- •
Define the most common and clinically significant coronary anomalies.
- •
Define common types of coronary fistulae.
- •
Define which coronary anomalies are low versus high risk.
- •
Outline the advantages of cardiovascular magnetic resonance (CMR) imaging over conventional X-ray angiography.
- •
Understand treatment options for common coronary anomalies.
Coronary anomalies are a rare group of congenital disorders with an incidence of approximately 0.6 percent of births. These can broadly be defined as anomalies of origin and course, termination, or intrinsic anatomy ( Table 24-1 ). Patients may be asymptomatic or present with angina, palpitations, or exertional syncope. Although most have a benign course, these conditions can cause sudden cardiac death and myocardial infarction—especially in young adults and athletes. Diagnosis is highly dependent on cardiac imaging. Traditionally, X-ray coronary angiography was used to make the diagnosis. Currently CMR has emerged as a noninvasive method for defining the origin of coronary arteries and their three-dimensional proximal course, without radiation exposure or contrast administration. This makes CMR an ideal choice for young adults with suspected coronary anomaly. Treatment highly depends on the type of anomaly. For those associated with an interarterial course and/or myocardial ischemia, surgical correction is warranted.
|
|
|
|
ANOMALIES OF ORIGIN AND COURSE: HIGH RISK
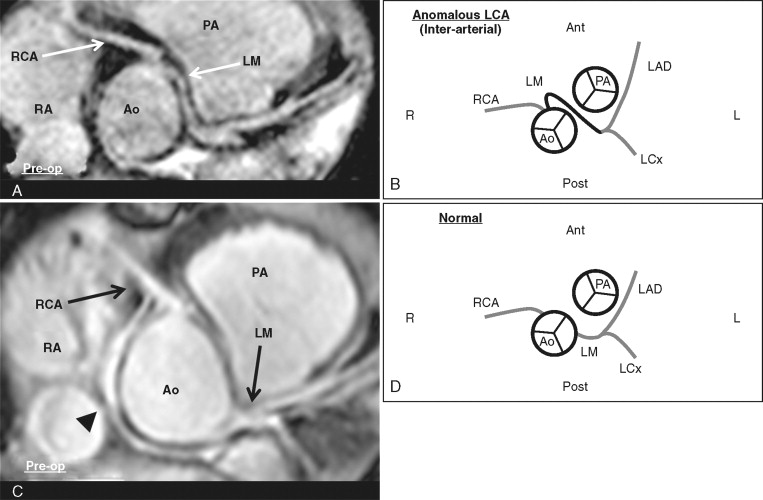
A 13-year-old boy presented with exertional syncope. CMR was ordered to assess for coronary anomaly. Based on the high-risk anatomy, the patient underwent successful surgery with reimplantation of the LM to the correct sinus ( Figure 24-1 ).
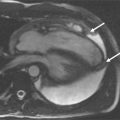
An 18-year-old man presented initially with exertional chest tightness and fatigue while playing basketball. A chest X-ray showed cardiomegaly, and an ECG showed nonspecific ST-T wave abnormalities. A transthoracic echocardiogram revealed moderate LV enlargement, a left ventricle ejection fraction (LVEF) of 35% with global hypokinesis, moderate to severe MR, and severe pulmonary HTN estimated at 100 mm Hg. An exercise myocardial perfusion stress test showed an infarct with severe peri-infarct ischemia in the distal anterior and inferolateral walls at 15 METs of exercise. X-ray coronary angiography revealed an anomalous left coronary artery (LCA) originating from the pulmonary artery (PA) and a large right coronary artery (RCA) providing collaterals to the LCA. He was referred for CMR to better delineate the coronary anomaly and to assess myocardial scar ( Figure 24-2 ). Based on the findings on CMR, he was referred for cardiac surgery where a LIMA graft to the LAD was placed as well as an annuloplasty ring to the mitral valve. His symptoms improved after surgery.