanics, which are predominantly governed by the subendocardial region, are the most vulnerable component of LV mechanics and therefore most sensitive to the presence of myocardial disease. The first of them is the ischemic etiology that will affect first the subendocardium. The mid-myocardial and epicardial function may remain relatively unaffected or weakly affect in patients with HF and preserved LV EF. Circumferential strain and twist may remain normal or show exaggerated compensation for preserving LV systolic performance. Increase in cardiac muscle stiffness, however, may cause progressive delay in LV untwisting. Loss of early diastolic longitudinal relaxation and delayed untwisting attenuate LV diastolic performance, producing elevation in LV filling pressures and a phase of predominant diastolic dysfunction, although the LV EF may remain normal. The diagnostic of these HF with preserved ejection that most affect the subendocardium could be very difficult and might require submaximal exercise stress echocardiographies [ ]. It has not been proposed in past recommendation, but that could change [ ].
On the other hand, an acute transmural insult (like a myocardial infarction) or progression of disease results in concomitant mid-myocardial and subepicardial dysfunction, leading to a reduction in LV circumferential and twist mechanics and a reduction in LV EF. Assessment of myocardial function, therefore, can be tailored per the clinical goals. The detection of altered longitudinal function alone may suffice if the overall goal of analysis is to detect the presence of early myocardial disease. Further characterization of radial strains, circumferential strains, and torsional function provides assessment of the transmural disease burden and provides pathophysiologic insight into the mechanism of LV dysfunction [ ]. For instance, the pathophysiologic process such as radiation that affects both the pericardium and the subendocardial region may produce attenuation of both longitudinal (first) and circumferential (afterwards) LV function [ ]. Several studies have reported the strain values in patients with systolic HF ( Table 12.1 ), HF with preserved LV EF, and hypertrophied cardiomyopathies. The data proposed in Table 12.1 are rather convergent; however, these measurements of LV systolic longitudinal strains are not used or proposed in guidelines such as in those for HF with preserved LV EF.
| Study | n | Population | End-point | Follow-up duration | GLS prognostic value | LV EF in the population (month) |
|---|---|---|---|---|---|---|
| Bertini et al. [ ] | 1060 | Ischemic cardiomyopathies | Death, cardiovascular hospitalization | 31 months | − 11.5% | Median = 34(25–58) |
| Mignot et al. [ ] | 147 | Heart failure | idem | > 12-months | − 7% | Mean = 29.9 ± 8.9 |
| Donal et al. [ ] | 140 | Heart failure | idem | 38 months | − 8% | Mean = 30 ± 9% |
| Nahum et al. [ ] | 125 | Heart failure | idem | 8.8 ± 6 | − 9% | Mean = 31 ± 10% |
| Lacoviello et al. [ ] | 308 | Heart failure | et idem + maligant arrhythmias | 26 ± 13 | ||
| Cho et al. [ ] | 201 | Heart failure | Cardiac death + cardiovascular hospitalization | 39 ± 17 | Not available − 10.7% for mean circumferential strain | Mean = 34 ± 13% |
As a rule of thumb, a global longitudinal strain less than − 17% is an independent parameter of severity of the cardiomyopathy [ ]. In HF with preserved LV EF, the prognostic cut-off that is most frequently reported is − 16% [ ].
In more complex cardiomyopathies like those induced by anthracyclins, it seems that as soon as the global longitudinal strain is less than − 19%, physicians have to carefully monitor the patients. Studies are ongoing to know whether dedicated treatments like ACE-inhibitor and B-blockers should be introduced [ ].
Although strain data are valuable in patients with systolic HF, the indication for an ICD or a biventricular pace maker remains dependent upon the degree of LV dysfunction as determined by the LV EF ( Figures 12.1 and 12.2 ). The LV EF should be measured, according to recommendations using the apical four- and two-chamber views using the Simpson method. The M mode should not be used especially in hearts having a spherical remodeling.


In the present and even more in the very near future, real-time 3D echocardiography (RT3DE) should improve the robustness and reproducibility of the echo data [ ]. It is not yet available everywhere (see Chapter 2 ). Still, improvements in transducer are required for the actual transfer of the 3D approach in clinical practice. Feasibility remains lower than for the 2D approach [ , ]. It has been demonstrated that in patients in whom serial examinations are obtained, the 3D echocardiographic approach is the most reliable [ , ].
Other approaches are available ( Figures 12.1–12.4 ) [ , ]. Pulse tissue Doppler is the most relevant and is a way for assessing LV longitudinal systolic function as well as MAPSE.


In addition to these measurements (LV EF required, global longitudinal strain, or pulse tissue Doppler), one must measure the LV stroke volume (Doppler and volumetric approaches) for estimating the cardiac output and finally the efficacy of this LV contractility to eject enough blood in the arterial tree ( Figure 12.5 ).

Also, as already mentioned, stress tests might be required to look for contractile reserve, in particular. Without going into much detail in regard to the technique, dobutamine could be used, but submaximal exercise stress echocardiography is probably the ideal approach to test the systolic response and the diastolic response of the failing heart. In HF with preserved ejection, the absence of systolic and diastolic reserve has already been mentioned. In ischemic heart disease, it has to be tested; sometimes, one is “surprised” to observe that without any acute ischemia, the exercise unmasks a dynamic functional mitral regurgitation that might be very useful for understanding the symptoms and is perhaps the best treatment of a patient with systolic HF [ ].
In addition to the assessment of viability or contractile reserve, it might be necessary to look for myocardial ischemia. The techniques are the same as in a non-failing heart, being nevertheless aware of the risk of maximal dobutamine stress test in patients with a failing heart (risk of ventricular arrhythmia, in particular).
12.3
Assessment of RV function
Until recently, the function of the RV in HF has been mostly ignored. A 2006 report of the National Heart, Lung, and Blood Institute identified a gap between RV research efforts that is far from being filled [ ]. Historically, the concept of a secondary role of the RV in circulation has been supported by the experimental evidence that ablation of the RV was not associated with significant alteration in systemic circulation or venous pressure [ ]. This evidence seemed cemented by the introduction of the Fontan procedure for complex congenital heart disease in 1968, a technique that directly connects the right atrium to the pulmonary artery, thus “bypassing” the RV [ ]. In spite of this fact, RV dysfunction is associated with increased morbidity and mortality in HF [ ] and in various heart diseases, such as myocardial infarction [ ], pulmonary arterial hypertension (PAH) [ ], and cardiac surgery [ ] after heart transplantation [ ] or LV-assisted device implantation [ ]. It is important to underline that the evaluation of RV function has often been limited to the estimation of pulmonary artery pressure (PAP). Actually, even if PAH and RV dysfunction are often joined, a normal RV function may coexist with increased PAP, even if the occurrence of RV is associated with a poor prognosis.
12.3.1
Anatomical and myofibers architecture
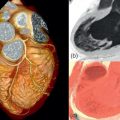
In the normal heart, the RV is the most anteriorly situated cardiac chamber and lies immediately behind the sternum. With respect to the LV, where the mitral and aortic valve are in continuity, one with the other, in the RV, a ventriculo-infundibular fold separates the tricuspid and the pulmonary valve, distinguishing the RV inlet from the RV outflow tract and determining the complex anatomy of the RV. Actually, the RV appears triangular in the sagittal plane and crescent shaped in cross section ( Figure 12.5 ). RV shape, as far as RV function, is also influenced by the position of the interventricular septum. Under normal loading and electrical conditions, the septum is concave toward the LV in both systole and diastole, but left deviation of the septum may occur in condition of RV pressure and volume overload, leading to alteration of both RV and LV functions. As far as the architecture of myofibril is concerned, the RV wall is composed of two muscle layers. The superficial fibers are arranged more or less circumferentially in a direction that is parallel to the atrioventricular (AV), while the deep layer is characterized by longitudinally oriented fibers [ ] and is responsible for the essentially longitudinal contraction of the RV.
12.3.2
RV function physiology
The alteration in RV function in pathological condition can be explained by looking at the particular physiology of this cardiac chamber. During fetal life, the RV provides blood to the lower body and placenta, supplying only a modest amount of blood to the lungs and thus working as a “systemic ventricle.” After birth, the primary function of the RV is to receive systemic venous return and to pump it into the pulmonary arteries. The reduction in pulmonary vascular resistance transforms RV physiology and morphology, and the RV becomes a low-pressure chamber [ , ] connected in series with the LV and pumping on average the same effective stroke volume.
Several differences exist between LV and RV contraction. Because of its myocardial structure and its bullet shape, LV contraction is due to a concentric contraction of the walls associated to a twisting motion of the heart. RV contracts by three separate mechanisms: inward movement of the free wall, which produces a bellows effect; contraction of the longitudinal fibers, which shortens the long axis; and traction on the free wall at the points of attachment, secondary to LV contraction. Interestingly, because of the greater surface to volume ratio of the RV, a greater EF is produced by a small change in surface area. This means that shortening of the RV is greater in longitude than in radius, and that a smaller inward motion of the lateral wall is required to equal LV stroke volume [ ]. The low impedance pulmonary circulation explains the very brief isovolumic contraction time of the RV and allows the RV to eject the blood into the pulmonary artery even after the onset of RV relaxation. This late ejection, or “hangout period,” explains the triangular-shaped RV pressure-volume loop [ ] and makes the identification of RV end-systole difficult.
The reduced mass and wall stress of the RV cause the RV to have a lower oxygen demand with respect to the LV. Moreover, in the LV, myocardial perfusion occurs predominantly in diastole when intramyocardial tissue pressure falls below aortic root pressure. Because of an intramyocardial tissue pressure that is below aortic root pressure throughout the cardiac cycle, coronary blood supply to the RV is continuous in the condition of normal afterload. Because of its particular physiology, changes in afterload and preload strongly affect RV morphology and function, leading to RV dilatation, reduced performance, and failure.
12.3.2.1
Response of the right ventricle to chronically increased volume
RV volume overload due to interatrial shunts or tricuspid or pulmonic regurgitation is normally well tolerated, and evident in patients with volume overload due to congenital heart disease [ ]. Initially, chronic volume overload causes RV dilatation and does not appear to impair contractile function that is preserved according to the Frank–Starling law. At a later stage, volume overload induces significant regional overexpression of growth factors like angiotensin II, insulin-like growth factor-I, and endothelin-1, with a corresponding increase of myocyte diameter and length and collagen deposition [ ]. The development of RV fibrosis is detrimental because it has been associated with an adverse clinical outcome in patients with congenital heart disease. This vicious cycle of collagen deposition and RV dilatation is associated with a rise in RV pressure [ ] and with an impairment in further increase in volume, either due to pericardial constraint or because of the shared architecture of the RV and LV. In this phase, additional increments in RV volume recruit minimal increments in RV free wall surface area and causes flattening and then bulging of the interventricular septum toward the LV, with development of biventricular failure.
12.3.2.2
Response of the right ventricle to acutely increased afterload
Being a “low-pressure” chamber, even small changes in afterload can reduce RV contractile performance and lower cardiac output, as evident in the setting of acute pulmonary embolism or acute lung failure. The RV cannot tolerate an acute increase in pulmonary pressure above 40–60 mmHg. As firstly described by Guyton et al. in 1954, a rapid increase in afterload induces a rise in RV contractility mediated by an homeomeric auto-regulation of the Anrep effect and by the release of endogenous catecholamines [ ]. With further increase in afterload, the RV begins to dilate and recruit function via the Frank–Starling mechanism. In this condition, the thin RV free wall experiences a rise in wall tension with increments in RV pressure. Moreover, the prevalent longitudinal contraction of the RV causes an increase in RV radius during systole ( Figure 12.6 ) that causes a shape-dependent increase in wall stress according to the Laplace law [ ], contributing to RV ischaemia and RV failure. Once all the mechanisms of contractile reserve are exhausted, systemic pressure begins to fall, causing a sudden catastrophic hemodynamic collapse.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree