Case presentation
A 13-year-old is brought to the Emergency Department after being struck by a large truck while attempting to cross a highway on his bicycle. There is no reported loss of consciousness. His vital signs show an afebrile patient with a heart rate of 120 beats per minute, respiratory rate of 28 breaths per minute, blood pressure of 100/70 mm Hg, and a pulse oximetry reading of 91% on room air. He is conversing on arrival and has bruising over the lower medial right side of his neck and upper- and mid-chest, bilaterally. He states his right collar bone hurts and he has bilateral chest pain, left more than the right, while taking deep breaths. There is no crepitus. He has some mild abdominal pain to the left upper quadrant. He also has an obvious deformity to his left lower extremity but is neurovascularly intact. His Glasgow Coma Scale score is 14.
Imaging considerations
Plain radiography
Plain radiographs are the most common imaging modality utilized to diagnose pediatric pulmonary trauma and should be obtained on every child when pulmonary contusion is suspected and in general on all seriously injured children. When compared to advanced imaging such as computed tomography (CT), plain radiographs are the most appropriate first-line imaging modality to identify clinically significant pulmonary contusions, although plain radiography may underestimate the size of the injury. , Localized patchy opacities in nonanatomic distributions in the area of impact are the most frequently found abnormality when pulmonary contusions are present. Although radiographs obtained shortly after trauma may be negative for signs of pulmonary contusion, they may show other abnormal findings such as pneumothoraces or rib fractures, which will make contusions more likely. It is not necessary to repeat radiographs if they are initially negative unless the child’s respiratory status worsens. ,
Thoracic ultrasound (US)
US can be used to evaluate the pediatric lungs, although the findings associated with pulmonary contusions are nonspecific and should be interpreted by a skilled practitioner. Findings include what are commonly referred to as “B lines,” which indicate interstitial edema, with an equivalent significance as Kerley B lines found on chest radiographs. Dynamic air bronchograms also may be seen, similar to pneumonia, due to parenchymal consolidation, but with dynamic movement of air in the patent bronchi. Clinical context needs to be applied to differentiate B lines secondary to contusion versus other causes of sonographic B lines such as pulmonary edema or pneumonia.
Computed tomography
CT provides greater detail than either US or plain radiography; however, CT is not recommended for the sole purpose of diagnosing pulmonary contusion. Pulmonary contusions appear as patchy localized opacities on CT. CT scans are more sensitive for the detection of pulmonary contusion than plain radiographs are, but this does not necessarily correlate with the patient symptoms or degree of injury. Small contusions may only be apparent on CT.
Imaging findings
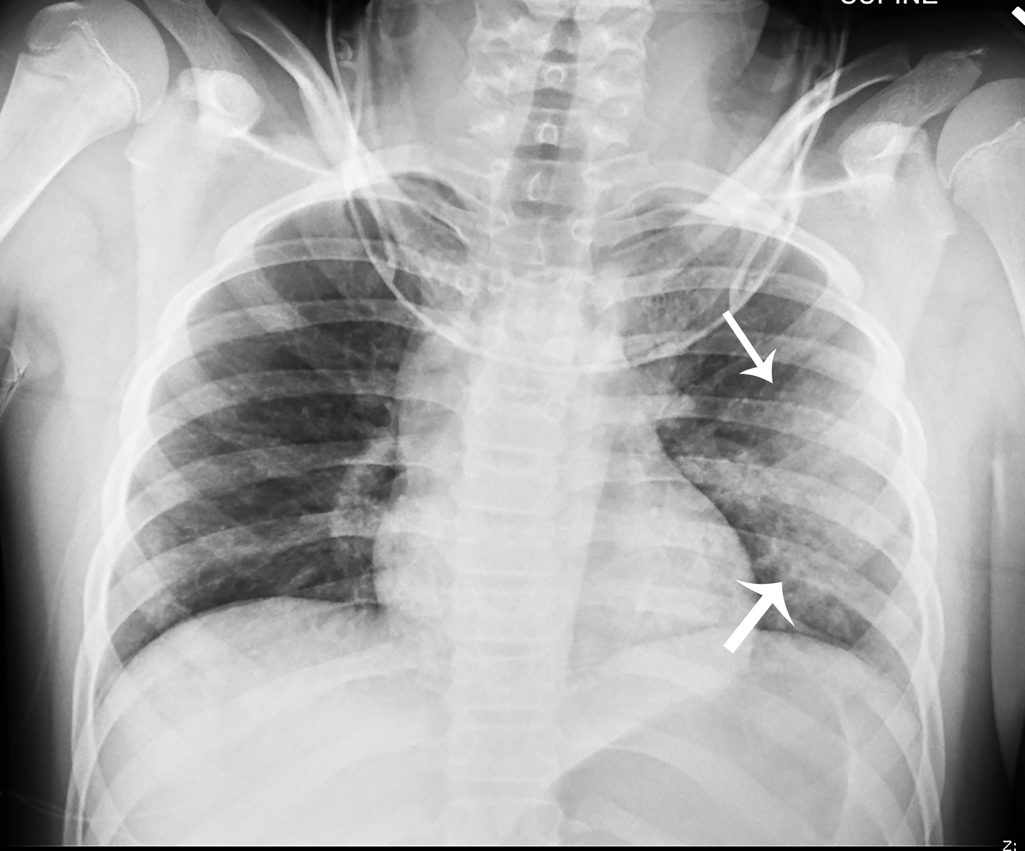
An initial, one-view chest radiograph was obtained. The image demonstrates abnormal lung opacities, left greater than right, suggestive of pulmonary contusion on the left. The opacity in the right lower lobe, predominantly retrocardiac, is thought more likely to represent atelectasis ( Fig. 45.1 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree