Key Points
- ▪
Contrast enhancement is crucial to optimal CT angiography and to most applications of cardiovascular CT.
- ▪
Synchronizing contrast delivery to image acquisition for CT angiography requires that the contrast be present within the left heart and aorta but diminished or diluted within the right heart cavities by a part-saline/part-contrast bolus.
- ▪
For dissection protocols and pulmonary embolism protocols, no saline “chaser” is needed.
- ▪
Few good alternatives to iodinated contrast are currently available.
- ▪
Pre-contrast images are useful to:
- ▪
Identify vascular calcification
- ▪
Identify acute intramural hematoma
- ▪
- ▪
Delayed (30- to 120-second) images are useful to characterize:
- ▪
The filling of the left atrial appendage
- ▪
The false lumen of a chronic aortic dissection
- ▪
- ▪
Contrast enhancement is essential for all forms of cardiovascular CT other than:
- ▪
Calcium scoring
- ▪
Identification of:
- •
Pericardial or other calcification
- •
Intramural hematomas of the aorta
- •
Intramyocardial fat
- •
- ▪
Cardiac tumor assessment
- ▪
Optimal Enhancement
Vascular and cardiac blood pool contrast enhancement is determined by the interaction of iodine administration and blood flow. The goals of contrast administration are:
- □
Adequate opacification of cavities and vessel lumen
- □
Avoidance of both under- and over-opacification. It is important to recognize that excessive contrast concentration generates high attenuation artifact.
- •
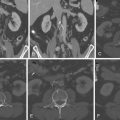
Starburst high-attenuation artifacts from the superior vena cava (SVC) are among the most common of all annoying and frustrating artifacts.
- •
CT angiography (CTA) requires high left heart/aortic contrast and low right heart contrast (high right heart opacification confounds assessment of the right coronary artery and the right ventricular contours).
- •
- □
Optimal enhancement depends on the purposes of the study.
- •
The optimum contrast effect for vascular enhancement is 300 to 500 HU.
- •
The optimal contrast effect for coronary plaque characterization is less: 250 to 350 HU.
- •
- □
Optimal opacification requires a near-steady level of contrast throughout the entire duration of the study.
- □
Synchronization of opacification to image acquisition phase is crucial. For CTA, the principal challenge is to synchronize these three variables:
- •
The arrival of the contrast medium in the left heart
- •
Washout from the right heart with the saline push
- •
Acquisition phase
- •
Acquisition Time and Contrast Need
As scanners are developed that can use larger numbers of slices and provide greater breadth of scanning, acquisition time is falling, as is the needed duration of contrast effect, and, therefore, the volume of contrast needed. In comparison to 10-slice scanners, 64-slice scanners need only half the volume of contrast. In comparison to 16-slice scanners, 64-slice scanners need one third less contrast.
Factors That Increase the Amount of Contrast Needed
- □
Larger field of view: e.g., post-aortocoronary bypass studies where the field of view along the Z-axis is from the subclavian arteries to the base of the heart (to visualize internal thoracic arteries as well as the heart)
- □
Slower (fewer detectors) scanners
- □
Lesser pitch
Factors That Reduce the Amount of Contrast Needed
- □
Faster (more detectors) scanners
- □
Smaller scan length
- □
Greater pitch
Issues of Practicality
- □
A robust protocol is wiser than an ambitious protocol.
- □
A dual-head injector is preferable (for contrast and for saline).
- □
The greater the kV, the greater the penetration and the lesser the contrast effect.
Injection
- □
Site
- •
Right antecubital vein. Use of the left antecubital vein is likely to result in high-attenuation artifact in the left subclavian vein, which may “bloom” or generate streak artifacts that cross the left subclavian artery/internal thoracic/mammary artery ostium and obscure it.
- •
Hand veins should be avoided.
- •
Central lines, unless labeled for IV injection, should be avoided.
- •
- □
Size
- •
A short 20-gauge IV catheter may be used for smaller patients.
- •
An 18-gauge IV catheter is more appropriate for larger patients.
- •
Dilute Contrast “Chaser”
It is becoming increasingly common to follow the contrast bolus with a “chaser” of dilute contrast (20–30% contrast with 70–80% saline) of the same volume as the injected saline so that there is diminished right heart cavitary attenuation but a smoother rendering of the blood-pool attenuation.
Saline “Chaser”
Otherwise, the same volume (as the contrast volume) of saline typically is injected to avoid excess concentration of contrast within the right heart chambers so that the right coronary artery imaging is devoid of high-attenuation artifacts arising from the right heart chambers.
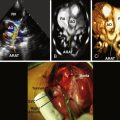
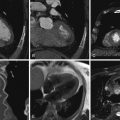
Occasionally, small bubbles of air from the IV tubing can be seen within the right heart. These are generally inconsequential; however, if there is a history of congenital heart disease or suspicion of Eisenmenger syndrome physiology, an IV air bubble filter should be used. Because this may decrease the overall rate of contrast injection (approximately 3 mL/sec), administration of a larger volume of contrast or dual injection into both arms should be considered ( Figs. 4-1 and 4-2 ).


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree